Update on GOUT (A Practical Approach......)
Osman El Labban
Regret for the inconvenience: we are taking measures to prevent fraudulent form submissions by extractors and page crawlers. Please type the correct Captcha word to see email ID.

Family Medicine Consultant & head of Department, Al Zahra Hospital, UAE
Correspondence: Osman El-Labban, Family Medicine Consultant & head of Department, Al Zahra Hospital, UAE
Received: August 12, 2016 | Published: August 16, 2016
Citation: El-Labban O. Update on GOUT. Biom Biostat Int J. 2016;4(3):113-116. DOI: 10.15406/bbij.2016.04.00098
Download PDF
Gout is an ancient disease which dates back to the time of Babylon. Its name comes from the Latin word gutta, (meaning drop), which reflect an old belief that the disease is caused by a poison which fall into the joint drop by drop.
The disease is quite prevalent nowadays and is considered as the most common inflammatory type of arthritis in men affecting 1-2% of adults in Western countries, with male to female ratio of 3.6:1. It is rare in pre-menopausal women and its incidence and prevalence increases with age.
Gout is an inflammatory syndrome caused as a response to monosodium urate monohydrate crystals (MSUM) formed in humans in the presence of having elevated serum urate concentration what is known as hyperuricemia. Hyperuricemia is defined as serum urate levels above 6.8mg/dl (≥ 400µmol/L) which is the level above which the physiological saturation threshold is exceeded.
The current increase in the prevalence of gout is related to overweight, of metabolic syndrome & change in our diet with high intake of meat, seafood, fructose sweetened beverages and beer, in addition to the increase in life expectancy. But, the main reason is related to the renal uric acid hypo-excretion, due to genetic and environmental factors such as diuretic use, low dose of aspirin and high alcohol consumption.
Stages of Gout
- Asymptomatic hyperuricemia with elevated uric acid but no clinical gout.
- Acute gout with acute inflammation and intervals between flares.
- Advanced chronic gout with long-term gouty complications of uncontrolled hyperuricemia.
Serum uric acid is determined by
- Dietary purine intake.
- Cellular degradation of purines to urate
- Urate excretion from body via intestines and kidneys.
Urate saturation above 6.8 mg/dl can lead to monosodium urate crystals
- Induce painful inflammatory responses.
- Grow into tophi.
- Precipitate erosive joint damage over time (Table 1).
Clinical |
Score |
Ankle or midfoot |
1 |
First MTP joint |
1 |
Characteristic episodes erythema, ulceration, unbearable to touch, difficulty walking) |
+1 up to+3 |
Episode time frame |
One typical +1, Recurrent +2 |
Tophus present |
4 |
Laboratory Serum urate |
less than 4:-4, 6-8mg :2, 8-10: +3, Equal or more 10mmg/dl:+4 |
Synovial fluid analysis |
MSU negative: -2 |
Imaging |
Urate deposition detected : +4, Presence of gout-related joint damage: +4 |
Table 1 2015 ACR/EULAR Criteria for Classification of Gout l
Diagnosis of gout
Score of 8 or more of ACR/EULAR criteria for classification of gout which consists of:
- Clinical score
- Laboratory: serum urates level score
- Imaging score
Joint aspiration and synovial fluid analysis, gold standard compensated polarized light microscopy
Imaging urate crystal deposits and tophaceous gout:
The crystals deposits can be clearly identified by the use of the dual energy CT imaging or by ultrasound which show double contours punctiform deposits in synovial membrane
- Plain x-ray: insensitive in early disease
- Ultrasound :sensitive in early disease but can be abnormal in asymptomatic hyperuricemia
- CT Scan: sensitive but expensive
- MRI :sensitive but expensive
Common sites of gout:
- Olecranon bursa
- Elbow
- Wrist
- Fingers
- Knee
- Ankle
- Subtalar
- Mid-foot
- First Metatarsophalangeal joint 50% of initial attack & affecting 90% of patients
Differential diagnosis
- Septic arthritis
- Pseudogout
- Cellulitis
- Osteoarthritis first MTP joint or nodal osteoarthritis
- Rheumatoid arthritis
- Psoriatic arthritis, spondylarthropathy
- Lyme disease
Co morbidity checklist for primary care
- Obesity and diet including excessive alcohol intake.
- Modifiable risk factors: hyperlipidemia, hypertension, metabolic syndrome, Type 2 diabetes mellitus.
- Serum urate-elevating medications
- History of urolithiasis
- Chronic kidney disease
- Genetic cause of uric acid overproduction
- Acquired cause of uric acid overproduction: psoriasis, myeloproliferative or lymphoproliferative disease
- Lead intoxication
2012 ACR Gout guidelines
Pharmacologic therapy for the acute flares:
- Supplement with topical ice as needed
- Initiate therapy within 24h of acute flare onset
- Continue pharmacologic rate-lowering therapy during attacks
Mild / moderate pain 1-3 small joints or 1-2 large joints: Monotherpy:
- NSAID: Cox 2 inhibitor has the same efficacy as conventional non-steroidal anti-inflammatory
- drugs
- Systemic corticosteroids : prednisolone greater or equal 0.5 mg/kg/day for 5-10 days
- Colchicines: 1.2 mg initially and 0.6 mg 1 hour later
- Polyarticular or multiple large joint with severe pain: Combination therapy:
- Colchicine + NSAID
- oral corticosteroid + colchicine
- Intra-articular steroids with all other modalities
Patient education after successful outcome:
- Diet and lifestyle triggers: avoid organ meats, high fructose com syrup-sweetened soda and excessive alcohol (more than two drinks per day for men and more than one drink per day for women). Limit beef, lamb, high purine seafood (shellfish) & beer.
- Prompt self-treatment of subsequent attacks
- Urate-lowering therapy (Figure 1)
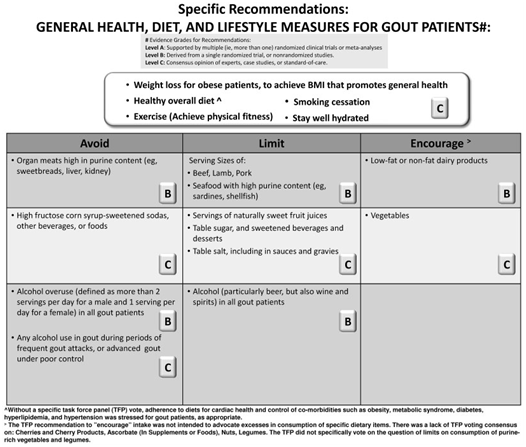
Figure 1 Specific Recommendations: General Health, and Life style measures for GOUT Patients#.
Indications for pharmacologic urate-lowering therapy:
- Tophus or Tophi
- Frequent attacks equal or greater than 2 attacks per year
- Chronic kidney disease: stage 2 or worse
- History of urolithiasis
Current recommendations for urate-lowering Therapy:
- Usual serum urate target is less than 6 mg/dl
- Serum urate levels less than 5 mg/dl may be needed to improve gout signs and symptoms.
Select first-line agent
- Xanthine Oxidase inhibitor : Allopurinol or Febuxostat.
- Probenecid: If xanthine oxidase inhibitor is contraindicated or not tolerated.
Acute Gout Prophylaxis
Allopurinol as first -line urate lowering therapy:
- Effective in uric acid overproducers and underexcretors.
- Starting dosage should be no greater than 100 mg/day for any patient, and start at 50 mg/day in stage 4 or worse CKD (evidence B). Gradually titrate maintenance dose upward every 2–5 weeks to appropriate maximum dose in order to treat to chosen SUA target (evidence C).
- Dose can be raised above 300 mg daily, even with renal impairment, as long as it is accompanied by
- Adequate patient education and monitoring for drug toxicity (e.g. pruritis, rash, elevated hepatic
- Transaminases; evidence B).
- Maximum approved dose 800mg/day (reduced in chronic kidney disease, CKD).
- Intolerance in 5-10%, pruritic rash 2%& major allopurinol hypersensitivity syndrome 0.1-0.4%
Urate lowering therapy: Febuxostat
- Selective inhibitor of xanthine oxidase with nonpurine backbone.
- The dose is 40 mg/day starting dose. Labeled use up to 80 mg/d (ACR guideline allow for doses up to 120 mg/d.
- Advantages: more selective than allopurinol. There is lower renal excretion vs allopurinol active metabolite. No dose adjustment with mild / moderate renal or hepatic impairment.
Urate-lowering Therapy: Uricosurics Increase urate excretion by inhibiting urate reabsorption in the kidney.
Probenecid:
- Alternative in those patients intolerant to at least 1 xanthine oxidase inhibitor.
- Not recommended in persons with history of urolithiasis as it increases urolithithiasis risk especially with acidic urine PH.
- Not recommended if creatinine clearness less than 50ml/min.
Losartan, atorvastatin and fenofibrate are less potent: The use of losartan and fenofibrate alone or in combination with urate lowering therapies can have an extra value in the prevention and management of hyperuricaemia in patients who have both hypertension and dyslipidaemia.
Emerging options in development
- Lesinurad: Selective uric acid reabsorption inhibitor.
- Arhalofenate: Dual-acting anti-inflammatory and urate-lowering therapy.
Gout flare prophylaxis
Initiate with or just before initiating pharmacologic urate-lowering therapy:
- First line: Low dose colchicine (0.5 or 0.6 mg once or twice daily) or Low-dose NSAID (with proton pump inhibitor where indicated).
- Second-line: low -dose prednisone or predinsolone (equal or less 10 mg/day).
If Gout signs / symptoms appear: evaluate gout symptoms with urate-lowering therapy
If No gout signs symptoms appear: Treat with Longest period among the following:
- At least 6 months.
- 3 month after achieving target serum urate level with no tophi.
- 6 months after achieving target serum urate level with greater or equal 1 tophus.
Long-term Management
- Treat to Target serum urate level no higher than less 6 mg/dl.
- If serum urate level achieved then continue gout attack prophylaxis. Regularly monitor serum urate.
- if serum level is not achieved, increase intensity of lowering therapy and reevaluate serum urate.
- Diagnose , treat and prevent acute gout flare.
- identify and manage comorbidities and causes of hyperuricemia.
Take home messages
- Aspirate joint if diagnosis is unclear or septic arthritis is possible
- Use ultrasound or advanced imaging particularly in early disease.
- Initiate pharmacologic urate lowering therapy in all patients with Tophi, multiple attacks /year, CKD stage 2, or higher , or previous urolithiasis
- Prescribe prophylactic anti-inflammatory therapy for at least 6 months hen initiating a pharmacologic urate lowering regimen
- Assess adherence of patients to prescribed regimens.


