eISSN: 2473-0815


Case Report Special Issue Thyroid Research
Department of Paediatrics, University of Patras School of Medicine, Greece
Correspondence: Eirini Kostopoulou, Department of Paediatrics, University of Patras School of Medicine, Greece
Received: April 22, 2017 | Published: November 15, 2018
Citation: Kostopoulou E, Spiliotis BE. Severe constipation and growth impairment in a child with subclinical hypothyroidism. levothyroxine proven to be beneficial. Endocrinol Metab Int J. 2018;6(6):391-393. DOI: 10.15406/emij.2018.06.00218
Subclinical hypothyroidism (SH) is a common endocrine condition characterized by specific biochemical findings that include raised serum TSH concentrations, above the upper normal limit for the population, and circulating thyroid hormones within the lower normal range. To date, data from literature regarding the effect of SH on children’s general health and the necessity of treatment are contradictory or inconclusive. Therefore, additional studies are needed for more definite conclusions to be drawn.
We report a patient with severe constipation and poor growth during infancy that was also diagnosed with mild SH. He underwent multiple gastrointestinal investigations that failed to identify the cause of his symptoms. The patient had a successful trial of Levothyroxine that appeared to be beneficial in terms of eventually eliminating his constipation and improving his growth parameters. We suggest that SH, even in its mildest form, when presenting with severe symptoms not directly related to any other medical conditions, be treated, as the possibility of the treatment being beneficial may outweigh any potential harm.
Subclinical hypothyroidism (SH) is defined by persistently elevated serum thyroid stimulating hormone (TSH) concentrations, and circulating total or free thyroid hormone concentrations within the reference range.1 It is common in children, with a prevalence of less than 10%.2 However, according to paediatric studies, the progression to overt hypothyroidism is uncommon.
SH is classified as transient and persistent. The aetiology is multi factorial and includes random TSH variation ,3 non-thyroidal illness, structural abnormalities of the thyroid gland, 4 autoimmune Thyroiditis that recovers,5 obesity ,6 children born small for gestational age7 and mutations in the DUOX2, PAX8, TTF-1, GNAS1 and TSHR genes.8
Data from the literature appear to be inconsistent with regards to the clinical presentation of SH. Children with SH have been reported as asymptomatic in many studies or presenting with a variety of symptoms in other studies, such as poor school performance and impaired cognitive function9 , migraine headaches,10 weight gain, dyslipidemia11 and other subtle preatherogenic abnormalities12 and decreased growth velocity.13
There is lack of consensus with regards to the management of SH in the case of normal total or free T4 and a TSH of 5-10 mU/L. Different approaches range from prompt treatment after confirmation of the elevated TSH to frequent monitoring of TSH for a prolonged period without no action being taken, especially in the absence of a goitre or positive antithyroid antibodies. In the presence of a goitre or if the TSH is above 10 mU/L, the possibility of developing overt hypothyroidism is likely and treatment is more likely to be indicated.
SH is a very common entity in children and the majority of elevated TSH levels either revert to normal or remain mildly elevated. The literature suggests that treatment of SH is not beneficial for growth or cognitive development, but further studies are needed.
Here we present a male patient that was referred to the Paediatric Endocrine Outpatient Clinic at the age of 27 months (2yr 3mo) because of impaired growth after the age of 14 months (Figure 1). The patient’s medical history revealed severe constipation from the age of 12 months. Defecation was only possible with the use of enemas or laxatives which many times were also ineffective. The rest of the medical history was unremarkable, including the perinatal period, with the patient having reached all the developmental milestones in the acceptable range.
From the family history, the patient’s mother suffered from mild constipation and her sister from hypothyroidism.
At the age of 21 months the patient was assessed by several Paediatric Gastroenterology teams. Extended investigations were performed, including allergy tests, endoscopy of the upper and lower gastrointestinal tract, a sweat test, esophageal manometry and a coeliac screen. No pathological findings were identified and the aetiology of the patient’s constipation remained unknown after Hirschprung’s disease, coeliac disease, food allergy and other gastrointestinal abnormalities were excluded.
The physical examination revealed no abnormal findings. The patient’s vital signs were within the normal range and there was no palpable goitre. His growth curve revealed that his weight was consistently along the 5thcentile but his height fell below the 5thcentile at 26 months (2yr 2mo) of age (Figure 1).
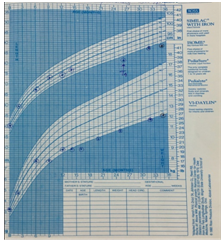
Figure 1 Growth curve of the patient before and after Thyroxine therapy showing good initial “catch-up” growth but with poor growth again later.
On the day of the assessment, the patient had a mildly elevated TSH concentration of 4.6 mU/l (Normal range: 2.5-4.1) and normal T3, T4 and FT4 levels. Antithyroid antibodies (anti-TPO and anti-TG) were negative. A thyroid ultrasound though, revealed diffuse heterogeneous echogenicity and 2 small hypoechoic nodules, measuring 3mm each. A few months prior to the patient being assessed by our Endocrine team, the TSH concentration was also elevated (5.38 mU/L) with normal thyroid hormones (Table 1).
Because of the impaired growth and severe constipation in the setting of subclinical hypothyroidism with abnormal ultrasound findings, we decided to initiate treatment with Levothyroxine at the dose of 1 μg/kg.
Within 3 weeks from the initiation of Levothyroxine, the constipation was greatly improved and subsequently disappeared at one month of therapy .Three months after treatment, the TSH decreased to normal levels and FT4 remained within the normal range (Table 1). The growth velocity of the patient improved until the age of 3 years (Figure 1).
At the age of 3 years, the patient’s growth velocity declined again. Hematological, biochemical and thyroid function tests were normal, whereas Growth Hormone Deficiency was proven by GH provocative tests using Clonidine and L-DOPA (Table 2). An MRI scan of the hypothalamus and pituitary gland was unremarkable. The patient was started on exogenous Growth Hormone replacement therapy and his growth pattern became normal thereafter (Figure 2).
Age |
T3 (nmol/L) |
T4 (nmol/L) |
FT4 (pmol/l) |
TSH (mU/L) |
|---|---|---|---|---|
Normal Range: 0.7-1.7 |
Normal Range: 62-165 |
Normal Range: 8-20 |
Normal Range: 2.5-4.1 |
|
1yr 10mo |
1.6 |
88 |
13 |
5.38 |
2yr 3mo |
1.2 |
100 |
15 |
4.6 |
(1st Endocrine assessment) |
||||
2yr 6mo |
- |
- |
16.6 |
2 |
2yr 11mo |
- |
- |
12.5 |
1.72 |
Table 1 Thyroid function test results of the patient. The abnormal TSH concentrations are highlighted in red.
Provocative Test/Time |
GH (L-DOPA) (ng/ml) |
GH (Clonidine) (ng/ml) |
T=0 min |
3.57 |
5.29 |
T=30 min |
1.57 |
2.72 |
T=60 min |
2.46 |
2.77 |
T=90 min |
4.23 |
1.61 |
T=120 min |
5.43 |
1.49 |
Table 2 Growth hormone concentrations of the patient after pharmacological provocation with L-Dopa and Clonidine showing abnormal peak GH concentrations in both tests.
Whether SH is associated with growth or cognitive impairment during childhood or bone health and metabolic disorders in adulthood is still controversial.
There is currently no consensus regarding treatment of mild subclinical hypothyroidism (TSH: 5-10 mU/L), particularly in children. The current recommendations from the European Thyroid Association for the management of subclinical hypothyroidism suggest treatment with Levothyroxine if the concentrations of TSH>10 mU/L, particularly when anti-thyroid antibodies are positive and in the presence of a goiter. In the absence of a goiter and when TSH levels are below 10 mU/L, monitoring of FT4 and TSH in 12 months is recommended.14 If the anti-thyroid antibodies are negative, a close follow-up is recommended. However, more studies are required for the duration of the follow-up to be determined.
In addition, patients with SH may present with severe symptoms, as in the case of our patient. In this scenario, especially if the symptoms cannot be attributed to any other medical causes, treatment with Levothyroxine may be beneficial, even if TSH concentrations are mildly elevated or within the upper normal range for the population. The absence of data in the literature regarding the usefulness of treatment with Levothyroxine in mild subclinical hypothyroidism does not necessarily suggest absence of benefit. More studies are warranted for definite conclusions to be drawn with regards to the long-term outcome of patients with or without Levothyroxine treatment for SH. Until the literature is conclusive, treatment plans should be decided on an individualized basis, after thorough co-assessment of all the clinical, laboratory and imaging parameters.
None.
The authors declare no conflicts of interest.

©2018 Kostopoulou. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.