Advances in
eISSN: 2377-4290


Case Report Volume 2 Issue 1
Department of Ophthalmology, Shanghai Childrens Hospital, China
Correspondence: Tong Qiao, Department of Ophthalmology, Shanghai Childrens Hospital, 355 Luding RD, China, Tel 86018901600271
Received: January 04, 2015 | Published: January 23, 2015
Citation: Qiao T. Surgical treatment of v-pattern exotropia in crouzon syndrome. Adv Ophthalmol Vis Syst. 2015;2(1):15-19. DOI: 10.15406/aovs.2015.02.00030
Introduction: Strabismus affects as many as 60–70% of patients with Crouzon syndrome. V-pattern strabismus is common and is thought to be secondary to severe oblique muscle dysfunction; the complex motility disorders produced by abnormal extraocular muscles in this syndrome can be difficult to manage. Few studies have reported findings regarding the extra-ocular muscles or how to plan and adapt the required surgery for this condition.
Methods: We retrospectively reviewed the surgical management and outcomes of four patients with Crouzon syndrome who had undergone craniofacial reconstruction surgery.
Results: All patients showed significant improvement in the primary eye position, but had residual ocular motility dysfunction postoperatively, especially relating to the up gaze position. During surgery it was noted that in one of the four patients the lateral or superior oblique tendons were absent or anomalous. In two of the patients there was an absence of the bilateral inferior rectus. The extra-ocular muscles were examined pathologically and revealed evidence of tendon capsule and mild fiber degeneration.
Conclusion: Strabismus in Crouzon syndrome is complex and the absence of certain extra-ocular muscles is unpredictable. It is not possible to perform strabismus surgery according to a defined surgical plan; one needs to adapt according to the patient’s individual anatomy. Also, the strabismus is difficult to completely correct. However, improving ocular motility in the most functional fields of gaze will benefit the quality of life for both children and their families.
Keywords: v-pattern, strabismus, crouzon syndrome
FGFR: fibroblast growth factor receptor genes; FC: finger count; PD: prism diopter ; CM: centimeter; IOOA: inferior oblique muscle(s)
Crouzon syndrome is a rare genetic disorder characterized by the premature closure of one or more cranial sutures and produces the characteristic craniofacial and other associated abnormalities.1,2 It is a craniosynostosis syndrome, caused by a mutation in the fibroblast growth factor receptor 2 gene (FGFR2).3 It has a worldwide prevalence rate of approximately 1 per 20,000 live births.1−4 Craniosynostosis (or craniostenosis) is the premature fusion of one or more cranial sutures. This condition can occur in association with more than 130 different syndromes, but most patients are non syndromic (60% or greater). Crouzon syndrome is the more severe form of craniofacial dysostosis, typically involving multiple cranial sutures. Strabismus is common in patients with craniofacial dysostosis, with as many as two thirds of patients manifesting the condition. V-pattern horizontal strabismus is the most common strabismus.5 To the best of our knowledge, no previous report has reviewed the management of V-pattern horizontal strabismus with marked inferior rectus loss in patients with craniofacial dysostosis. This report documents our experience in the management of four cases of Crouzon syndrome and reviews the anatomical extra-ocular muscle anomalies noted during surgery.
(Table 1) The patients were reviewed sequentially by pediatric neurosurgeons and ophthalmologists. Four cases represented sporadic occurrence in their families. The children were assessed for visual acuity using the E letter matching test if the child was cooperative, and by fixation reflex to “central, steady, and maintained.” if they were not. Alignment was measured in all positions of gaze at 1/3 m and 6 m using accommodation controlling targets. In patients with a short attention span, strabismus was evaluated using the alternative prism cover test. Versions, ductions, and convergence were examined. The anterior segments of each globe were studied using a slit microscope. All children had cycloplegic refraction and fundus pictures were taken using a RetCam II. Strabismus surgery was deferred until craniofacial reconstruction was performed.
Case |
Extraocular muscle finding |
Operation procedure |
1 |
Normal |
First time: an inferior oblique muscle transposition adjacent to the inferior rectus temporal side 2 mm and down 1 mm and a left lateral rectus recession 9 mm from the insertion; after 8 months, a second procedure that resected the left media rectus 6mm and recessed the right superior rectus 5mm. |
2 |
Lacked an inferior rectus muscle, and all of the extra-ocular muscles were atrophic with fatty degeneration of the muscle tendons. |
Bilateral rectus by 10 mm and resected the left medial rectus by 7 mm; an anterior transposition on both the inferior oblique muscles by 3 mm anterior to the ususal site of the inferior rectus insertion. |
3 |
The right superior oblique muscle to be underdeveloped. The left superior oblique muscle and both inferior rectus muscles were absent. |
Recessed the bilateral rectus by 10 mm and resected the left medial rectus by 7 mm, an anterior transposition on both inferior oblique muscles to the inferior rectus supposed insertion(6.8mm distance from limbus),and tucked the right superior oblique muscle by 14 mm. |
4 |
The right inferior rectus muscle was underdeveloped. Both superior oblique muscles were present but the left inferior rectus muscle was absent. |
Recessed the left lateral rectus muscle by 10 mm, and resected the left medial rectus muscle by 6.5 mm, an anterior transposition of the right inferior oblique muscles to the inferior rectus insertion. |
Table 1 Operation findings and procedure in each case
Case 1
A 9-year-old boy was diagnosed with Crouzon syndrome, and accepted for craniofacial reconstruction 1 year ago. He had normal intellectual capacity with vision of 8/100 in his right eye, and Finger Count (FC)/40 centimeter (CM) in his left eye. Both retinal discs, observed during a fundus examination, were pale. Alignment showed V-pattern exotropia with bilateral inferior oblique muscle overaction, accompanied by torsional nystagmus and a right head tilt of 25 degrees. The primary alignment was 30 prism diopter (PD) exotropia. We performed an inferior oblique muscle transposition adjacent to the inferior rectus temporal side 2 mm and down 1 mm and a left lateral rectus recession 9 mm from the insertion. During the procedure, we discovered that all of the extra-ocular muscles were present but attenuated. At the 8 month follow-up the patient still had a left head tilt of about 20 degrees. We performed a second procedure that resected the left media rectus and recessed the right superior rectus. Results are shown in (Figure 1).
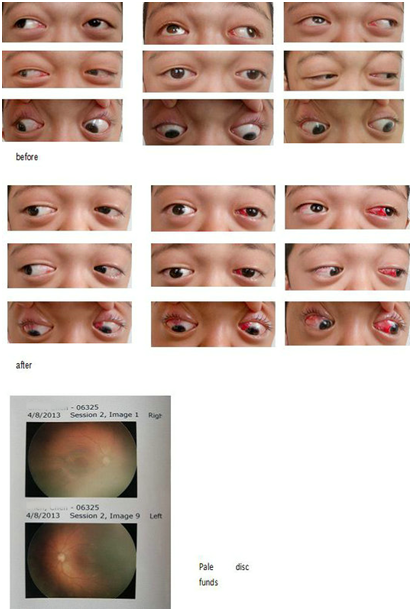
Figure 1 Case 1 showed orthotropia in the primary position, and the inferior oblique muscle overaction changed from +++ to +, head tilt changed from 25 degrees to 5 degrees, and nystagmus did not change.
Case 2
A 6-year-old boy was diagnosed with Crouzon syndrome, and accepted for craniofacial reconstruction 1.5 years ago. He had normal intellectual capacity with vision of 60/100 in both eyes with normal refraction and normal retinal discs. Alignment showed V-pattern exotropia with marked overreaction in the bilateral inferior oblique muscles. The primary position alignment was 110 PD exotropia. During surgery we discovered that both eyes lacked an inferior rectus muscle, and all of the extra-ocular muscles were atrophic with fatty degeneration of the muscle tendons. To treat the horizontal strabismus, we recessed the bilateral rectus by 10 mm and resected the left medial rectus by 7 mm. We performed an anterior transposition on both the inferior oblique muscles by 3 mm anterior to the usual site of the inferior rectus insertion. This patient was followed-up after 6 months. Results are shown in (Figure 2).
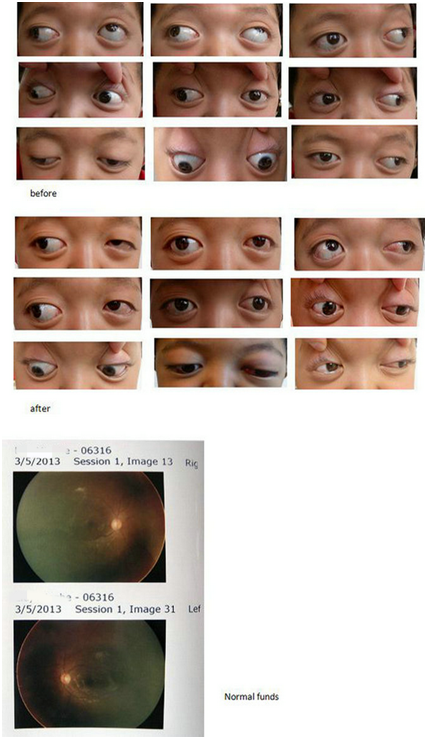
Figure 2 Case 2 had -5 PD in the primary position, and the inferior oblique muscle overaction changed from ++++ to ++; both eyes had the ability to gaze downward.
Case 3
A 3-year-old girl with Crouzon syndrome was accepted for craniofacial reconstruction 1 year ago. Due to her age, she was unable to be tested by the E letter-match test. Her visual acuity was central, steady, and maintained. Both retina pictures showed tortuous retinal vascular. The primary position alignment was 90 PD exotropia with large V-pattern exotropia, and deficiency in downward movement in both eyes. During the surgery, we explored the extra-ocular muscles and found the right superior oblique muscle to be underdeveloped. The left superior oblique muscle and both inferior rectus muscles were absent. To treat the horizontal strabismus, we recessed the bilateral rectus by 10 mm and resected the left medial rectus by 7 mm. We performed an anterior transposition on both inferior oblique muscles to the inferior rectus supposed insertion (6.8mm distance from limbus), and tucked the right superior oblique muscle by 14 mm. This patient was followed-up after 6 months. Results are shown in (Figure 3).
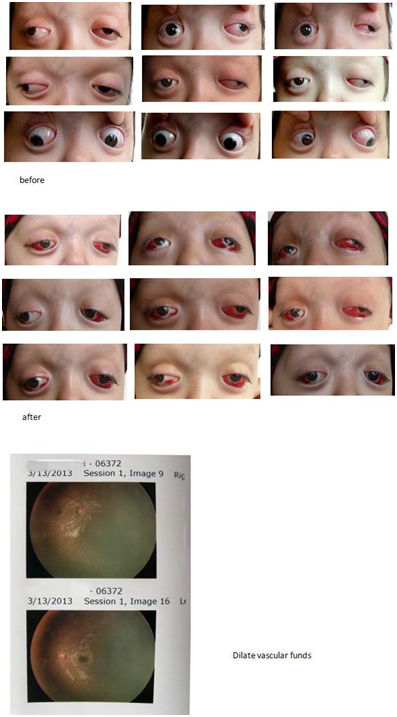
Figure 3 Case 3 had -10 PD in the primary position, and the inferior oblique muscle overaction changed from ++++ to ++; both eyes had the ability to gaze downward. There was no improvement in eyesight over 6 months.
Case 4
A 7-year-old girl with Crouzon syndrome was accepted for craniofacial reconstruction 2 years ago. Visual acuity was 50/100 in both eyes. The primary position alignment was -50 PD with large V-pattern exotropia, and limited downward movement in both eyes. During surgery we explored five extra-ocular muscles and found that the right inferior rectus muscle was underdeveloped. Both superior oblique muscles were present but the left inferior rectus muscle was absent (Figure 4). We recessed the left lateral rectus muscle by 10 mm, and resected the left medial rectus muscle by 6.5 mm to treat the horizontal strabismus. We also performed an anterior transposition of the right inferior oblique muscles to the inferior rectus insertion. This patient was followed-up after 2 months. Results are shown in (Figure 5).
Postoperative |
Preopreative |
|||||||||||||||
Case Number |
Primary Position |
Parttern |
IO |
10:20 |
SO |
10:20 |
IR |
10:20 |
Primary Position |
Parttern |
IO |
10:20 |
SO |
10:20 |
IR |
10:20 |
OD |
OS |
OD |
OS |
OD |
OS |
OD |
OS |
OD |
OS |
OD |
OS |
|||||
1 |
XT 30pd |
V60pd |
2+ |
3+ |
1- |
2- |
NR |
NR |
Ortho |
V10PD |
NR |
1+ |
NR |
NR |
NR |
NR |
2 |
XT 110pd |
V80pd |
2+ |
4+ |
1- |
4- |
3- |
4- |
Ortho |
V40pd |
NR |
2+ |
NR |
1- |
1- |
2- |
3 |
XT 90pd |
V60pd |
NR |
4+ |
1- |
4- |
2- |
4- |
XT-10pd |
V5pd |
NR |
1+ |
NR |
2- |
1- |
2- |
4 |
XT 50pd |
V40pd |
4+ |
NR |
2- |
NR |
2- |
4- |
Ortho |
V10pd |
NR |
NR |
1- |
NR |
1- |
4- |
Table 2 Preoperative and postoperative data
Octave Crouzon first described the hereditary syndrome of craniofacial synostosis, which includes a triad of skull deformities, facial anomalies, and exophthalmos collectively known as Crouzon syndrome.1,2 Early fusion of a single suture is typically an isolated sporadic event, rarely due to a genetic mutation. Patients with syndromic craniosynostosis due to genetic mutations often manifest multiple suture fusions, or pan-suture synostosis, along with other physical abnormalities such as syndactyly and brachydactyly. The most frequently encountered craniosynostosis syndromes are the Crouzon, Apert, and Saethre-Chotzen syndromes. The Crouzon and Apert syndromes are secondary to mutations in fibroblast growth factor receptor genes (FGFR), either gene 2 or 3. To date more than 15 mutations are associated with Crouzon syndrome. Ocular and visual system abnormalities occur much more frequently in patients who have coronal suture synostosis (uni-or bilateral) and/or skull base suture synostosis.
Patients with coronal suture synostosis, syndromic or nonsyndromic, commonly experience a characteristic V-pattern strabismus with a large exotropia during upward gaze, which diminishes in downward gaze. This is often accompanied by apparent overaction of the inferior oblique muscle(s) (IOOA), with possible superior oblique under action. This apparent oblique dysfunction occurs ipsilateral to the fused coronal suture. This leads to hypertropia of the involved eye that becomes worse in adduction in cases of unilateral unicoronal suture fusion, and in cases of asymmetric bilateral coronal suture fusion.7 Our approach to the horizontal strabismus varied in each case due to their individual muscle abnormalities. In Case 1, there was exotropia in primary position. We performed a standard surgical amount with a resultant residential exotropia. This was followed with further surgery of resection of the left media rectus which eventually achieved a satisfying outcome. In Case 2, we performed bilateral rectus recession and media rectus resection to achieve a good outcome. In Case 3, the amount of horizontal squint was less than Case 2, but the muscle was underdeveloped. We performed identical surgery as Case 2, but unfortunately the girl still had residential exotropia of about 10 PD. If the parents agree, we plan to perform a further procedure on the left media rectus. In Case 4, we performed horizontal strabismus surgery and an anterior transposition of the right inferior oblique muscle, achieving a good outcome for the primary position of the eye and relief of head tilt. From these four cases it seems that there is no standard surgery to treat strabismus in Crouzon syndrome. In most cases require a significant amount of surgery, especially when abnormal development of the extra-ocular muscles exists. Compared to normal extra-ocular muscles, the muscles of Crouzon patients have pathological changes consistent with collagen degeneration (Figure 5). The proptosis contributes to collagen degeneration. During surgery, we also found that the tendon capsule was thicker than normal, and in some cases, the lateral rectus muscle had fused to the sclera (Figure 6).
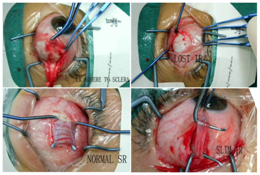
Figure 6 The proptosis contributes to collagen degeneration. During surgery, we also found that the tendon capsule was thicker than normal, and in some cases, the lateral rectus muscle had fused to the sclera.
Most ophthalmologists admit that the reasons for the apparent oblique dysfunction are multifactorial. First, orbital extorsion causes secondary globe extorsion, with extra-ocular muscle displacement (medial rectus muscles are offset superiorly, acting as elevators in adduction, mimicking IOOA). Second, superior orbital rim retrusion with secondary retrusion of the superior oblique trochlea causes true superior oblique underaction and secondary IOOA. Lastly, there are anomalous pulleys, anomalous extraocular muscle insertions and/or extraocular muscle agenesis. In our cases we found that the inferior rectus was abnormal to a greater extent than the superior oblique muscle. Reviewing the pictures prior to surgery, we found that the large V-pattern exotropia affecting the downward movement of the eye was due to under-action. In Case 2 we initially observed absence of the inferior rectus muscle and we conservatively placed the inferior oblique muscle into the inferior rectus supposed insertion (6.8mm distance from limbus). In Case 3, when the same absent inferior rectus muscle was encountered, we performed an anterior-transposition of the inferior oblique muscle, 3.8 mm distance from limbus. After surgery, the parents were pleased to see their child’s eyes could move down. This is the first report of an inferior rectus defect in Crouzon syndrome. We believe that it is necessary to explore all of the vertical extra-ocular muscles when the strabismus in Crouzon syndrome is large and unusual (Figure 5).
In the four cases outlined, the outcome of strabismus surgery was improved in patients with a less complex strabismus, and better visual acuity. Visual acuity level was an important reason influence on the outcome of the strabismus surgery. The better the visual acuity, the better the result. To improve outcome, it is beneficial to perform early craniofacial reconstruction, to reduce the intracranial pressure, correct the refraction and treat amblyopia. For the treatment of vertical strabismus, we discuss the surgical management options for the apparent oblique and/or vertical rectus muscle dysfunction. In general, patients with non-syndromic unicoronal synostosis have improved chances for normal alignment and fusion postoperatively, often after simple inferior oblique weakening procedures. In contrast, patients with syndromic craniosynostosis and complex strabismus are difficult to align. No single surgical procedure reliably treats the V-pattern, or the apparent inferior oblique overaction and hypertropia in side gaze. Options for surgical correction include inferior oblique weakening, inferior oblique anterior-positioning, inferior oblique anteropositioning, nasal inferior oblique fixation to the orbital wall, vertical offsets of the horizontal muscles, medial rectus offset downward and lateral rectus offset upward, horizontal offsets of the vertical muscles, superior rectus offset temporally and inferior rectus offset nasally, and the superior oblique tuck.8−11 There is no one correct plan before surgery. With all of the options in mind, we need to adjust our surgical management according to the results of our surgical exploration and identification of the extra-ocular muscles.
Attention to diagnosis and treatment of amblyopia and strabismus are necessary to preserve vision in craniosynostosis patients. In our patients, we concluded that the better the vision acuity, the better the outcome. Better vision acuity resulted from early diagnosis and early cranioplasty surgery to lower the IOP and eliminate papilledema. Considering Case 1, the poor visual acuity and nystagmus was secondary to optic nerve atrophy. Orbital imaging may aid in planning the surgery for patients whose strabismus remains a challenge. However, MRI testing may not be possible due to metallic components of the craniofacial reconstructive surgery. In these cases, surgical exploration and identification of the extraocular muscles becomes more valuable in the planning process.
None.
Author declares that there is no conflict of interest.

©2015 Qiao. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.