Advances in
eISSN: 2377-4290


Case Report Volume 13 Issue 1
1Former Head of Department of Ophthalmology, Ivrea Hospital (Turin, I), Italy
2Department of Ophthalmology, Koelliker Hospital Turin (I), Italy
3Head of Department of Histopathology, Ivrea Hospital (Turin, I), Italy
4Head of Department of Otolaryngology, Regina Margherita Hospital (Turin, I), Italy
5Head of Department of Ophthalmology, Chivasso Hospital (Turin, I), Italy
Correspondence: G Vadalà, Head of Department of Ophthalmology, Chivasso Hospital (Turin, I), Italy
Received: November 16, 2022 | Published: February 1, 2023
Citation: Bauchiero L, Monteu F, Orlassino R, et al. Silicone nasolacrimal intubation: our experience in long term cases. Adv Ophthalmol Vis Syst. 2023;13(1):15-18. DOI: 10.15406/aovs.2023.13.00432
Purpose: To evaluate the bicanalicular tube structural integrity and the anatomical and functional post operative results of cases of long and very long bicanalicular intubation (from 2 to 13 years).
Methods: We studied all the patients of our Department with long-lasting intubation (greater than one year), from 2000 to 2021. We obtained an histocytological evaluation of the material of intubation and a nasal endoscopy. We investigated the causes of the long permanency and the patient tolerability.
Results: In our study, 6 eyes from 5 patients (4 women and 1 man) underwent a nasolacrimal duct intubation. The mean intubation permanency time was 6.8 years and the median value was 7 years (minimum 2 years, maximum 13 years). The bicanalicular tube examinations found traces of mucus made of amorphous protein material, sporadic leukocytes and histiocytes. In all the patients the nasal endoscopy showed good conditions of the middle meatus mucosa.
Conclusions: In complex cases, such as multiple re-operations, inflamed and small lacrimal sac, fibrotic sac, inflamed nasal mucosa for previous nasal pathologies, a permanent silicone tube could be a reasonable choice as it appears to be well tolerated and without major complication risks.
Keywords: nasolacrimal duct intubation, epiphora, patient tolerability
Dacryocystorhinostomy (DCR) is the most commonly used surgery in case of lacrimal drainage obstruction, allowing tears to drain directly via a surgically created low resistance bypass between the lacrimal sac and the nasal cavity. DCR techniques can be ab externo, standard DCR (EX-DCR) or ab interno, endoscopic DCR (EN-DCR).
Beginning in the 1970s, ophthalmologists introduced the use of a silicone intubation, implanted during the end of the surgery.1 The reasons were an increased postoperative patency rate because of maintenance of the opening of the ostium.2 However, other studies reported a higher failure rate when using a silicone stent because of granulomatous inflammation.3 The role of silicone intubation during DCR surgery has been discussed several times in the recent literature, with conflicting opinions.4–8 There is no uniformity of opinions also on the permanence of the intubation. Some Authors prefer not to use it, while others maintain it up to 6 months, with a mean from 2 weeks to 2 months.9–16 There are only few studies regarding tissue alteration after prolonged intubation and silicone tube intactness, as the one reported by Mimura et al, who studied a neglected silicone tube in lacrimal duct for 20 years.17 Purpose of our study is to analyze the silicone tube conditions and the anatomic and functional post operative results, in cases of long and very long maintenance of bicanalicular intubation (from 2 to 13 years).
We analyzed all the patients of our Department who underwent DCR from 2000 to 2021 and we selected all the long-lasting intubations (greater than one year), finding 6 cases (0.47% of all the surgeries performed).
During 13 years of follow up, 6 eyes from 5 patients (4 women and 1 man) underwent a nasolacrimal duct intubation for persistent epiphora in nasolacrimal duct obstructions. The mean age was 62 years old at the age of the surgery (from 48 to 72) and all the patients had postsac obstructions, confirmed by dacryo-CT (computerized tomography dacryocystography). All included patients underwent EX-DCR, which was performed by the same oculoplastic surgeon. One procedure was performed under general anaesthesia (a patient with trisomy 21), while the remaining 4 were performed under local anaesthesia. Surgery involved a complete opening of the lacrimal sac and suturing of anterior and posterior flaps. FCI Ophthalmics, BIKA stent was the bicanalicular silicone tube used (a silicone tube connected by each of its extremities to two malleable metallic probes by secure crimping process; silicone tube: 300 mm long, 0.94 mm diameter; metal probes: 53 mm long, 0.80 mm diameter).
Follow up examinations were performed at 7 and 30 days post procedure. Then, they continued at six-month intervals thereafter until the end of the study. The follow up consisted in ophthalmic examination, fluorescein dye disappearance test, nasolacrimal irrigation and slit lamp imagines acquisition. Patients were also asked to subjectively report their symptoms as none, mild, moderate or unchanged at each visit (foreign body sensation, watering eyes, ocular pain, ocular discomfort, other). After the intubation removal, the last follow up consisted in the nasal endoscopy, the slit lamp imagines acquisition and the histocytological study of the tube material, collected by our Histopatology Department. Then, we assessed the mean and the median intubation permanency, the causes of the long intubation time, the conditions of the intubation material and the functional and anatomical result of the surgery (lacrimal patency to irrigation test). Our Department obtained the Ethical Standards Board approval for this study (written informed consent signed by the patients / guardians, included the consent for the use of clinical photographs that permit identification of the patient). The research adhered to the tenets of the Declaration of Helsinki.
The mean intubation permanency time was 6.8 years (minimum 2 years, maximum 13 years), the median value was 7 years. The causes of the long intubation permanency were:
As regard the functional results, all of the patients had lacrimal patency to irrigation and fluorescein dye disappearance test grade 0-1 at the last follow up visit.
During the last follow up visit, regarding the anatomical results, no one showed signs of inflammatory reactions, lacrimal punctum enlargement or tractional dilatation and no one had tube displacement or the burrow of the intubation in the medial canthus. One patient shown a mild inferior lacrimal punctum hypertrophy (EX-DCR with BIKA implantation performed 7 years before) (Figure 1). All of the patients reported their symptoms were none and referred absence of discomfort during all of the follow up. The nasal endoscopy, performed by the same otolaryngologist of our Department, shown in all of the patients good conditions of the middle meatus mucosa and of the ostium (Figure 2, Figure 3).As regard the histocytological study, we submitted the intubation material to the Anatomic Pathology of our Department. In one case, mucous matter was found at the entrance of the puncta (Figure 4). In another case, whitish material was found inside of the intubation. The anatomic pathologist argued that the material could be entered by retrograde obliteration or by fissuration of the tube wall and micro infiltration consequently. The whitish substance was made of amorphous protein material, sporadic leukocytes and histiocytes. The lumen of the intubation was partially obliterated (70% of the lumen) (Figure 5 and 6).

Figure 1 Mild inferior lacrimal punctum hypertrophy (EX-DCR with BIKA implantation performed 7 years before).

Figure 2 Nasal endoscopy, proving the good conditions of the middle meatus mucosa and of the ostium, before and after BIKA removal.
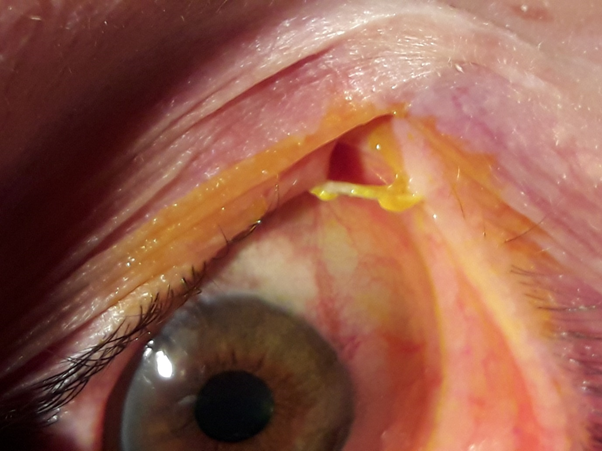
Figure 4 In a female patient, who maintained BIKA for 3 years, mucous matter was found at the entrance of the puncta.
In 2017, a recent meta-analysis indicated that the use of a silicone tube did not increase the risk of tissue granulation, infection or adhesion. In literature, the common complications after DCR were intranasal tissue granulation, adhesion, infection, haemorrhage and some complications were considered to be related with silicone tube, including punctual/canalicular laceration, tube displacement or loss and conjunctival irritation.6,18 The opinion that the silicone tube itself may stimulate tissue granulation, however, was controversial.19 suggested that silicone intubation as a foreign inorganic material may predispose the patient to granulation formation with subsequent rhinostomy closure. The ostial size reduction has been reported by Longari et al. in higher percentage in the stent group, mainly due to peristomal granuloma, scar tissue formation, and turbinoseptal synaechia.20 In 2013, Rather and Singh21 conducted a large, randomized controlled trial and demonstrated that silicone intubation in DCR prevented the closure of the ostium, thereby enhancing the success rate of DCR.22 When comparing the clinical effectiveness of recanalization with extubation in 3 months or without silicone intubation, found no statistically significant differences. At the same time, Veloudios A et al.23 studied the structure and time of complications during lacrimal tract intubation in 82 patients with follow-ups from 3 to 66 months and concluded that prolonged intubation is quite safe.
A 2006 study about silicone stent retained on a permanent basis,24 valued that the main reason for the removal of the silicone tube was tube-related complication itself, rather than insufficient efficacy of the tube and that the most common complication was tube-related canaliculitis. In our cases series, there weren’t complications as adhesions, ostial size reduction, infections, canaliculitis or tube displacements. The inferior lacrimal punctum hypertrophy and the whitish mucous matter find could be related to the tissue chronic reaction to the silicone tube, but they didn’t cause complications or dangerous tube stenosis. Obviously, the major limitation of the study was the small sample. It is so possible that the reason our series did not report ostial size reduction is because of the small number of patients. On the other hand, it is also possible that our series represents a subset with extremely good tolerance of intubation, and there is actually a higher prevalence of ostial size reduction if all patients (including those with tubes removed much earlier) are included. Furthermore, the group analyzed is rather heterogenous and includes patients with problems (revision surgery, excessive inflammation post-op) and without problems (the patients who were satisfied and that was the reason why the tube was retained).
The reasons for the long permanence were explained by the complicated cases or by patient choice. For these motivations, we can state that in complex cases, such as multiple re-operations, inflamed and small lacrimal sac, fibrotic sac, inflamed nasal mucosa for previous nasal pathologies, a permanent silicone tube could be a reasonable choice. On the basis of our results, it can be stated that the tolerability of long and very long-lasting intubation is excellent, with surgeon and patient satisfaction. In such cases, it is essential to carefully check at least once a year that the lacrimal puntum does not show signs of enlargement or tractional dilatation and especially that the intubation extrusion, canalicular laceration or the burrow of the BIKA in the medial canthus does not occur. Otherwise, in the event this happened, the surgical removal will be mandatory.
None.
The authors declare that there are no conflicts of interest.
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.

©2023 Bauchiero, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.