eISSN: 2469-2778


Research Article Volume 8 Issue 2
1Department of Anesthesia, College of Medicine and Health Sciences, Bahir Dar University, Ethiopia
2Department of Anesthesia, College of Health Sciences, Addis Ababa University, Ethiopia
3Department of Biomedical Sciences, Medicine and Health Science College, Bahir Dar University, Ethiopia
Correspondence: Gebrehiwot Assfaw Tegu, Department of Anesthesia, College of Medicine and Health Sciences, Bahir Dar University, Ethiopia
Received: March 24, 2020 | Published: May 13, 2020
Citation: Tegu GA, Awol MA, Birhan MM. Blood requisition and transfusion practices for elective surgical procedures at Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia, 2017. Hematol Transfus Int J. 2020;8(2):42-45. DOI: 10.15406/htij.2020.08.00221
Background: For elective surgeries preoperative over ordering of blood is very common practice and leads to holding up of the blood bank reserve, aging of the blood unit, and wastage of blood bank resources. This can be decreased by simple means of changing the blood cross-match and ordering schedule depending upon the type of surgery performed.
Objectives: To assess blood requisition and transfusion practices in elective surgical procedures.
Methods: Hospital-based cross-sectional study was conducted from February 1, 2017, to March 31, 2017 G.C at Tikur Anbessa specialized Hospital. Using a convenient sampling technique and structured checklist, data was collected from elective surgical patients. Blood utilization was calculated using a cross-match to transfusion ratio (C/T), transfusion probability (%T) and transfusion index (TI), and the maximum surgical blood-ordering schedule (MSBOS) is formulated by Mead's criterion for common surgical procedures.
Results: Among 525 units of blood cross-matched blood, 107 units were transfused. Among all 242 elective surgical patients who had cross-matched blood, 55 (22.7%) patients were transfused with 107(20.4%) units of the prepared blood giving cross-match to transfusion ratio of 4.9, transfusion probability of 22.7% and transfusion index of 0.44.
Conclusion: The amount of blood requested and cross-matched for patients undergoing elective surgery is much greater than the amount actually used. Ordering pattern needs to be revised and over-ordering of blood should be minimized.
Keywords: blood transfusion, cross-match to transfusion ratio, transfusion probability, transfusion index
Blood transfusion no doubt plays a major role in the resuscitation and management of patients especially in surgical cases, but surgeons often overestimate the anticipated blood loss thereby over-ordering blood.1 Analysis of the data indicated that the majority (77%) of operations will need no pre-operative preparations of blood.2 The demand for a large quantity of preoperative cross-matching of blood for elective surgeries of which little is utilized causes wastage of valuable supplies and resources both in terms of technician time and reagents, not only that but also cross-matched blood is unavailable for others for 24 to 48 hours. During this time, 1 to 2 days is lost, and the chance for outdating increases. 3 Over ordering with minimal utilization, squanders technical time, reagent, and imposes extra expenses on patients and institutions.
Blood donation rates in Africa are generally very low (about 5 per 1000 population) compared with developed countries (47 per 1000 USA). Survey on blood safety and availability was collected by WHO from 40 of the 48 countries in sub-Saharan Africa indicated that 35 (87.5%) countries collect less than half of the blood needed to meet the transfusion requirements of their populations.4 The same is true in Ethiopia as the National Blood Bank disclosed in September 2015 around 87,000 units of blood were collected, although the country needs 200,000 annually.
Above all Africa is in desperate need of a significant scaling-up of efforts to make safe blood available to all patients, whose survival and wellbeing depend on this treatment intervention. It is technically feasible, lacking only the political commitment and financial resources.4
From the studies of the United States, Australia, and Israel great saving of blood and resources made from rationalizing blood-ordering habits. 5 That would require a cultural shift at all levels of the health system including clinicians, managers, and policymakers.6 In Ethiopia, hospitals lack not only institution-specific guidelines but also the magnitude of the problem was not investigated. This study aimed to assess blood requisition and transfusion practices in elective surgical procedures at Tikur Anbessa Specialized Hospital, from February 1, 2017, to March 31, 2017 GC.
Hospital-based descriptive study was carried out on 242 elective surgical patients at Tikur Anbessa Specialized Hospital from February 1, 2017, to March 31, 2017 G.C. Upon proposal development, logbooks of each surgical departments were reviewed for possible seasonal case flow variations and to determine the convenient data collection period to include the maximum possible number of cases. So from previous experience February to March found relatively highest surgical procedures performed. It might be because of the sociodemographic nature of the country that composed of more than 80% agrarian society that has seasonal health-seeking behavior mainly at the end of the harvesting season. All elective surgical patients during the study period were considered but patients with inadequate diagnosis, operative or transfusion details, and surgeries canceled were excluded from the study. Data was collected by a convenient sampling technique using a structured checklist. The data collection was undertaken by MSc anesthesia students who assigned at the respective operation room and the postoperative data collected by nurses at respective wards. Data collectors were trained; the pretest was done at each operation theatre and respective wards of Tikur Anbessa Specialized Hospital to test the data collection instruments. During data collection, regular supervision and follow up were made. Principal investigators cross-check for completeness and consistency of data every day.
Data were checked manually for completeness, coded, and entered into Epi Info version 7 and exported to SPSS version 20-computer program for cleaning, transformation, and analysis.
Statistical analysis was performed using SPSS version 20. Blood utilization indices were computed with the following equation:
Before the study, ethical clearance was obtained from the Departmental Research and Ethics Review Committee of Department of Anesthesia college of Health Sciences of Addis Ababa University, and acquiescence was also obtained from Tikur Anbessa specialized Hospital. Moreover, full clarification about the purpose of the study was made to the Authorized person of the health facilities. A formal letter of cooperation was obtained from Tikur Anbessa specialized Hospital. The purposes of the study were also explained to patients who were included in the study. Verbal consent from patients was asked and Confidentiality of the information was assured by using code numbers and keeping questionnaires locked.
Characteristics of surgical patients at TASH
Among a total of 242 patients, 153 were men and 89 were females (male to female ratio of 1.7:1). The age of patients ranges from 2 months to 80 years with an average age of 31.2 years. About 76% of patients were above 15 years old. Nearly half of patients are without underlining medical conditions scheduled only for surgical procedures that lie on ASA status I (Table 1).
Characteristics |
Frequency |
Percentage |
|
Sex |
Male |
153 |
63.2 |
Female |
89 |
36.8 |
|
Age |
<15 |
60 |
24.8 |
>15 |
182 |
75.2 |
|
ASA status |
I |
120 |
49.6 |
II |
101 |
41.7 |
|
III |
21 |
8.7 |
|
Type |
GA |
190 |
78.5 |
RA |
52 |
21.5 |
|
Table 1 Socio-demographic and clinical characteristics of surgical patients At Tikur Anbessa Specialized Hospital, from February 1, 2017, to March 31, 2017 GC
GA, general anesthesia ; RA, regional anesthesia
Blood requisition and utilization
Five hundred twenty-five blood units were cross-matched, 97% during preoperative, and 3% during the intraoperative period. One hundred seven (20.4%) units of blood were transfused giving an overall cross-match transfusion ratio of 4.9 (Figure 1). Of the 242 cases operated only 55 patients had been transfused with PRBC or whole blood which gives a transfusion probability (%T) of 22.7% and transfusion index of 0.44.
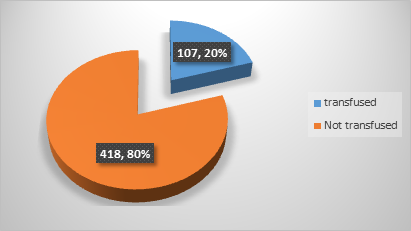
Figure 1 Comparison of units of blood cross-matched and transfused at Tikur Anbessa Specialized Hospital, from February 1, 2017 to March 31, 2017 GC.
Blood requisition and utilization in respective departments
Twenty six percent of the listed cases were from Orthopedics Department with a relatively good transfusion index of 0.5. From all departments neurosurgery was efficient with significant blood usage even if crossmatch to transfusion ratio is slightly higher than the seated criteria (Table 2).
Department |
Cases CM |
Cases TD |
Units CM |
Units TD |
C/T |
%T |
TI |
Cardiothoracic surgery |
28 |
4 |
73 |
9 |
8.1 |
14.3 |
0.3 |
General surgery |
25 |
5 |
65 |
10 |
6.5 |
20 |
0.4 |
Gynecology |
18 |
4 |
47 |
10 |
4.7 |
22.2 |
0.6 |
Neurosurgery |
31 |
14 |
89 |
29 |
3 |
45.2 |
0.9 |
Orthopedics |
64 |
17 |
121 |
29 |
4.2 |
26.6 |
0.5 |
Pediatrics surgery |
39 |
6 |
49 |
6 |
8.2 |
15.4 |
0.5 |
Urology surgery |
37 |
5 |
81 |
14 |
5.8 |
13.5 |
0.4 |
Total (N ) |
242 |
55 |
525 |
107 |
4.9 |
22.7 |
0.44 |
Table 2 Blood ordering and utilization indices of different surgical departments of Tiku Anbessa Specialized Hospital from February 1, 2017 to March 31, 2017 G.C. (N=242)
*CM, cross-matched, TD, transfused, C/T, cross match transfusion ratio, %T, transfusion probability, TI, transfusion index
Blood requisition and utilization of surgical procedures with respective MSBOS
Based on the Mead's criterion majority of surgical procedures didn’t need preoperative preparation of cross-matched blood and group save and hold (GSH) will be enough. Only craniotomy (neurosurgery) and transurethral resection of bladder tumor needs preoperative cross-matched blood preparation and perioperative transfusion (Table 3).
Procedure |
Patients CM |
Patients TD |
Units CM |
Units TD |
C/T |
%T |
TI |
MSBOS |
Craniotomy |
24 |
12 |
75 |
26 |
2.9 |
50 |
1.1 |
2 |
Excision * |
5 |
1 |
8 |
1 |
8 |
20 |
0.2 |
GSH |
Exploration* |
8 |
2 |
15 |
2 |
7.5 |
25 |
0.3 |
GSH |
Laparotomy |
8 |
2 |
21 |
5 |
4.2 |
25 |
0.6 |
GSH |
ORIF of Femur |
21 |
3 |
41 |
6 |
6.8 |
14.3 |
0.3 |
GSH |
PNL |
5 |
0 |
10 |
0 |
- |
0 |
0 |
GSH |
Pullthrough |
8 |
1 |
10 |
1 |
10 |
12.5 |
0.1 |
GSH |
Pylolithotomy |
10 |
0 |
19 |
0 |
- |
0 |
0 |
GSH |
TAH |
12 |
3 |
32 |
6 |
5.3 |
25 |
0.5 |
GSH |
THE |
7 |
2 |
20 |
4 |
5 |
28.6 |
0.6 |
GSH |
Thoracotomy* |
11 |
0 |
25 |
0 |
- |
0 |
0 |
GSH |
Thyroidectomy |
6 |
0 |
14 |
0 |
- |
0 |
0 |
GSH |
TURBT |
5 |
3 |
14 |
9 |
1.6 |
60 |
1.8 |
2-3 |
Uritheroplasty |
7 |
0 |
12 |
0 |
- |
0 |
0 |
GSH |
Urithroscopy |
5 |
0 |
9 |
0 |
- |
0 |
0 |
GSH |
Table 3 Blood ordering and utilization indices of various surgical procedures with their respective MSBOS for TASH from February 1, 2017 to March 31, 2017 G.C
*thoracotomy (pneumonectomy, BPF repair, cyst removal), Excision (of soft tissue mass) Exploration (for biliary and renal stone), PNL, percutaneous nepherolithotomy; TAH, total abdominal hysterectomy; THE, trans hiatal esophagotomy; TURBT, transurethral bladder tumor resection
*thoracotomy (pneumonectomy, BPF repair, cyst removal), Excision (of soft tissue mass) Exploration (for biliary and renal stone), PNL, percutaneous nepherolithotomy; TAH, total abdominal hysterectomy; THE, trans hiatal esophagotomy; TURBT, transurethral bladder tumor resection
In this study, we found out that 77.3% of elective surgical patients didn’t need blood transfusion in agreement with as stated by other studies 77% of operations will need no pre-operative preparations of blood.2,3 This study revealed that only 20.4 % of the cross-matched blood was utilized which is almost comparable to that reported in Nepal 2009 (17.24%) and Zambia 2015, (23.8%) of blood cross-matched was utilized.7,8 But the utilization was relatively efficient compared to a study conducted in Bellary, India, 2012 (26%), Egypt, 2011 (25.2%), Nigeria, 2014 (34.51%), University of Gondar hospital, Ethiopia, 2013 (36%).9–12. Despite the disparity in the degree all might depict that the problem is common worldwide especially in developing countries including Ethiopia.
To determine the efficiency of blood ordering and utilization system several indices are used. Boral Henry was the first that suggested the use of cross-match to transfusion ratio (C/T ratio) in 1975. Consequently, many authors used C/T ratio for evaluating blood transfusion practice and ideally, this ratio should be 1.0, but a ratio of 2.5 and below was suggested to be indicative of efficient blood usage.1 According to the recommendation, a cross-match to transfusion ratio of 4.9 in Tikur Anbessa Specialized Hospital is unacceptably high which is twofold of the recommended. Despite this, the result is comparable with Malaysia, 2002 (5),13 better compared with Nepal (11.7), and India tertiary care teaching hospital, 2000 (6.6)7,14 and shows significant wastage of blood compared with Egypt (3.9), Zambia (2.8) and in our country at university of Gondar hospital (2.6 and 2.9 in elective surgical and gynecologic patients).8,10,12
A probability of transfusion of 30% and above has been suggested as appropriate.1 The results of the present study revealed an overall transfusion probability of 22.7%, which was indicative of inappropriate utilization compared to units of blood cross-matched. This study is almost near to Zambia (20%)8 and higher than the study conducted in Nepal (13.5%)[11]and Indian tertiary care hospital (11.1% to 25%)14 but it is lower than Egypt where it was 36.9% and Nigerian (34.51%).11
A transfusion index of 0.5 or more is indicative of efficient blood usage.1,15 The overall transfusion index reported in the current study was 0.44, which is near to Zambia 0.40. This finding was higher than the study conducted in Indian tertiary care hospital which was 0.3614 but lower than that reported in Egypt which was 0.69.10
Study in Westerns and some other countries showed their transfusion indices are becoming near to the standard even to the ideal; Aga Khan University Hospital, Pakistan 2001, the majority (97.56%) of the patients had C: T ratios higher than 2.5 latter in 2009/10 for procedures performed, C: T ratio was 1 in (95 %) procedures16. While in Leicester, UK, 2013(2.1)[17], Baltimore, Maryland, 2014 (1.54±0.07)18 this was achieved through continuous auditing and formulation of MSBO [16,17,18] whereas in developing countries like Ethiopia even the magnitude of the problem is yet not exploited. Therefore, this study is a revelation where we should focus in addition to awareness creation on blood donors to address the alarmingly increased demand for blood supply challenges.
From this study, none of the transfusion indices showed efficient blood utilization. Thus ordering large quantities of cross-matched blood for surgical patients of which little is ultimately utilized, incurs an artificial shortage in the reserves, wastes valuable technical time, and squanders expensive reagent. Above all, we have a blood supply challenge; collected less than half of the national requirement that necessitates the judicious use of blood and blood products. So frequent blood ordering and transfusion audits should have been made along with the formulation of a maximum surgical blood-ordering schedule.
In Tikur Anbesa Specialized Hospital, the amount of blood requested and cross-matched for patients undergoing elective surgery is much greater than the amount actually used. This high rate of unnecessary cross-matching of blood prior to surgery necessitate changes in the pattern of blood requisition and frequent audit.
It is a single-center study; therefore, our results cannot be generalized to other centers that follow different transfusion and technical protocols for different surgical procedures.
First, we would like to thank Tikur Anbesa Specialized Hospital for permitting us to do this research. Our gratitude also goes to the surgical staff of Tikur Anbesa Specialized Hospital and the departments for all the supports. Our gratitude also goes to Bahir Dar University for its financial support for the success of the project.
The authors do not have any conflict of interest regarding this article.

©2020 Tegu, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.