eISSN: 2471-0016


Research Article Volume 3 Issue 1
1Department of Pathology, ACPM Medical College, India
1Department of Pathology, ACPM Medical College, India
2Department of Public Health Dentistry, ACPM Dental College and Hospital, India
2Department of Public Health Dentistry, ACPM Dental College and Hospital, India
3Department of Urology, ACPM Medical College, India
3Department of Urology, ACPM Medical College, India
Correspondence: Rajeshwari K, Assistant Professor, Department of Pathology ACPM Medical College, Dhule,Maharashtra, India, # 8 staff quarters
Received: January 01, 1971 | Published: October 21, 2016
Citation: Dravid NV, Rajeshwari K, Karibasappa GN,et al. Histomorphological profile of lesions in cystoscopic bladder biopsies - a prospective study in North Maharashtra. Int Clin Pathol J. 2016;3(1):161–166. DOI: 10.15406/icpjl.2016.03.00064
Introduction: Urinary bladder lesions constitute an important source of clinical signs and symptoms which are more disabling than lethal. The present study aimed to study the frequency of bladder lesions and to study the clinico-histomorphological features of various bladder lesions with special emphasis on grading and staging of the bladder tumours.
Materials and methods: The present study is a 3 years prospective study carried out in the department of pathology. All patients who visited to urology outpatient department with lower urinary tract symptoms and obstructive bladder symptoms were subjected to cystoscopy. The detailed clinico-histomorphological features of cystoscopy biopsies are studied using WHO/ISUP 2004 histological grading and TNM staging are used in classifying the bladder tumours.
Results: Out of 139 cystoscopy biopsies, the non-neoplastic bladder lesions constituted 26.6 % and neoplastic lesions constituted 73.38%. Among the neoplastic, benign lesions showed 10.79% of the cases and malignant lesions showed 62.58% of the cases. Among the malignant lesions, urothelial carcinoma was the commonest accounting for 55.39% of the cases with increased prevalence of high grade papillary urothelial carcinoma (55.43%) and invasive papillary urothelial carcinoma accounting for 78.25% of the cases.
Conclusions: The present study has stressed the importance of Histopathological examination with special emphasis on the study of serial sections, inclusion of smooth muscle in the biopsy for accurate grading and staging so as to decrease the mortality and morbidity due to bladder tumours.
Keywords: urothelial lesions, urothelial carcinoma, high grade, low grade
OPD, outpatient department; TURBT, transurethral resection of bladder tissue; LUTS, lower urinary tract symptoms; PUNLMP, papillary urothelial neoplasm of low grade malignant potential; PAS, periodic acid- schiff; JMS, jones’ methenamine siver stain; PEM, periodic acid-siver methenamine; GMS, gomori’s trichrome stain; MTS, massons trichrome stain; IHC, immunohistochemistry
In this modern era, there have been increased prevalence of bladder lesions including both neoplastic and non neoplastic lesions and have been contributed for significant disabling than lethal. Bladder tumours constitute one of the most common urologic condition and accounts for significant morbidity and mortality.1,2 It is the second most common neoplasm of genitourinary tract next to prostate and sixth most common cancer in the world wide.3 These neoplasms of bladder pose biologic, clinical, diagnostic and therapeutic challenges to both urologist and uropathologist, as these bladder tumours represent a heterogeneous group of tumours with different subtypes and behavioral patterns.4,5 As per the data of Indian cancer registry, it is the ninth most common cancer and accounts for 3.9% of all cancers.6 Since most of the bladder tumours are known for its recurrence, rapid progression to high grade and stage and it presents with various non-specific symptoms for which there is a need for accurate diagnostic tests. The significant diagnostic test includes cystoscopy, bladder biopsy and urine cytology for accurate diagnose, management and prognostic assessment of the patient.
Giving the importance of bladder lesions in genitor urinary pathology, the present study was undertaken to study the clinicopathological features of bladder lesions with special emphasis on grading and TNM staging, so as to prevent the mortality and morbidity associated with urinary bladder carcinoma.
The present study is a prospective type carried out in the department of pathology over a period of three years between June 2012 – June 2015 and included 139 cases in the study.
All the patients who visited the urology outpatient department (OPD) with lower urinary tract symptoms and obstructive urinary symptoms were included in the study. After the informed written consent of the patients, fiberoptic cystoscopy bladder biopsies were taken from the walls of the bladder. The cystoscopic bladder biopsies taken were fixed in 10% buffered formalin and then processed with embedding in paraffin wax. Four microns thick sections were taken and stained with regular haematoxylin and eosin stain (H and E). The study of biopsy specimens along with the histomorphological changes under low and high power magnification were studied by light microscope. The WHO/ISUP – 2004 grading system was used to grade the bladder neoplasms 7 and staging was done according to TNM staging.7
Inclusion criteria: All the transurethral resection of bladder tissue (TURBT) biopsies received in the department of pathology.
Exclusion criteria: Autolysed and inadequate biopsies were excluded.
Out of total 139 cases, 71cases (51.1%) were males and 68 cases (48.9%) were females with peak age incidence is between 60-69 years as shown in graph 1. In the study, we found that the majority of the patients with benign lesions presented with lower urinary tract symptoms (LUTS) accounting for 82.7% of the cases and those with malignant lesions present with haematuria accounting for 90.8% of the cases as shown in graph 2. The details of the histomorphological diagnosis of bladder lesions are given in table 1. In our study, we observed that majority of the bladder lesions were malignant constituting 62.58% (87 cases) of the cases, among them the most common we found was urothelial carcinoma followed by squamous cell carcinoma and adenocarcinoma constituting 55.39%, 5.03% and 2.15% respectively. As per histological grading WHO/ISUP (2004) used in the study we found high prevalence of high grade urothelial carcinoma followed by low grade urothelial carcinoma, urothelial papilloma and papillary urothelial neoplasm of low grade malignant potential (PUNLMP) accounting for 55.43%, 22.82%, 16.3% and 5.43% respectively as shown in table 2.
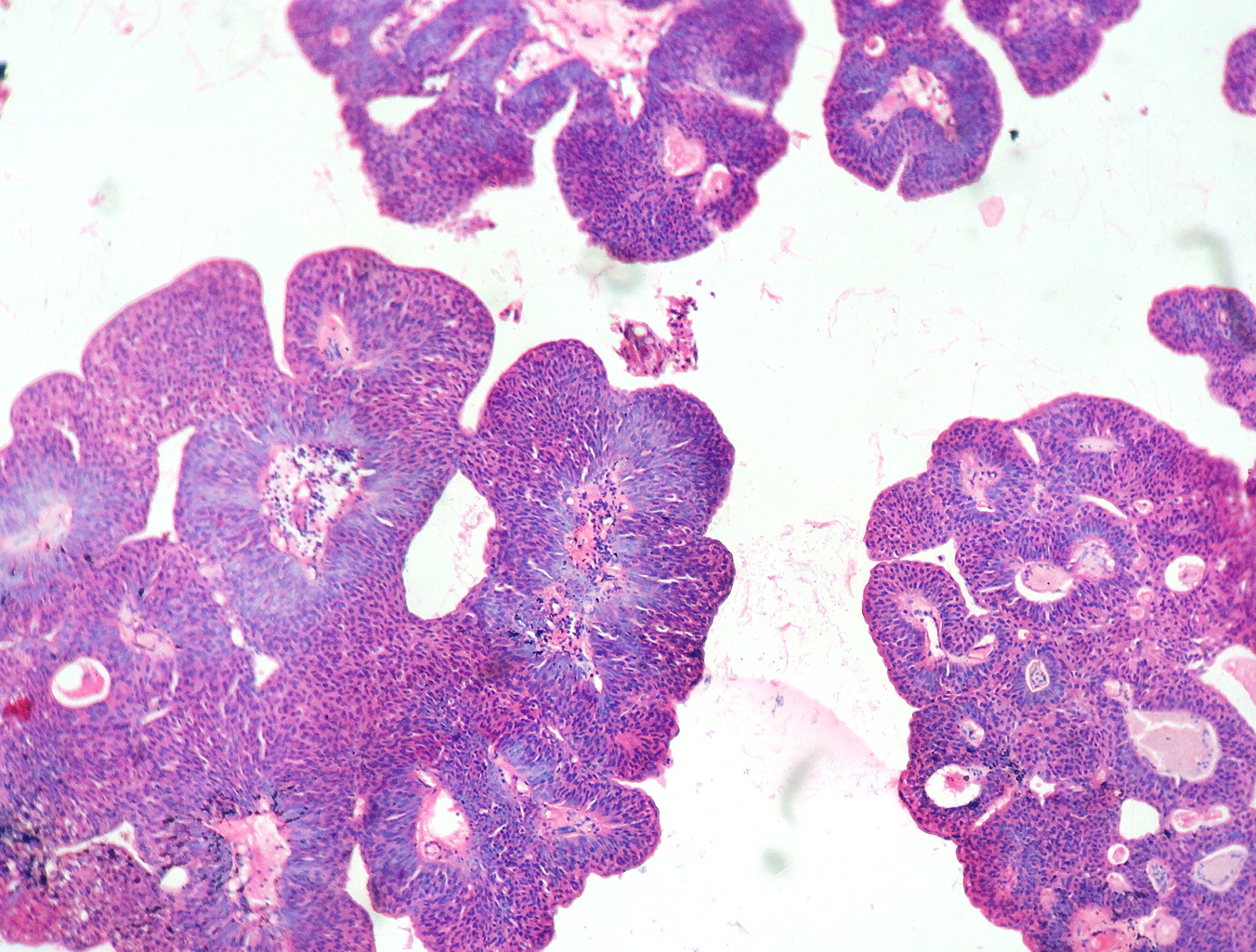
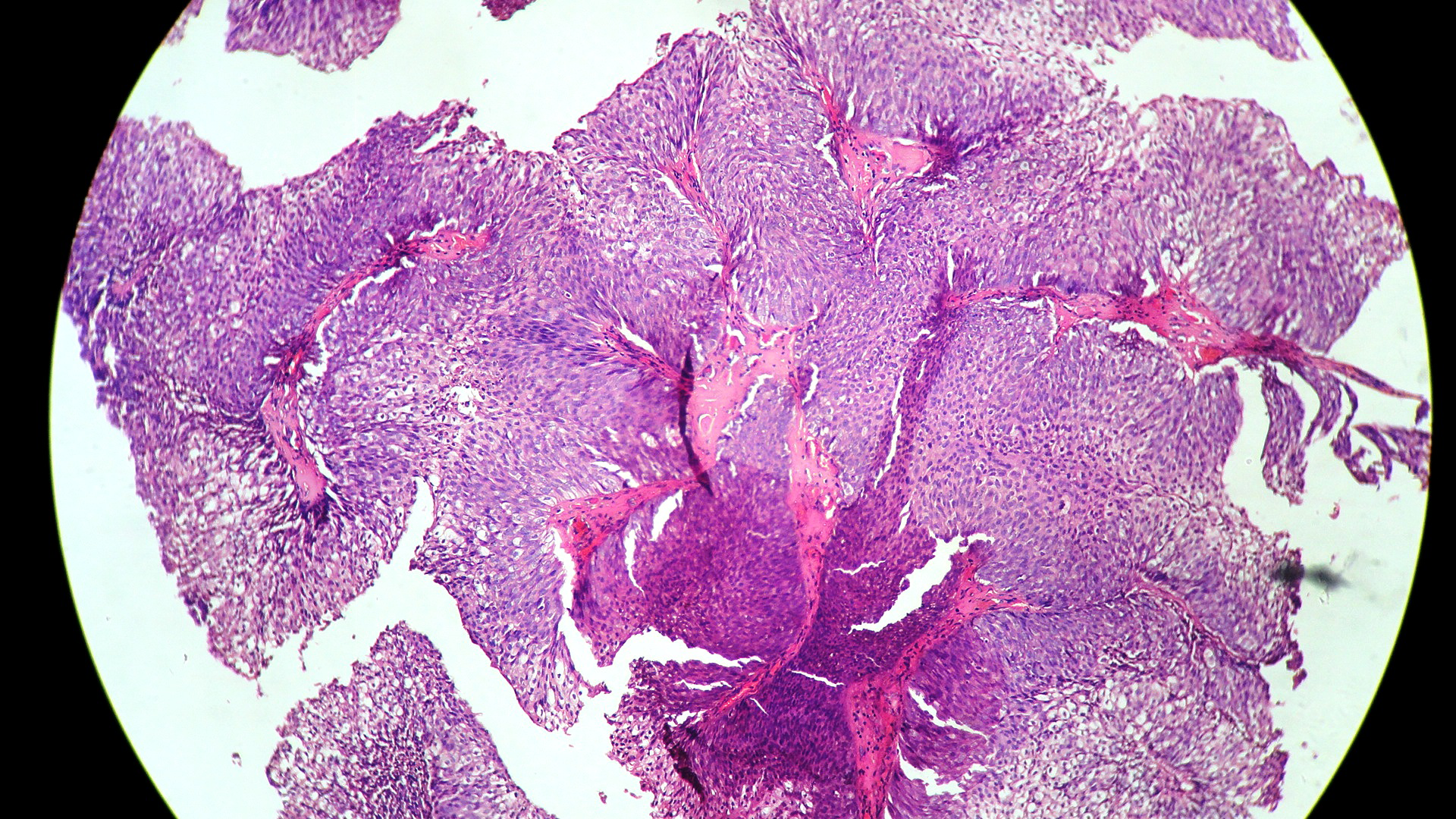
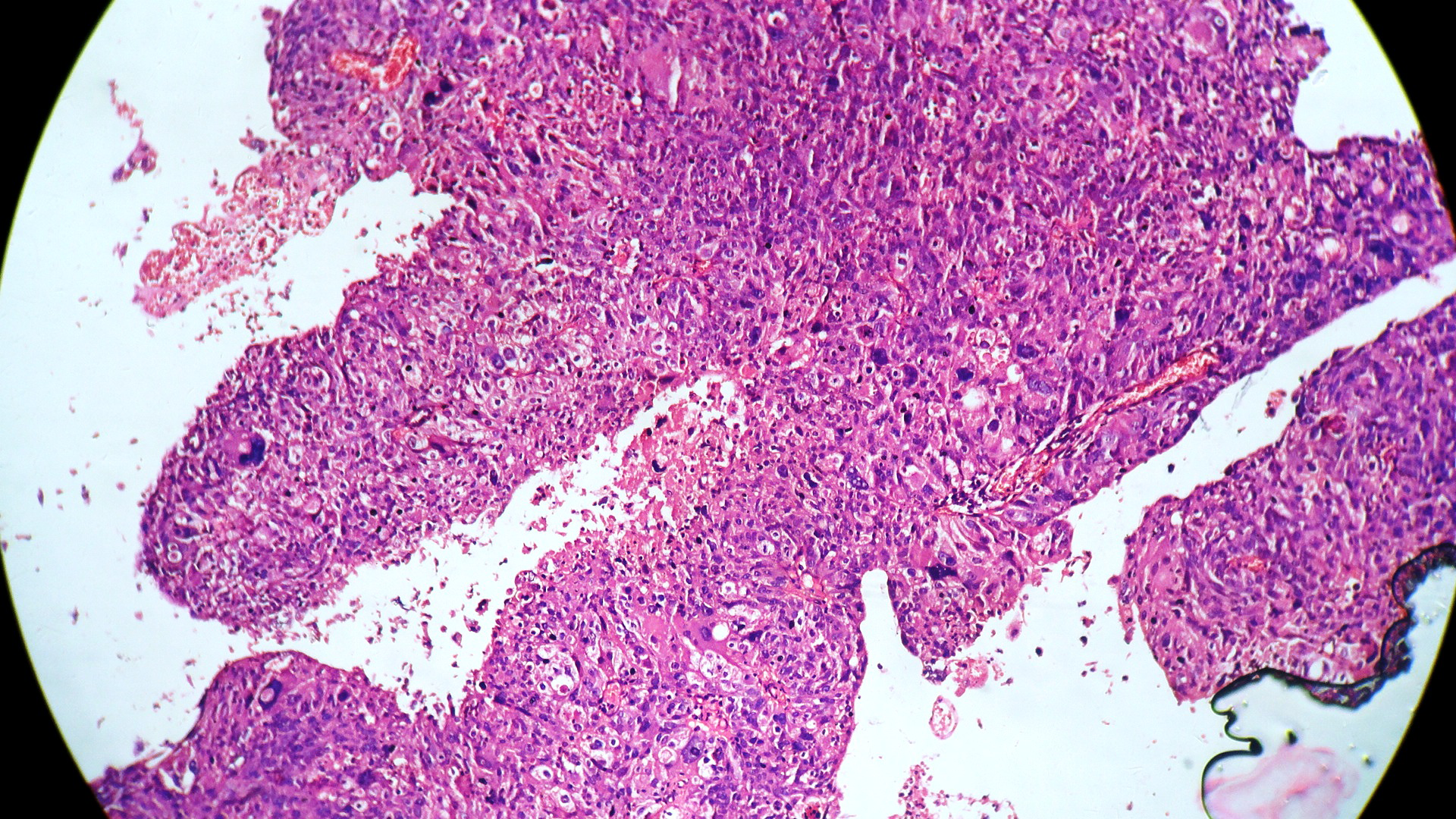
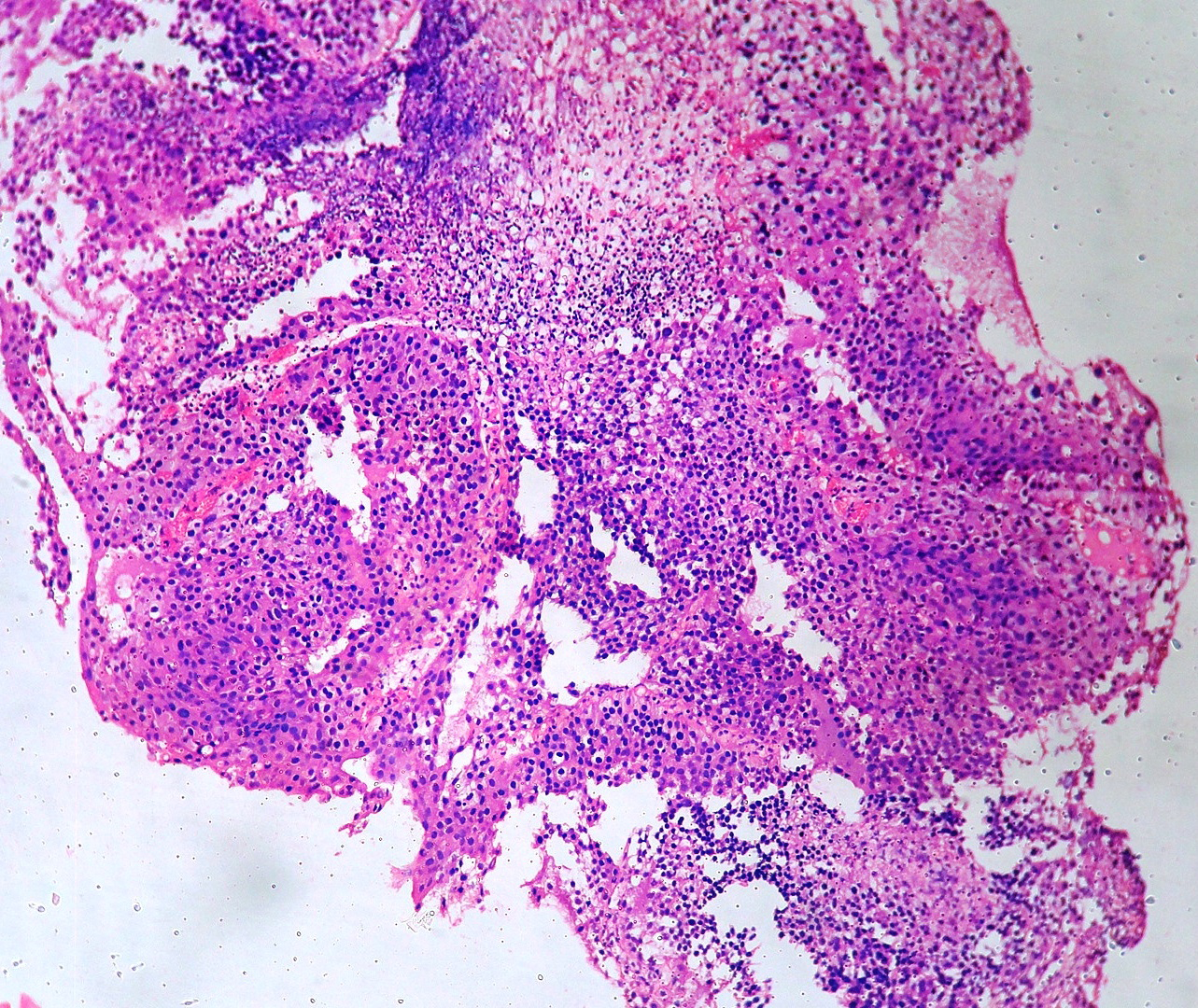
In our study, we made an attempt to evaluate the pattern of tumor growth, its degree of differentiation, progression and associated mucosal changes. In 15 cases of urothelial papilloma, it is characterized by discrete papillary growth with a central fibrovasular core lined by urothelium of normal thickness and cytology (Figure 1). In five cases of Papillary urothelial neoplasm of low grade malignant potential (PUNLMP), histopathologically the tumor is characterized by delicate, orderly, tenuous papillary structures with orderly arrangement of cells within the papillae with minimal architectural abnormalities and nuclear atypia usually limited to basal layer irrespective of cell thickness (Figure 2). The major distinction from papilloma is that in PUNLMP the urothelium is much thicker and nuclei are significantly enlarged. In 21 cases of low grade urothelial carcinoma, histologically it is characterized with papillary axes which are more compact, crowded, fused at the base and lined by unordered cells showing both architectural and cytological abnormalities with frequent mitosis (Figure 3). In 51 cases of high grade urothelial carcinoma showed fused papillary axes over the large areas resulting in sheets and solid areas. The cells have enlarged, hyperchromatic, pleomorphic nucleus in full thickness of the epithelium with increased atypical mitosis (Figure 4). As per TNM staging used in our study we observed majority of the bladder tumours were invasive accounting for 78.25% (Figure 5 & 6) as compared to non-invasive bladder tumours constituting 21.73% of the cases as shown in table 3.


Sl. No |
Histomorphological Diagnosis |
No. of Cases |
Percentage |
I |
Non neoplastic |
52 |
37.41% |
1. |
Non-specific cystitis |
18 |
12.94% |
2. |
Follicular cystitis |
6 |
4.31% |
3. |
Eosinophilic cystitis |
1 |
0.71% |
4. |
Cystitis glandularis |
2 |
1.43% |
5. |
Cystitis cystica |
1 |
0.71% |
6 |
Squamous metaplasia |
8 |
5.75% |
7 |
Tubercular cystitis |
1 |
0.71% |
II |
Neoplastic |
102 |
73.38% |
a. |
Benign |
|
|
|
Urothelial papilloma |
15 |
10.79 |
b. |
Malignant |
87 |
62.58% |
1. |
Urothelial carcinoma |
77 |
55.39% |
2. |
Squamous cell carcinoma |
7 |
5.03% |
3. |
Adenocarcinoma |
3 |
2.15% |
|
Total |
139 |
100% |
Table 1 Histomorphological Diagnosis Of Bladder Lesions.
Sl. No |
Grade |
No. of Cases |
Percentage |
1. |
Papilloma |
15 |
16.3% |
2. |
PUNLMP |
5 |
5.43% |
3. |
Low grade papillary urothelial carcinoma |
21 |
22.82% |
4. |
High grade papillary urothelial carcinoma |
51 |
55.43% |
|
Total |
92 |
100% |
Table 2 Histological Grading of Urothelial Neoplasm As Per Isup/Who 2004.
*PUNLMP – Papillary urothelial neoplasm of low grade malignant potential.
The present study is undertaken mainly to highlight the importance of histopathological examination in the diagnosis of bladder lesions. In recent days, the diagnosis and monitoring of bladder lesions are made by combination of cystoscopy, histopathology and urine cytology.8 All these diagnostic methods have its own limitations and cannot diagnose the presence of bladder tumours at every point of time.9 Advantages of cystoscopy are 1) helps in localizing the bladder tumours. 2) Detects low grade papillary lesions. Disadvantages are 1) Cystoscopy cannot visualize all the areas of bladder 2) Certain tumours like carcinoma insitu cannot be detected by cystoscopy. 3) It cannot comment on tumour grade and its depth of invasion.
Hence histopathology remains the gold standard method for diagnostic and therapeutic purpose. But it has its own limitations due to friability nature of bladder tumours, there may be technical impediments and interpretation errors like electro coagulation artifacts, retraction artifacts, exclusion of smooth muscle fibers from the mucosa pose difficulties in the histological grading and staging of the tumour. In such situations these limitations can be overcome by studying, multiple serial sections, by inclusion of smooth muscle during cystoscopic biopsy and by the usage of special stains to ensure accurate and definitive diagnosis.
Various special stains which includes histochemical and immunohistochemical stains are used
In the era of modernization, robust techniques like flow cytometry, chromosomal analysis, genomics, proteomics and immunohistochemistry (IHC) applications are used for an accurate classification and prognostication of bladder tumours.10 But these techniques are not routinely used due to lack of specificity, sensitivity and also due to exorbitant cost and inaccessibility to common people.
In our study, we have utilized all the three diagnostic modalities but emphasizing more on the Histopathological diagnosis with respect to histological grading and staging of bladder tumours. We selected, WHO/ISUP (2004) classification for histological grading in the present study due to its various advantages like 1) Uniform terminology and common definition used and accepted by various urological pathologist. 2) Well defined criteria for preneoplastic and neoplastic bladder tumours leading to greater inter-observer reproducibility. 3) Terminologies of WHO/ISUP (2004) classification and terminologies of urine cytology are similar facilitating better cyto-histologic correlation. 4) Prevents over or under diagnosis of urothelial tumours. 5) Identification of distinct group of patients with high grade papillary urothelial carcinoma and carcinoma insitu for intravesical therapy. 6) Removes ambiguity in diagnostic categories. 7). It mainly shows prognostically significant categories. 8) It also gives idea regarding the recurrence rate, progression grade and stage and survival rates between tumours of different categories of non-invasive papillary urothelial neoplasms of bladder as given in table 4.11
Sl. No |
Staging |
No. of Cases |
Percentage |
1. |
pTa (Confined to epithelium) |
20 |
21.73% |
2. |
pT1 (Invasion into lamina propria) |
49 |
53.26% |
3. |
pT2 (Invasion into superficial muscle) |
18 |
19.56% |
4. |
pT3 (Invasion into deep muscle) |
3 |
3.26% |
5. |
pT4 (Invasion into organs) |
2 |
2.17% |
|
Total |
92 |
100% |
Table 3 Staging Of Urothelial Neoplasm As Per Tnm Staging.
|
Papilloma |
Papillary Neoplasm of Low Grade Malignant Potential |
Low Grade Papillary Urothelial Carcinoma |
High Grade Papillary Urothelial Carcinoma |
Recurrence |
0-8% |
27-47% |
48-71% |
55-58% |
Grade progression |
2% |
11% |
7% |
Not applicable |
Stage progression |
0% |
0-4% |
2-12% |
27-61% |
Survival |
100% |
93-100% |
82-96% |
74-90% |
Table 4 Comparison of Recurrence Rate, Grade and Stage Progression And Survival Rates Of Non-Invasive Papillary Urothelial Neoplasms.
In our study we observed that bladder lesions are common between the age group of 60-69 years constituting 48.64% of the cases and is in concordance with Vaidya et al.12 and Matalka et al.11 The bladder lesions showed male preponderance than female accounting for 51.1% and 48.9% of the cases respectively. Our observations are in accordance with Lim et al.14 and Vaidya et al.12 The increased prevalence of bladder lesions in males observed in our study could be attributed to cigarette smoking, industrial exposure to acrylamine, schistosoma haematobium, cyclophosphamide, artificial sweetners and long acting analgesics. Various literatures state that the exact mechanism of inducing the cancer by these risk factors is unclear but a number of cytogenetic and molecular alterations are heterogenous.15
In the present study majority of the bladder lesions noted were malignant lesions accounting for 62.58% of the cases and correlated with the Vibhav KG et al study (96.87%) and Vaidya S et al study (77.57%).16,12 We have also observed that, among the malignant lesions of bladder most common was urothelial carcinoma followed by squamous cell carcinoma and adenocarcinoma accounting for 55.39%, 5.03% and 2.15% respectively and is in accordance with Mahesh K et al.17 and discordance with Mohammad M et al (93.3%) and Vibhav KG et al. (93%) [8,16] as shown in table 5.
We have found a wide spectrum of bladder lesions of which 26.6% of the cases accounted for non neoplastic lesions of bladder and 73.38% of the cases accounted for neoplastic lesions. This wide spectrum of bladder lesions in our study could be attributed to, free screening camps conducted by our centre. Our centre being one of the largest where free cystoscopic bladder biopsies were carried out in suspected patients presenting with obstructive and lower urinary tract symptoms.
Present study showed increased prevalence of high grade urothelial carcinoma accounting for 55.43% and is in concordance with Vibhav KG et al.16 and Vaidya S et al,12 Mahesh K et al.17 and Satya et al.18 as shown in table 6.
Our study showed increased prevalence of invasive urothelial carcinoma than non-invasive urothelial carcinoma and correlated with Christopher et al.11 and Vaidya et al.12 as shown in table 7. The increased prevalence of high grade urothelial carcinoma in our study may be due to lack of awareness among the people, low socio-economic status and poor hygienic practices among the patients have contributed for the same.
In our study the diagnosed cases of invasive urothelial carcinoma were treated surgically with radical cystectomy with urinary diversion. Preoperative radiotherapy and adjuvant chemotherapy was given for patients with localized disease in urothelial carcinoma. Patients with squamous cell carcinoma and adenocarcinoma were treated with radiotherapy. On follow–up patient doing well till the date of review of the case.
Neoplastic Lesions |
Mahesh K et al.17 |
Mohammad M et al.8 |
Vibhav KG et al.16 |
Present Study |
Urothelial carcinoma |
28(46.6%) |
467(93.3%) |
93(93%) |
77(53.39%) |
Squamous cell carcinoma |
2 (3.33%) |
13(2.6%) |
2(2%) |
7(5.03%) |
Adenocarcinoma |
2 (3.33%) |
10(2%) |
1(1%) |
3(2.15%) |
Table 5 Comparison of Prevalence of Various Neoplastic Lesionso Bladder in Different Studies.
Grading |
Laishram |
Mahesh K |
Vaidya |
Satya |
Vibhav KG et al.16 |
Present Study |
PUNLMP |
7.69% |
- |
10.28% |
- |
4.1% |
5.43% |
LGPUC |
53.85% |
42.85% |
29.91% |
25.0% |
32.29% |
22.82% |
HGPUC |
34.61% |
53.57% |
32.7% |
62.85% |
60.41% |
55.43% |
Table 6 Comparison of Prevalence of Different Histological Grades of Bladder Neoplasms in Various Studies.
*PUNLMP- Papillary urothelial neoplasm of low grade malignant potential;
*LGPUC- Low grade papillary urothelial carcinoma.
*HGPUC- High grade papillary urothelial carcinoma.
TNM Stage |
Christopher et al.19 |
Laishram et al.6 |
Vaidya et al.12 |
Present Study |
pTa |
23(33.3%) |
14(53.85%) |
39(48.14%) |
20(21.73%) |
pT1 |
15(20.0%) |
4(15.38%) |
18(22.22%) |
49(53.26%) |
pT2 |
8(10.7%) |
8(30.77%) |
24(29.63%) |
18(19.56%) |
pT3 |
9(12.0%) |
|
|
3(3.26%) |
pT4 |
14(18.7%) |
|
|
2(2.17%) |
Table 7 Comparison of Prevalence of Different Stages of Bladder Neoplasms in Various Studies.
We conclude that urinary bladder lesions are common in north Maharashtra. A high prevalence of 62.58% of the cases of bladder tumours is noted. The early and definitive diagnosis with accurate grading and staging of bladder tumours can be done by histopathology. The importance of including the smooth muscle in the biopsy, study of multiple serial sections and with usage of special stains needs to be emphasized in definitive diagnosis of bladder neoplasms. Attempts should also be made to create awareness among the public regarding the bladder symptoms so as to prevent mortality and morbidity faced by the people due to advanced bladder tumours.
None.
The author declares no conflict of interest.

©2016 Dravid, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.