Advances in
eISSN: 2377-4290


Case Report Volume 14 Issue 2
Hopital militaire dinstruction Mohammed V, Morocco
Correspondence: Yonli yempabou Hugues Arnaud, Hôpital militaire d’instruction Mohammed V-Rabat, Morocco, Tel +212634095590
Received: August 01, 2024 | Published: August 21, 2024
Citation: Jeddou I, Brarou H, Yaya-Oye DA, et al. Multivisceral metastases from choroidal melanoma: a case report. Adv Ophthalmol Vis Syst. 2024;14(2):71-73. DOI: 10.15406/aovs.2024.14.00467
Aim: To describe a case of choroidal melanoma metastasis.
Case presentation: This is a case of a 39-year-old female patient diagnosed with choroidal melanoma of the right eye. Initial extension exam was negative; treatment consisted of enucleation of the tumor. The patient was subsequently lost. The evolution was marked by the appearance of multivisceral metastasis which were diagnosed at re-evaluation. The patient died after a short treatment of chemotherapy.
Conclusion: choroidal melanoma is a rare disease with a severe prognosis that requires appropriate treatment and regular follow-up.
Keywords: metastases, melanoma, choroid
Choroidal melanoma is the most common intraocular tumor, accounting for around 80% of cases. But it remains rare. However, the occurrence of metastases is frequent and constitutes the main prognostic factor.1 We report a case of melanoma in a 39-year-old female patient with multivisceral metastases.
The patient was 39 years old and had no personal and familial history of melanoma. She was consulted for a decrease in visual acuity of 03/20 in the right eye and 20/20 in the left eye. Examination with a light biomicroscope was normal in both eyes. Retinophotography revealed a suspicious mass in the superior temporal region of the right eye with retinal pallor associated with venous tortuosity (image not available). Examination of the left eye was normal. B-mode ultrasound revealed a hyperechoic dome-shaped choroidal mass with retinal detachment in the right eye (image not available).
Imaging was complemented by orbitocerebral MRI, which revealed a suspicious mass in hyposignal T1 and hypersignal T2, with gadolinium uptake, suggesting in the first instance a choroidal melanoma to be correlated with anatomopathological data. The patient's extension work-up at the diagnostic was negative (cerebral, lung and hepatic scan) (Figure 1).
Very suggestive of choroidal melanoma
The diagnosis of choroidal melanoma was made on the basis of fundus examination, B-mode ultrasound and orbito-cerebral MRI. The diagnosis was confirmed by histology.
Treatment was enucleation of the right eye with patient consent because enucleation is the only therapy available in our environment (Figure 2).
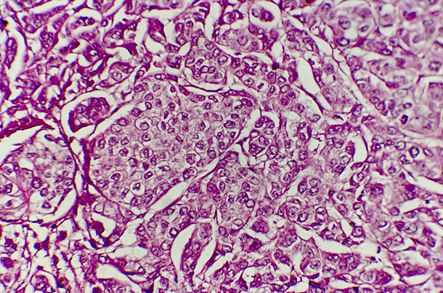
Figure 2 Histological examination of the excisional specimen found a brownish lesion measuring 12mmX10mm+ Tumor proliferation of essentially spindle-shaped architecture with anisokaryotic and strongly nucleated nuclei in favor of a choroidal melanoma.
The first examination at 48 h post-operatively and the second one month later were normal.
Post-operative management was aimed at fitting an ocular prosthesis, treating post-surgical complications and detecting metastases at an early stage. No adjuvant treatment had yet been decided at this stage.
The patient was subsequently lost one month after surgery.
On re-evaluation, the patient was found to be in poor general condition, with weight loss not quantified, asthenia and a chronic cough that had been evolving for a year.
Imaging was ordered and multivisceral metastases were noted: hepatic, pulmonary and vertebral.
Figures 3–5: Presence of multivisceral metastases with choroidal location as the primary tumor CT-detected.
The diagnosis of primary choroidal tumor metastases was suspected by the absence of any other primary cancer site, then confirmed by pathological examination.
Chemotherapy was started at a rate of 2 sessions per week. After one month of treatment, the patient died of cardiorespiratory arrest as a result of her pathology.
Choroidal melanomas are malignant tumors that develop at the expense of melanocytes in the posterior uvea.2
It is a cancer with a poor prognosis due to its high metastatic potential. The occurrence of metastases depends on several factors: patient age, tumor characteristics and associated chromosomal abnormalities.
Advanced age appears to be a factor with a poor prognosis. This risk increases with age.3 It is partly explained by the numerous comorbidities found at this age. Tumor characteristics include size and histological type. Size is the main prognostic factor. Tumor diameter and thickness are the main parameters concerned. The risk of metastasis is between 10-20% when thickness increases by 5mm, according to the Kaplan and Meier study.4
The tumor's epithelioid histological type and high mitotic power are factors with a poor prognosis.5 Chromosomal abnormalities: monosomy of chromosome 3 and 8, trisomy of chromosome 6 are indicators of poor prognosis.6 In this case, only one poor prognostic factor was found: tumor size, which was 12mmX10mm. The histological type was fusiform with strongly nucleated anisokaryotic nuclei.
Regardless of the therapy used, metastases occurred in 50% of cases ten years after diagnosis.7 The main site of metastasis is the liver in over 89% of cases, followed by the lung and finally the bone. The patient had all three secondary sites.
From the onset of metastases, median survival is between 12-16 months.8,9
However, patients whose metastases are treated have a prolonged survival of a few months compared to patients whose metastases are not treated.10,11
None.
None.
Authors declare that they have no conflict of interest.

©2024 Jeddou, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.