Advances in
eISSN: 2377-4290


Clinical Report Volume 13 Issue 1
Private Eye Center, Argentina
Correspondence:
Received: January 07, 2023 | Published: January 20, 2023
Citation: Martelli L. Recurrent craniopharyngioma. Adv Ophthalmol Vis Syst. 2023;13(1):11-13. DOI: 10.15406/aovs.2023.13.00431
Craniopharyngioma is a rare embryonic malformation tumor in the sellar and parasellar area of low histological grade. Local recurrence is frequent, being of great importance the use of the preoperative visual field as a clinical predictive indicator; and its postoperative outcome. The objective of this report is to recognize a recurrence in the event of small changes in visual acuity or campimetric alterations in patients with a history of this tumor.
Clinical case: A 10-year-old girl presents to the clinic with a history of craniopharyngioma operated on a year earlier, with both atrophic optic nerves and decreased visual acuity. Complementary studies and urgent referral to the pediatric neurosurgeon were carried out, who detected intracranial hypertension secondary to recurrence of the craniopharyngioma, leading to its surgical removal.
Conclusion: It is important to highlight the requesting of a visual field both for the detection of possible recurrences and for the follow-up of the craniopharyngioma, considering its high recurrence rate.
Keywords: craniopharyngioma, recurrence, intracranial hypertension
A 10-year-old-pacient consulted our center accompanied by her mother, due to a clinical picture of one week of evolution characterized by decreased visual acuity. Manifesting according to family with a notable change in writing. She used to do it in an organized and linear way on lines of school paper, and as the days went by she began to write in a disorderly way, altering its alignment. Due to this, she decided to consult (Figure 1). She has a history of craniopharyngioma surgically removed a year before, with onset of symptoms similar to those that led to the new consultation.The ophthalmological examination showed best corrected visual acuity (BCVA) of 20/400 in both eyes (AO), biomicroscopy of the anterior segment without particularities, without relative afferent pupillary defect (RPD). Intraocular pressure (IOP) 10 mmHg in both eyes. Fundus examination (FO) showed bilateral papilla atrophy without evident papilledema.Optical coherence tomography (OCT) was performed, revealing atrophy of both optic nerves with alteration of the nerve fiber layer (Figure 2). The visual field presented decreased bilateral retinal sensitivity, with remnants in the upper nasal quadrant, greater in the left eye (Figure 3). Given this condition, brain imaging and consultation with the neurosurgery service were requested. Comparing with previous magnetic resonance imaging (MRI), a slight increase in the size of the expansive lesion was observed, predominantly cystic in the sellar/suprasellar region, with solid marginal areas, with the presence of peripherally distributed calcifications and enhancement of its solid portion after administration of contrast.
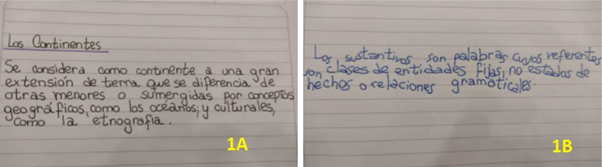
Figure 1 Patient's writing, 1A) One month before the consultation, 1B) One week before the consultation.

Figure 3 Computerized visual field (preoperative) decreased bilateral retinal sensitivity with superior nasal remnant in the left eye.
That lesion partially compressed the 3rd ventricle, displaced the optic chiasm anteriorly and extended posteriorly occupying the interpeduncular and prepontine cistern. Associated with a small hyperintense nodular image on T1 at the level of the 3rd ventricle (Figure 4). Considering the clinical picture, the changes in the MRI and its history, it was interpreted as a recurrence of Craniopharyngioma. In conjunction with neurosurgery, surgical removal of the tumor was decided, with placement of a ventriculoperitoneal shunt valve. Systemic treatment with corticosteroids, hormone replacement drugs and external radiotherapy was established. After a year, she attended a new ophthalmological control, presenting cushingoid facies. On examination, BCVA was 20/40 in both eyes. She presented exotropia, with hypertropia of the left eye with limited infraduction (Figure 5). She preserved photomotor and consensual pupillary reflex in the right eye, while in the left eye she manifested areactive mydriasis. On examination of the fundus, bilateral papilla atrophy was observed (Figure 6). The visual field also showed clinical improvement, with sequelae bitemporal heteronymous hemianopsia (Figure 7). The OCT did not present significant changes in the fiber layer (Figure 8). The axial section of the nuclear magnetic resonance showed, on T1 sequence, that an area with a sequelae aspect persisted at the level of the center-medial nucleus of the left thalamus, interpreted as evolving ischemia (Figure 9).
Craniopharyngioma is a rare embryonic malformation tumor in the sellar and parasellar area of low histological grade.1 They represent 4% of intracranial tumors in childhood2 with a bimodal distribution, with the highest incidence in ages 5-14 years and being able to present in adulthood between 50-74 years.1 It is a chronic disease that requires interdisciplinary monitoring due to its clinical consequences.3 The clinical manifestations generally correlate with the size and location of the lesion and its pattern of slow growth. One of the main reasons for consultation is headache in 60-75%, secondary to increased intracranial pressure.4 However, the close relationship of the tumor with the anterior visual pathway produces variable campimetric alterations2 in 68-84%. Repka et al.5 found that 17% of patients had vision of 20/40 or worse in the better eye at diagnosis and 27% continued to have the same or worse visual acuity in the better eye postoperatively.6 For this reason, difficulties in seeing the blackboard at school or sitting closer to the television are also brought to the consultation.4 Patients usually present visual impairment, increased intracranial pressure, and between 40-80%, dysregulation of at least one hypothalamic-pituitary axis at the time of diagnosis.7 They usually have a high survival rate, around 92% 3 and benign histological classification,5 however, recurrence ranges from 9% to 51% of cases.8 Its morbidity depends mainly on the compromise of adjacent structures, such as the optic chiasm, pituitary gland or hypothalamus, causing different degrees of hormonal alterations, metabolic syndrome and secondary complications.9
Visual manifestations are more significant in recurrences compared to the primary tumor.8 Therefore, it is extremely important to control visual acuity and visual field before surgery, as well as the eye fundus to detect papilledema or optic atrophy.8 Preoperative campimetry is a prognostic indicator of the final visual outcome. There is an association between a greater initial campimetric compromise and an increase in the recurrence rate, so strict control is recommended.6 The most frequent campimetric alterations are bitemporal hemianopsia, lower quadrantanopia or visual field constriction due to compression of the optic chiasm and bilateral optic atrophy.2 Computed tomography (CT) classically shows a heterogeneous suprasellar mass with calcification and extension to the chiasm or third ventricle. However, calcification may be absent in adults. Magnetic resonance imaging (MRI) is more sensitive for detecting cystic components and delimiting the extent of the tumor.
The exact location of the tumor will determine the surgical plan. When possible, a radical treatment with complete resection of the same is performed.3 While when it affects neighboring structures, conservative treatment is preferred9 with subsequent application of local radiotherapy.3 This reduces the chances of recurrence from 71-91% to 21% at 5 years of follow-up.9 This is why it can be considered part of the standard treatment. However, due to the complications derived from external radiotherapy, variants arose with the aim of preserving the surrounding tissue, and with it the endocrinological function and the visual pathway. Then, fractionated three-dimensional conformal radiotherapy, modulated intensity, fractionated stereotactic or proton beam therapy are used. There is currently no consensus regarding treatment, so each individual case should be considered.10 On the other hand, close radiological follow-up of patients is of the utmost importance, which allows for the detection of recurrences at an early stage.11 Most are diagnosed during the first 3 to 4 years after initial treatment. For this reason, in this paper we propose the importance of including ophthalmological follow-up, especially considering the visual field as a minimally invasive strategy.
Craniopharyngioma is a rare tumor, but with a high recurrence rate. Therefore, a strict follow-up of the patient with a history of this pathology must be carried out. Emphasizing interdisciplinary work. Likewise, we want to emphasize the mother's story in the consultation and how subtle changes in writing can lead us to the diagnosis if we do not underestimate them. Despite presenting signs of chronicity or not having findings that justify an acute visual loss in the fundus, it is extremely important to request a visual field, since it gives us direct information on the state of the optic pathway throughout its entire journey.
None.
The author declares there are no conflicts of interest.

©2023 Martelli. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.