eISSN: 2469-2794


Review Article Volume 9 Issue 2
Nottingham Trent University, UK
Correspondence: Andrew O’Hagan, Nottingham Trent University School of Science & Technology, UK
Received: September 12, 2021 | Published: September 28, 2021
Citation: O’Hagan A, Westerman BL. An investigation into the effectiveness of the test and trace system for the SARS-CoV-2 pandemic within the UK. Forensic Res Criminol Int J. 2021;9(2):74-82. DOI: 10.15406/frcij.2021.09.00343
The investigation of the UK Test and Trace system illustrated that policies enforced were not sufficient to prevent the spread of SARS-CoV-2 in the UK. Some of the shortcomings included the app, the introduction to curfews and policies in hospitality sector, the methods of reporting COVID related deaths, restriction of movements across the border and adherence from the public. Other countries such as Japan and New Zealand implemented effective contact tracing systems due to the promotion of contact tracing and adherence to the policies created. These countries also had more preventive measures in place such as reducing attendees at school and enforcing the use of contact tracing for all industries. The Netherlands could also use more preventative measure to reduce cases, since there was a similar number of cases to the UK per 1 million in the population, however the mortality rate in the UK is double that of the Netherlands. To determine why, more research into pre-existing health conditions and obesity would need to be conducted to provide evidence into whether these factors effect mortality rates in SARS-CoV-2 cases. Research into other countries contact tracing systems can provide more possibilities for improvement.
Keywords: test and trace, Covid 19, SARS-Cov-2, contact tracing, prevent
Background information
SARS-CoV-2 or Severe Acute Respiratory Syndrome Corona virus 2 is a respiratory virus which is highly contagious and suspected to originate from a food market in Wuhan, China. Originally SARS-CoV-2 was diagnosed as Pneumonia cases in 2019 and is transferred to humans through interspecies transmission.1,2 SARS-CoV-2 is a positive, single-stranded RNA virus from the coronaviridae family and belong to the Nidovirales, which are known for causing respiratory and gastrointestinal tract infections, such as the common cold, bronchitis, and Pneumonia.3–5 Other common corona viruses include SARS and MERS (Middle Eastern Respiratory Syndrome) which have cause epidemics in 2003 and 2012 respectively.5,6
Corona viruses were named after their structure as their spike projections from the virus membranes resembles a crown structure; in Latin, corona meaning crown.4 These spike projections are (spiked) glycol proteins, or carbohydrate-protein complexes, found on the outer surface of the viral envelope. The inside of the envelope contains the nucleo capsid which is comprised of nucleic acid, in this case RNA, and capsids which encloses the nucleic acid.3,7,8 The structure of a virus is essential to understand how it enters and replicates in host cells. In this instance, the spiked glycol proteins bind to a cellular receptor called ACE2 in hosts, which initiates the release of viral RNA to undergo translation and replication into small proteins. These proteins act as capsids, or a shell, when viral RNA is added at the endoplasmic reticulum and the Golgi complex forming virions, a complete form of the virus, which are released out of cells in vesicles using exocytosis.7 Replication can occur quickly as there are only a few steps in virus replication, which is more rapid in corona viruses as the positive RNA strand acts like messenger RNA and can be translated directly.8 Although SARS-CoV-2 is genetically similar to SARS-CoV-1,SARS-CoV-2 has a higher reproductive rate. This is caused by slight structural differences in SARS-CoV-2 virus which allows for strong binding to the ACE2 receptor and are more efficient in evading host cells.9 Another cause of increased replication is that SARS-CoV-2 has an affinity to the upper respiratory tract, infecting and controlling the airways more easily.9 These factors affect the transmission of the virus and is a main reason SARS-CoV-2 has caused a pandemic. China recognised that this outbreak was in Wuhan, and shared information with the World Health Organisation (WHO) in January 2020, a common method of notification for international outbreaks.10,11 After this point active surveillance was required to monitor the transmission of this disease. Since the first case was identified in December 2019, the pandemic was named COVID-19.
As a new corona virus, vaccinations were not available until the end of 2020. Therefore, the safest way of protecting the public was heavily based on contact tracing systems to monitor and track the spread of disease. The purpose of these monitoring systems is to reduce the spread of the disease and ensure that mortality caused by the disease is low. An example of this is the National Notifiable Diseases Surveillance System (NNDSS) in the US, which is a programme that monitors public health and control of approximately 120 diseases from infectious zika virus to food borne outbreaks such as E.coli and non-infectious conditions like lead poisoning. The surveillance system is use for collating, sharing and analysing data including policies, laws, information systems, and resources at local, state, territorial and national level.12 This system is being used by epidemiologists conducting public health surveillance to calculate key factors such as incidence (the number of new cases within a specific time period), prevalence (number of cases at one point in time), hospitalisation and deaths.13
Monitoring the transmission of diseases is common and have been utilised in other epidemics. A blog published by Public Health England (PHE) discusses using contact tracing for MERS, which caused an epidemic in Middle Eastern countries in 2012.14 For England, the PHE is responsible for surveillance of diseases, which is based on a surveillance strategy created in 2013 outlining the response to outbreaks, monitoring prevalence and incidence of infectious diseases, and prioritising the allocation of resources.15 To monitor the number of cases of SARS-CoV-2 in the UK, the PHE helped the release of the NHS Test and Trace system, to identify cases and reduce the transmission of the disease to minimise mortality.16 This is monitored by the reproductive rate (R rate) which determines how infectious a particular disease is at one point in time.16
The purpose of this investigation is to determine whether the UK’s Test and Trace system and response to the COVID-19 pandemic was efficient; this will be based on a comparison to other countries across the world and how effective their systems were. To explore this concept, data from February 2020 to February 2021 will be examined and analyzed to identify any trends present and correlate the data to each country’s response to reach a conclusion on whether the UK’s system was appropriate. Other factors, such as the population, border control and public reactions will be considered when concluding the efficiency of contact tracing systems.
Test and trace system in the UK
At the beginning of April 2020, just after a national lockdown had been announced across the UK, the Department of Health and Social Care published its plan to test for SARS-CoV-2, describing how the testing will be scaled accordingly. In this document, the plan describes a Five Pillar System forming the base of the Test and Trace system in the UK; pillar one focuses on scaling up NHS swabbing for those with medical need and “where possible” key workers i.e., those in a critical role such as doctors, and nurses. The second pillar concentrates on mass testing for all key workers including individuals working in social care. The third pillar was mass antibody testing of the public to determine whether people obtain immunity from the virus after infection. Fourthly, this pillar looked at surveillance testing to further research into the novel virus and develop new treatments and testing. Finally, the fifth pillar was to form a mass testing facility in aid to lead a movement in the diagnostics national effort.17 Some aims provided to facilitate the Five pillar system include increasing the number of swab testing for the first pillar. During March 2020, the Department of Health and Social Care stated that they were performing 10,000 tests a day and by April 2020 they wanted to increase to 25,000 tests per day. Their aims for pillar two was to network with companies such as Amazon, Boots, and universities to provide capacity for testing sites and provide mass swab testing.18,19 The third pillar focused on antibody testing for immunity using a rapid system for detection to determine whether “Life can return as normal”. Facilitating the fourth pillar involved surveys from PHE using high accuracy antibody tests. Pillar five involved large scale companies providing ventilators and pharmaceutical companies collaborating to formulate a diagnostic industry.18,19
To effectuate the Five Pillar System, lighthouse laboratories were created in Milton Keynes, Glasgow, and Alderley Park, consisting of qualified volunteers from industry and academia areas.20 Lighthouse laboratories are facilities dedicated to corona virus testing at high throughputs as part of the National Testing Programme.20 All lighthouse laboratories are managed through the Department of Health and Social Care and are each reviewed by experts with their own virology adviser.21 The first laboratories were set up in Milton Keynes and Alderley Park in Cheshire.22 Other methods of increasing capacity have been partnering laboratories which perform a high volume of corona virus testing alongside other services. A partnership agreement with public, private, and academic sectors were utilised to increase the capacity.21
A factor of concern with the use of these laboratories is the quality assurance and whether protocols are being followed according to the appropriate accreditation. According to the government website, the lighthouse laboratories were set up by scientific experts with decades of experience, however, does not provide any information of how suitable protocols have been placed or how quality standards are met.21 To further this concern, an online news article implies that a panorama journalist from the BBC was working as a laboratory technician in one of the lighthouse laboratories. They reported that ISO standards were not being followed and staff were under pressure, had malfunctioning equipment and tests discarded wrongly.23 The credibility of this source is low, as there is no apparent author, therefore the accusation of poor laboratory practice is nothing more than an assumption. Nevertheless, there is no apparent evidence to prove improper or proper laboratory standards which introduces doubt into the public’s trust in the national health services and the Government.
The system in the UK has been set up to work collaboratively with Test and Trace apps, there are different apps depending on which part of the UK an individual lives; for England and Wales the NHS app is used, in Scotland an app called Scotland protect Scot is utilised and finally Northern Ireland uses COVID NI app.24 The app is used to help contact people who may have been in contact with someone who tested positive for SARS-CoV-2, known as contact tracing, however this relies on individuals to report their symptoms to obtain a test. This is achieved by scanning QR codes for buildings and stores requiring internet access and Bluetooth to determine if an individual has been within 2 meters of a person testing positive for longer than 15 minutes. The individual would then be notified to be tested, without sharing confidential information such as the name of the person who was confirmed as a positive case.25
An individual showing symptoms, or advised to take a test, can obtain a test via multiple routes. Tests can be ordered online using the NHS website or calling 119 if they do not have access to the internet. Walk in or drive through corona virus testing site are available by booking an appointment. Since April 2021, everyone can access free lateral flow tests by ordering a testing kit online through the government or NHS website which do not require laboratory testing. Once an individual has access to a test, their swabs are sent to a laboratory, one part of the National Laboratory Network, for analysis. Once the results are obtained, the NHS contacts the individual with the results; if positive the individual should isolate for 14 days, which was decreased to 10 days in December 2020, and follow instructions provided on the app so that others can be tested. If not followed, then an individual can receive a £1000 fine.16 To investigate how effective the UK contact tracing system is, the advantages and disadvantages of the NHS Test and Trace app is shown in Table 1. Other issues had occurred when the app was publicized as there were rumors that the app violated data protection laws and unknowingly changed phone settings, leaving the public feeling as if they lost their right for privacy in their life.26 This resulted in some of the public being unwilling to use or download the app, which then lowers the efficiency of the app and the Test and Trace system. This leads into investigating adherence from the public and the effect on the Test and Trace system.
|
Benefits to the NHS test and trace app |
Negatives to the NHS test and trace app |
|
Easy to access and scan |
Some individuals do not have access to a smart phone |
|
Reduces use of paper which can transmit virus |
Is dependent on Bluetooth and Internet access |
|
Rapid notification of contact between individuals |
Notifications do not always work or can be turned off |
|
If phone is turned off or runs out of battery the app will not work |
Table 1 Table demonstrating advantages and disadvantages to the NHS Test and Trace app
Adherence to the test and trace system UK
An article by Smith and others stated in October 2020 that three quarters of individuals with symptoms in their household reported of leaving their home within the last 24 hours when participating in this survey.24 This article also noted that men were more likely to not adhere to rules and leave their household when themselves or a member had symptoms of corona virus, this refers to similar trend in the 2009/2010 UK influenza pandemic. They suggested a targeted campaign aim at men could have increased adherence to lockdown rules. Another significant finding is that adherence to self-isolation is associated with fear of becoming infected, therefore when the number of cases decline, adherence is lower as the public are less afraid. This research concluded that self-adherence and self-isolation was poor at the time of research and suggested effective use of a volunteering system to provide essentials to those shielding and isolating would increase adherence in a pragmatic way.27
In another study, Wright and others suggested that people with higher awareness of COVID-19 i.e., higher levels of knowledge in relation to COVID-19, is associated with higher adherence based on research performed at UCL.28 Wright and others also investigated other factors such as confidence in institution; it was implied that individuals with high confidence in the government and the health services had a higher compliance to the laws relating to COVID-19. However, this research included people volunteering as part as a community group in low adherence even though Smith and others suggested that these volunteers would help increase compliance to the rules.27,28
Both articles discuss that there are limitations in their research for example Wright and others mention that their data can be subjected to selective bias as they specifically used data from a study focused on COVID-19 and the selection of samples are not representative of the general population.28 Smith and others implied that their research may not accurately represent the general population and included other limitations, they did not ask whether individuals encountered another individual from a different household, as non-adherence is not the only factor to increase transmission of the virus.27 Both studies suggested that adherence varies but can be improved, for example increasing the trust in the ability of the Government in handling the pandemic and focusing on establishing volunteer systems. This allows isolated individuals access to essential items without leaving their household and increasing risk of infection.27,28
Case data on Civid-19 pandemic
To determine whether contact tracing systems were effective, data obtained by the World Health Organisation was collected and analysed to produce the figures below; these focus on the UK, the Netherlands, Japan, and New Zealand. This involved observing differences between the cumulative total of SARS-CoV-2 cases, the cumulative total of SARS-CoV-2 deaths and factoring population on the cumulative totals.
From observing the graph, there is a general trend of increasing numbers between November 2020 and February 2021.The total number of cases in the UK is constantly above any other country and the difference increases especially towards the end of February 2021 as the UK has four times the number of cumulative cases compared to the Netherlands and Japan. When comparing all the countries investigated, New Zealand has the minimal number of cases and does not increase during the November 2020 to February 2021 period unlike all the other countries. Generally, all countries apart from New Zealand, have had an increase in case numbers of SARS-CoV-2 between November 2020 and February 2021.
Possible factors contributing to the increase of SARS-CoV-2 transmission
One possible causation is easing of lockdown rules and low adherence of the public. Poole and others investigated the transmission of Rhinovirus during 2019 and 2020 to estimate the trend of SARS-CoV-2 cases during winter; from this research Poole and others determined some significant findings. The percent proportion of positive tests is generally higher in 2020 than 2019.33 Secondly, in both years, transmission increased when schools reopened and when lockdown began to ease.33 This indicates that transmission is prominent when schools reopen therefore an increase SARS-CoV-2 transmission is likely to happen when schools reopen. In the UK, schools reopened in September 2020 and only closed during the UK’s third lockdown announced on January 4th, 2021. During this time, UK citizens would traditionally celebrate Christmas which has a focus on meeting family and friends, and exchanging gifts, allowed by the government, which would drastically increase transmission of SARS-CoV-2. These factors are likely to contribute to the increase of cumulative cases during the winter and spring seasons in the UK. To identify if schools reopening was a general cause or just specific to the UK, the other countries’ tactics were investigated.
In the Netherlands, pupils returned to schools in June 2020 which was before UK students returned to school.34 A Dutch head teacher explains that students under the age of 12 could mingle freely but socially distance themselves from adults. Other conditions include parents waiting at the fence at the beginning and end of school. Van Druijten states that is this an issue when there’s hundreds of parents at the fence waiting for their children.34 Van Druijten also discusses promotion of frequent hand washing and designated areas for the children to work or for younger children to play in and restricts movement from these areas.34 This extract from Van Druijten is not representative of all the schools in The Netherlands. A different newspaper article mentions how each district had different policies in place for when schools reopened, which is similar to the conditions UK schools were given.35 The UK were given basic guidelines from the Government, such as students in year 7 and above (aged 12 and over) must wear a face covering unless exempt for medical reasons,36 however guidelines would vary depending on size and population of the school and the staff available. For example, according to the Government guidance, schools are encouraged to separate toilet blocks if possible.37 The similarity in monitoring and reducing transmission in schools could be a cause for increased cases in both the UK and the Netherlands.
Japanese students returned to school in May 2020. Schools considered conditions such as decreasing overcrowding and reducing the number of school hours which was achieved by letting students attend either once or twice a week.38 However, similar to The Netherlands, different areas applied different policies in school and some schools returned in June 2020 instead.38 These policies were set by the Ministry of Education, Culture, Sports, Science and Technology – Japan (MEXT) which set out to provide costs for disinfectants, thermometers and also funding for classroom equipment. Furthermore, MEXT also state in this report the number of infections and the source of transmission; between June 1st, 2020 and June 31st, 2020, 242 out of 12 million students tested positive for corona virus. Out of the 242 cases, 57% was caused by household transmission and only 5% of cases were caused by in-school transmission.39 The report by Wada and others on school students aged 6-12 and 13-15 on the transmission of SARS-CoV-2 during the 1st to 31st June 2020, also supports the MEXT findings.40 In the UK, it is not known where the transmission source is from or where most of transmissions occur as the data is not available to the public. This could be interpreted as a lack of transparency from the Government or a lack in efficient monitoring of the disease. If this were implemented, the UK could determine if schools cause increased transmission.
New Zealand schools started to reopen in April and May 2020 according to guidance from the alert level system. At level 4, all schools are working remotely as lockdown is in place, at level 3 school years 1-10 and early childhood centers can return at limited capacity and other students must use distance learning.42 At level 2 all schools are open and accessible for all with specific safety measures in place, for example schools will close for cleaning and contact tracing if there is a confirmed case when at school. Some other safety measures include using a contact tracing system in all schools which was implemented in level 3, providing distance learning to those who are vulnerable and are shielding and requesting that ill individuals remain at home. For level 1 similarly to level 2 all schools are open and operate safely.42 In the UK there was no contact tracing systems in place and schools did not close for cleaning when there were cases of SARS-CoV-2, which clearly shows lack of efficiently monitoring the outbreak and preventing cases.
Another consideration to the increase of cases in the UK is the introduction of curfews in September 2020 by the Government to the hospitality sector. Pubs, bars, and restaurants were to close at 10pm in efforts to reduce the amount of time the public spent in these buildings to lower the likelihood of transmission as cases had begun to rise.43,44 This new enforcement brought new issues to contend with as in the beginning, people would all leave the pub, bar or restaurant simultaneously then in some cases continue drinking in one household. People often started drinking earlier and therefore still spent the same amount of time in one particular building with people outside their household.45,46 This is a possible causation to the increase of cases, as there was a greater opportunity for transmission of SARS-CoV-2, due to the crowding and prolonged periods in the hospitality setting.
During September 2020, New Zealand had their bars open for 3 months with no or very minimal cases of coronavirus.47,29 Safety measures in hospitality settings in New Zealand include using the contact tracing app or similar, remain seated where possible, remain 1 meter apart from other groups and maintain one server for the duration. Japan’s bars and restaurants also began to reopen in May, however there were some concerns about the number of cases and deaths as some individuals thought it was too early to reopen.48 Bars and restaurants can remain open till 8pm depending on the prefecture and each prefecture’s cases.49 In the Netherlands bars and restaurants reopened in June, allowing 30 people indoors and an unlimited number of people outside regarding that they remain 1.5 meters apart from other groups.50 In October, the Netherlands returned to a partial lockdown which meant that the hospitality sector had to reclose.51 Overall, the other countries did not have issues with curfews and generally were allowed more freedom in relation to using hospitality sector.
One factor that could cause general increase of numbers is that influenza, a similar virus to SARS-CoV-2, is seasonal and cases increase in winter periods. There is currently very little evidence on the effect of influenza on SARS-CoV-2 cases but would be an area of consideration to investigate when the data is available.
The death total from all the countries except the UK remain relatively low whereas the UK death total reaches 20,000 between April 2020 and May 2020. For both Japan and The Netherlands there is a general increase from April 2020 to February 2021, but the cumulative number of mortalities remain under 20,000 whereas the total cumulative death number for New Zealand is much lower. The UK’s cumulative death number is almost five times higher than the Netherlands’ and Japan’s cumulative mortalities. Some factors not considered in Figures 2 & 3 is population size and density. These factors are shown in Table 2.
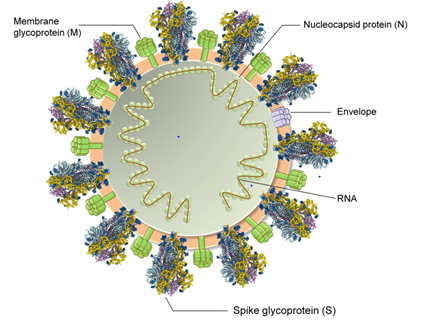
Figure 1 Annotated structure of SARS-CoV-2, demonstrating significant characteristics such as the Envelope, the membrane glycol proteins and nucleo capsid protein.7
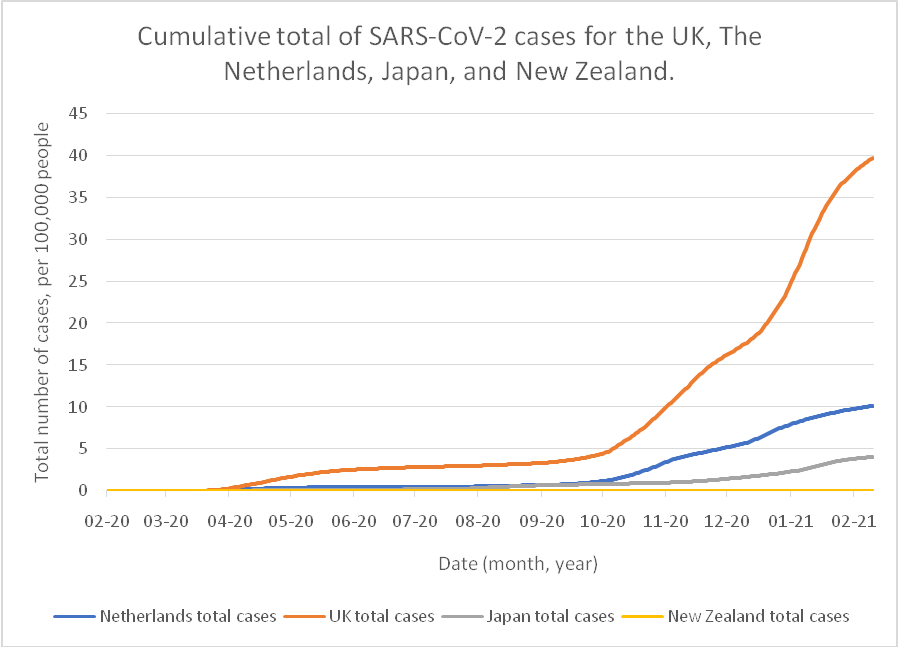
Figure 2 Graph demonstrating the cumulative number of SARS-CoV-2 cases, comparing the UK, the Netherlands, Japan, and New Zealand.29–32
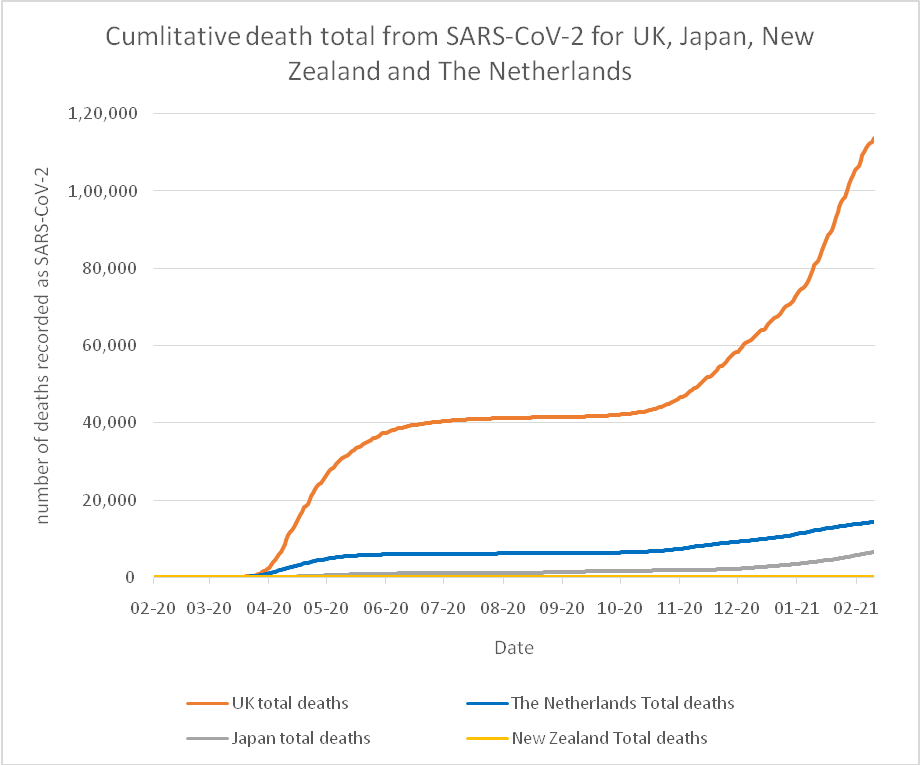
Figure 3 A graph demonstrating the total cumulative mortalities from SARS-CoV-2 infection in the UK, The Netherlands, Japan, and New Zealand.29–32
|
Country |
Population size (million) |
Population density (person/km2) |
Cases per 1 million people (population) |
Deaths per 1 million people (population) |
|
UK |
67 (52) |
281 (52) |
59,284 |
1,699 |
|
The Netherlands |
17 (53) |
508 (53) |
59,375 |
846 |
|
Japan |
126 (54) |
347 (54) |
3,239 |
52 |
|
New Zealand |
4 (55) |
18 (55) |
492 |
6 |
Table 2 Population and SARS-CoV-2 cases with appropriate representation
Data used from graph and only contains cumulative numbers up to February 2021
Some conclusions can be drawn from this table; Japan has the highest population and second highest population density but second lowest in cases and deaths from SARS-CoV-2 per 1 million people. The Netherlands, with the third highest population, had the highest population density and highest SARS-CoV-2 cases per 1 million, however the deaths are half those of the UK per 1 million of the population. New Zealand is likely to have benefited from a small population and population density but still have a small number of cases per 1 million people and mortalities per 1 million people. Both the UK and The Netherlands have a similar number of SARS-CoV-2 cases per 1 million people although the Netherlands mortality cases are half of the UK’s. To determine why the death rate is so much higher in the UK in comparison to the other countries, other factors were considered.
Factors effecting the death rate from SARS-CoV-2
One factor adding to the increased mortality is method of reporting deaths in the UK. It is assumed that reporting SARS-CoV-2 deaths is simple, however this does not consider other long-term illness or life changing traumas. For example, if a cancer patient was diagnosed with SARS-CoV-2 no matter the time period when the patient died, the cause of death would be classified as SARS-CoV-2.56 The World Health Organisation (WHO) stated that COVID-19 deaths are defined as so for surveillance purposes from a clinically compatible illness unless there is a clear alterative cause of death such as trauma.57 Towards the beginning of the pandemic, the UK was reporting all deaths with a positive test of SARS-CoV-2 as COVID-19 related death based on the criteria of a clinical assessment provided from WHO.56 Although Newton suggested that this method is robust, it does not take into consideration deaths from other causes as specified earlier or alternatively individuals that died before being confirmed as a positive case.56
To increase the complexity of this issue, Scotland has a different method of classifying SARS-CoV-2 deaths; if a death occurs after 28 days of a positive test, then the death is not classified as SARS-CoV-2 death.56 In April 2020, the method of classifying COVID-19 deaths changed allowing individuals’ deaths to be classified as SARS-CoV-2 death without a positive test and classifying deaths as SARS-CoV-2 after 60 days of a positive test.56,58 This introduces new issues into the complex death classification system as now there is no need for evidence to classify a SARS-CoV-2 death; it is possible that individuals could be classed by symptoms present which is problematic as it shares symptoms with other respiratory viruses such as influenza. There is also a possibility that individuals who are hospitalised for other reasons came into contact with the virus and tested positive for SARS-CoV-2 and therefore no definite cause of death as either factor could cause death.
Other possible considerations are the cuts to the NHS and social cares sections and possible health conditions including diabetes and obesity.59,60 There is very limited evidence to prove this affected the death toll, but the UK Government have introduced campaigns to reduce population obesity and the pressure placed on the NHS was present prior to the pandemic which are important to consider when reflecting on SARS-CoV-2 deaths.59,60 The number of people who have pre-existing respiratory conditions such as Chronic obstructive pulmonary disease (COPD) and asthma could affect the death rate if higher percentage of the population suffer from these conditions.
Other countries contact tracing systems
In New Zealand, the Government introduced the Alert system on the 21st of March 2020 which consists of four levels, four being the highest level and one being the lowest. Prior to this, the New Zealand government banned gatherings over 100 people on the 19th of March 2020 as well as closing the borders on the same day. If any changes to the alert system occurred, they would be implemented within 24 hours. Some precautions include contact tracing for all indoor public buildings such as restaurants and schools.47,42,61 The public can decide which tracing app or method they prefer if they participate in contact tracing.61
All these decisions are based of a surveillance strategy using five objectives; the first objective was to identify all cases for public health management from which the government wanted to find methods to detect cases early.62 The second objective was to evaluate the response from this considering all the perspectives such as the capacity of the health system, is contact tracing is effective, how effective public health measurements are at the border and the degree of undetected infection.62 The third objective considered researching into the virus to learn more about disease risk and patterns such as identifying groups who are most at risk. The fourth objective was to monitor the disease to ensure equity in relation to testing, border control and public health management.62 The final objective was to ensure the public confidence and participation in their response to the pandemic by determining what level of accept and adherence is appropriate for the public.62 With these at the core of the government decisions, New Zealand was able to achieve a high compliance rate to COVID-19 related laws.63
One effective method of controlling the spread in Japan was the accessibility of diagnostic tests to detect SARS-CoV-2 cases. The government has offered PCR testing, Antigen testing, and Antibody testing to the public explaining the guidelines for each test and where they can be obtained.64 Since March 2020, the government have stated that PCR tests will be covered by medical insurance allowing private institutes to use PCR testing outside of public health centres, which is considerably earlier than the UK’s testing system.64 The effective PCR testing is only a small section of Japans 3-part strategy or 3 strategies; the first and second parts involve promoting social distancing, contact tracing, and surveillance under the Patient Cluster Countermeasure Group of the Ministry of Health, Labour, and Welfare. All contact tracing was performed by the public health centres which, prior to PCR testing, used computed tomography (CT) scanners to investigate suspicious pneumonia cases. The third strategy involved addressing public behaviour and promoting frequent handwashing, coughing, and sneezing etiquette as well as prioritising healthcare for the elderly.65 Additionally, the citizens of Japan have a high adherence to the recommendations provided by the Government as a study found that 80% participants implemented social distancing measures along with the suggested behavioural changes for virus prevention i.e., frequent hand washing.65 Another principal factor is Japan’s border control which imposed travel restrictions from March 2020, which increased to limited access for entry into the country.66
Similar to the UK, the Netherlands’ principles for monitoring cases included a contact tracing app known as Corona Melder. All cases had to be reported to the municipal health service with information about who you’ve been within 1.5 meters of for at least 15 minutes in a 24-hour time period including the possible source and the potential individual who could be infected.67,68 Adherence to lockdown rules was low like in the UK as, according to a study by Bente and others, the Dutch were likely to visit their family and were less likely to wear a mask compared to people from Fleming although the Dutch were more likely to wash their hands.69 As the number of SARS-CoV-2 cases are similar, there are more effective methods for monitoring, and low adherence to rules can majorly tribute to surge in SARS-CoV-2 cases. Alternatively, the death rate is much higher in the UK than it is in the Netherlands. Some factors affecting this could include the health of the population and number of people vulnerable to SARS-CoV-2 but with little evidence to prove correlation between state of health and SARS-CoV-2 infections a strong conclusion cannot be made. In relation to border control, the UK made minimal effort to restrict border movements and many people were able to travel for holidays during 2020.70 The Netherlands did close their border but only to countries outside of the EU, which can be problematic as many EU countries had large outbreaks of SARS-CoV-2 such as Italy.71
As demonstrated in Table 3, adherence to government recommendations and closure or restriction of movement across borders are significant factors to the number of cases of SARS-CoV-2. These are important to consider as reducing the transmission of the virus will decrease the mortality caused by SARS-CoV-2. The effectiveness of the contact tracing system is dependent on the attitude of the country’s citizens and limited access of entry from other countries across the world. There is minimal evidence to find a definite cause to the UK’s high mortality rate, but the insufficient procedures in place and the public’s low adherence caused by losing trust in the government capabilities is one important aspect to the UK’s poorly performing Test and Trace system. Some trust was lost from the public from rumours of poor laboratory standards in lighthouse laboratories, intrusion of privacy and counterproductive curfews, drastically affecting the number of SARS-CoV-2 cases and mortalities.
|
Country |
Closed borders/strict restrictions |
Adherence to corona virus laws and recommendations |
Total cases of SARS-CoV-2 (up to 10th February 2021) |
Total deaths from SARS-CoV-2 (up to 10th February 2021) |
||
|
UK |
× |
Low |
39,72,035 |
1,13,832 |
||
|
The Netherlands |
× |
Mid to low |
10,09,373 |
14,374 |
||
|
Japan |
√ |
High |
4,08,084 |
6,610 |
||
|
New Zealand |
√ |
High |
1,967 |
24 |
|
|
Table 3 Summary of significant findings
Adherence and closure of borders are not the only factors affecting case numbers as transmission in schools requires consideration. Each country had similar basic procedures such as promoting regular hand washing, however some countries put more policies into place. For example, Japan reduced the number of students in classes, increased the teaching staff and reduced the hours spent at school. Smaller groups and less time spent at school meant that there was a smaller transmissibility between students and staff members. New Zealand close schools when an individual tested positive so the school could be sanitised. Both Japan and New Zealand had contact tracing within their school environments unlike the UK which had no obvious requirement for contact tracing in schools. These differences highlight how additional policies can reduce the transmission of the virus and emphasises how the government has lacked in support of implementing a contact tracing system successfully into society.
Hospitality sectors had some significance to the transmission of SARS-CoV-2. Each country has similar principles for safety such as the use of contact tracing systems via an app or taking contact details from customers. The UK, particularly when introducing curfews, introduced more risks due to the response of the public. After a brief time, the curfew in the UK was adjusted to reduce the transmission risk created. Japan was able to successfully introduce curfews which were earlier than the curfews implemented in the UK. This clearly demonstrates how adherence is important in contact tracing systems to reduce transmission.
When comparing each countries’ contact tracing system, the objectives and aims are similar, however the implementation of the objectives varies significantly which determines the effectiveness of each countries monitoring system. Japan changed the public’s behaviour effectively unlike the UK and the Netherlands. Japan utilised a contact tracing system through the Ministry of Health, Labour and Welfare, like the NNDSS; an effective system for epidemiologists to collate, analyse and share data. If a system like the NNDSS was implemented into the UK information between experts, the Government and the public could have been accessed more rapidly. The UK’s system would be improved by introducing alternative contact tracing apps as offered in New Zealand or through a nationalised system like Japan.
Some recommendations for this investigation include assessing other countries like Australia, Taiwan, USA, Canada, or any other European country. This is to compare the similarities and differences between the contact tracing systems, and strategies in place monitoring transmission and mortality. Another consideration is to investigate into pre-existing health conditions and their effect on mortality in relation to SARS-CoV-2, which could be possible when more published research is performed into these areas. When definite causes are known, more recommendations can be provided to improve how the UK handle epidemics and pandemics.
None.
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported on this paper.

©2021 O’Hagan, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.