eISSN: 2473-0815


Research Article Volume 5 Issue 2
1Department of Endocrinology, University of Pennsylvania, USA
2Department of Medicine, Einstein Medical Center, USA
3Chair of Endocrinology, Einstein Health Care Network, USA
Correspondence: Lakshmi Kannan, MD MSc, Mol Med, Fellow, Department of Endocrinology, University of Pennsylvania, USA, Tel 4146306791
Received: September 13, 2016 | Published: July 12, 2017
Citation: Kannan L, Pomerantz S, Chernoff A. Hypothyroidism and the metabolic syndrome. Endocrinol Metab Int J. 2017;5(2):188-191. DOI: 10.15406/emij.2017.05.00115
Objective: To examine the relationship of hypothyroidism and the metabolic syndrome and to explore differences in individual parameters of the metabolic syndrome between hypothyroid and euthyroid states.
Methods: In this retrospective case control study we analyzed 149 subjects in total, 39 euthyroid and 110 hypothyroid subjects. Metabolic Syndrome was defined as per ATP III criteria. All data were collected through chart review. Study groups were analyzed for differences in baseline demographic variables including age, gender, smoking status and alcohol consumption. Statistical analyses performed for the primary outcome, difference in metabolic syndrome prevalence, included the Chi-square test and logistic regression analysis. All analyses were performed on the SPSS platform.
Results: Study groups were similar at baseline demographic variables including age, gender, smoking status and alcohol consumption. The prevalence of metabolic syndrome was found to be 28.2% in euthyroid and 51.8% in hypothyroid subjects. Statistical analysis revealed an odds ratio of 2.6(CI 1.5 to 5.7) with a P-Value of 0.01. No statistically significant difference was noted in the prevalence of any single component of the metabolic syndrome though a uniform trend of increased prevalence among the hypothyroid group was seen. Subset analysis revealed a higher mean TSH among those with the metabolic syndrome as compared to those without, in both groups.
Conclusion: Our study suggests that hypothyroid subjects are at about 2 to 5 fold increased risk for metabolic syndrome independent of age, gender, smoking status and alcohol intake. This may contribute to the increased risk of atherosclerotic disease in hypothyroidism.
Keywords: hypothyroidism, metabolic syndrome, prevalence, coronary heart disease, overt hypothyroidism
ASCVD, atherosclerotic cardiovascular disease; CVD, cardiovascular disease; OH: overt hypothyroidism; SH, subclinical hypothyroidism.
The metabolic syndrome is a constellation of interrelated risk factors of metabolic origin that appear to directly promote the development of atherosclerotic cardiovascular disease (ASCVD).1 Prospective population studies show that the metabolic syndrome confers a 2-fold increase in relative risk for ASCVD events, and in individuals without established type 2 diabetes mellitus, a 5-fold increase in risk for developing diabetes as compared with people without the syndrome. At present metabolic syndrome appears to have multiple underlying risk factors, the most important of these being central obesity and insulin resistance. Other associated conditions include physical inactivity, aging, hormonal imbalance, and genetic or ethnic predisposition.
Thyroid function regulates a wide array of metabolic parameters. Thyroid function significantly affects lipoprotein metabolism as well as some cardiovascular disease (CVD) risk factors, thus influencing overall CVD risk. Hypothyroidism is characterized by impaired glucose absorption from the gastrointestinal tract and delayed peripheral glucose assimilation and gluconeogenesis, decreased or normal hepatic glucose output and decreased peripheral tissue glucose disposal. A recent cross sectional study revealed that even in the euthyroid state low thyroid function predisposes to higher cholesterol, glucose, insulin and insulin resistance.2 Thyroid disorders, including both hypo- and hyper-, have been associated with insulin resistance due to various mechanisms such as altered insulin secretion and lipid levels.3 Overt Hypothyroidism (OH) and subclinical hypothyroidism (SH) are characterized by attenuated basal plasma insulin and insulin sensitivity could improve following substitution therapy.4,5 Insulin resistance, present in both OH and SH, may increase cardiovascular risk, especially when it is associated with other frequently associated risk factors such as hyperlipidemia and elevated blood pressure.6
Hypothyroidism and metabolic syndrome per se increase cardiovascular morbi-mortality. We conducted a retrospective case-control study to explore the relationship of hypothyroidism and the metabolic syndrome
The study protocol was approved by Einstein Medical Center’s Institutional Review Board. All authors had access to the data and vouch for data accuracy and completeness.
Retrospective chart review was performed to identify the study population. We included hypothyroid subjects that were above18yrs of age, had documented hypothyroidism (primary or secondary) before index hospitalization, primary hypothyroid subjects had biochemical hypothyroidism as defined by TSH>4.9, a major proportion were on treatment though TSH was still elevated at the time of data collection. Biochemically euthyroid subjects that had all of the metabolic parameters available were included as controls. The following subjects were excluded, hypothyroid patients that were biochemically euthyroid after treatment, subjects that did not have a complete set of metabolic parameters available and patients admitted to the intensive care units.
Metabolic syndrome
Metabolic syndrome was defined as per Table1.
Triglycerides |
≥150 mg/dL |
HDL Cholesterol |
|
Men |
<40 mg/dL |
Women |
<50 mg/dL |
Blood Pressure |
≥130/≥85 mm Hg |
BMI |
≥30 |
Fasting Glucose |
≥110 mg/dL |
Table 1 Definition of Metabolic Syndrome- when at least 3 of the above 5 criteria were met; subjects were classified as having the metabolic syndrome
Statistical analyses
Demographic data were summarized using descriptive statistics. Group differences between those who are hypothyroid and those who are euthyroid were analyzed using t-test or chi square as dictated by data type. The comparison of the two groups on metabolic syndrome was done using chi-square test. The relationship between thyroid status and prevalence of metabolic syndrome after controlling for such risk factors as age, sex, smoking and alcohol intake was performed using logistic regression. The specific controlling variables were determined based on findings from the bivariate analyses. Among hypothyroid subjects with the metabolic syndrome, thyroid function, as measured by TSH and T4, was correlated with individual metabolic parameters using Pearson correlation coefficient. Subset analysis was performed comparing subjects with the metabolic syndrome and those without the syndrome within each thyroid status category.
Demographic data
One hundred and ten hypothyroid and thirty nine euthyroid subjects met inclusion criteria. Demographic characteristics are summarized in Table 2 with descriptive statistics and the corresponding p values. Hypothyroid and euthyroid groups were similar in terms of age distribution, smoking status and alcohol use. There were a higher proportion of female subjects in the hypothyroid group, though the difference did not attain statistical significance
Age |
Gender |
Smoking |
Alcohol |
||||
Mean (YRS) |
Females % |
Males % |
YES % |
NO % |
YES % |
NO % |
|
Euthyroid |
64.8 |
50 |
50 |
17.1 |
82.9 |
17.10% |
82.90% |
Hypothyroid |
66.6 |
67.5 |
32.5 |
21.4 |
78.6 |
12.80% |
87.20% |
p-Value |
>0.05 |
>0.05 |
>0.05 |
>0.05 |
|||
Table 2 Demographics of the study population
Thyroid status and metabolic syndrome
We found that 28.2% of the euthyroid and 51.8% of hypothyroid subjects met the metabolic syndrome criteria (Figure 1). Statistical analysis revealed an Odds ratio of 2.6(CI 1.5to5.7) with a P-Value of 0.01. The groups did not significantly differ in the prevalence of any single component of the metabolic syndrome, namely glucose tolerance, blood pressure, body mass index, HDL cholesterol or TGL levels, though a uniform trend of increased prevalence of each component among the hypothyroid group was present. Subset analysis revealed a higher mean TSH among those with the metabolic syndrome as compared to those without, in both euthyroid and hypothyroid groups, but this did not attain statistical significance (Tables 3A & 3B).
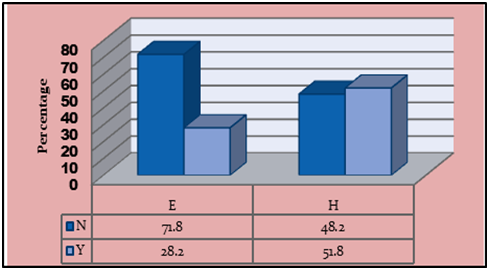
Figure 1 Prevalence of metabolic syndrome according to thyroid status. N- No metabolic syndrome, Y- Metabolic syndrome present. E Euthyroid, H Hypothyroid.
Parameter Metabolic Syndrome |
AGE (Yrs) |
TSH (mU/ml) |
HbA1c (g/dL) |
TGL (mg/dL) |
HDL (mg/dL) |
No |
69.9 |
1.5 |
6.9 |
1.4 |
58 |
Yes |
59.7 |
2.3 |
7.1 |
180.5 |
38.5 |
p-value |
0.13 |
0.08 |
0.72 |
0.02 |
0.001 |
Table 3A Subset analysis- Mean age, TSH, HgbA1c, Triglyceride and HDL by metabolic syndrome status in the euthyroid group with the corresponding p-values
Parameter Metabolic Syndrome |
AGE (Yrs) |
TSH (mU/ml) |
HbA1c (g/dL) |
TGL (mg/dL) |
HDL (mg/dL) |
No |
69.3 |
16.6 |
6.6 |
81.6 |
57.2 |
Yes |
63.9 |
17.6 |
7.2 |
153.8 |
38 |
p-value |
0.061 |
0.87 |
0.2 |
0.001 |
0 |
Table 3B Subset analysis- Mean age, TSH, HgbA1c, Triglyceride and HDL by metabolic syndrome status in the hypothyroid group with the corresponding p-values
Thyroid hormones (TH) play an important role in regulating energy balance, metabolism of glucose, and lipids. Individual components of the metabolic syndrome have been studied in relation to the thyroid status. Multiple studies in the general population have confirmed positive associations between serum TSH and BMI, arterial hypertension, especially diastolic hypertension, serum cholesterol and triglyceride levels.7‒12 Patients with thyroid dysfunction as such are at higher risk for cardiovascular morbidity and mortality.13 We postulated that given that metabolic syndrome per se contributes to increased cardiovascular risk, the combined burden of hypothyroidism and metabolic syndrome if present concurrently would pose a larger threat. In this retrospective case control study, we have observed that hypothyroid subjects have two to three times’ higher likelihood of having the metabolic syndrome as compared with euthyroid individuals. Additionally, there was a trend towards worse control of metabolic parameters though this did not attain statistical significance.
A number of studies have confirmed the associations of thyroid function with metabolic parameters in the general population.14‒20 Most of the studies conducted to date have been population-based, cross-sectional studies that performed correlation analyses of TSH and thyroid hormone levels with individual metabolic parameters. A study in Taiwan explored the serum TSH levels and metabolic syndrome components and concluded that even slight increases in TSH, as in subclinical hypothyroidism, may be a metabolic syndrome risk factor.17 Another study concluded that Higher TSH levels in subclinical hypothyroidism with a TSH>10mIU/l are associated with increased odds of prevalent metabolic syndrome.18 Moreover, even high normal TSH levels and low normal free T4 levels were significantly associated with increased prevalence of metabolic syndrome, which may be of importance when evaluating such subjects.19,20 Metabolic syndrome is increased in patients with hypothyroidism and suggested that hypothyroidism be considered in newly diagnosed metabolic syndrome patients.14 In accordance with the above-mentioned studies, we have found increased risk of metabolic syndrome in hypothyroidism. Metabolic syndrome could contribute to the association between hypothyroidism and atherosclerotic diseases such as ischemic heart disease, cerebrovascular disease and peripheral vascular disease.
It is important to note that in our study, differences in the individual metabolic parameters did not attain statistical significance between the euthyroid and hypothyroid groups. This could be potentially explained by other components of the metabolic syndrome, for example inflammatory markers such as CRP, which were not included in our study.
We acknowledge limitations in the current study including the retrospective study design and small number of subjects. It is also important to bear in mind that we used ATP criteria alone to define metabolic syndrome. It would be interesting to study the impact of other measures such as alternate classifications of MS, HOMA-IR to assess insulin resistance or the Triglyceride/HDL index on the association between thyroid status and metabolic syndrome.
Further research is needed to evaluate the cost-effectiveness and the timely approach for routine screening of hypothyroid patients for the metabolic syndrome, the effect of thyroid hormone replacement on the metabolic parameters and the target TSH level in hypothyroid individuals with metabolic syndrome.
Our study suggests that hypothyroid subjects are at about 2 to 5 fold increased risk for metabolic syndrome independent of age, gender, smoking status and alcohol intake. This may contribute to the increased risk of atherosclerotic disease in hypothyroidism.
None.
The authors declare that there are no conflicts of interest.

©2017 Kannan, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.