Advances in
eISSN: 2377-4290


Case Report Volume 2 Issue 6
Complejo Hospitalario de Cáceres, Spain
Correspondence: Elena Rodriguez Neila, Complejo Hospitalario de Cáceres, Avda de Espana, 2.10004, Spain, Tel 0034 670599221
Received: July 03, 2015 | Published: August 5, 2015
Citation: Neila ER. Harada disease versus central serous corioretinopathy. Adv Ophthalmol Vis Syst. 2015;2(6):184-188. DOI: 10.15406/aovs.2015.02.00065
Harada's disease is an acute inflammatory, immune-mediated disorder that typically affects both eyes of middle aged adults. Melanocyte-containing organs such as the skin, ear, meninges, and eye can be involved. Acute exudative panuveitis occurs in both eyes causing multifocal serous detachment of the retina. A large dose of systemic corticosteroids is a rewarding treatment for a rapid resolution of exudative lesions. Central serous chorioretinopathy (CSC) is a chorioretinal disorder characterized by serous detachment of the neurosensory retina. It can be triggered by steroids. We present two cases of challenging differential diagnosis between Harada disease and CSCR.
Keywords: harada disease, linfocitary meningitis, acute posterior multifocal epitheliopathy, vogt-koyanagi-harada syndrome
CSC: central serous chorioretinopathy; OCT: optical coherence tomography; RPE: retinal pigment epithelium; ILM: internal limiting membrane; VKH: vogt-koyanagi-harada's; PED: pigmentary epithelium detachment; FA: fluorescein angiography; ICG: indocyanine green; EOM: external ocular movements; VA: visual acuity; CSCR: central serous chorioretinopathy
Harada disease is an acute inflammatory, immune-mediated disorder that typically affects bilateral eyes of middle aged adults. Melanocyte-containing organs such as the skin, ear, meninges, and eye can be involved. Acute exudative panuveitis occurs in both eyes and causes ocular inflammation and visual loss. Acute phase of the disease is featured by neurosensory retinal detachments associated to multiple loci of aggressive choroidal exudation. Some patients may present optic disk swelling. A large dose of systemic corticosteroids is a rewarding treatment for a rapid resolution of exudative lesions (Figure 1A).
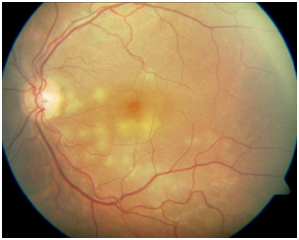
Figure 1A Color Fundus Retinography of left eye shows multiple loci of choroidal exudation in a case of Harada disease.
Multilobular dye pooling with a dark rim on late-phase FA is frequent. Optical Coherence Tomography (OCT) often reveals subretinal septa that divide the subretinal space into several compartments. The subretinal septum lay on the retinal pigment epithelium (RPE) in the foveal area, forming the posterior wall of the subfoveal compartment while it detaches from the RPE in the perifoveal area, which serves as a lateral wall between the subfoveal and perifoveal compartments. The dark rims of each area of subretinal dye pooling correspond to the subretinal septa. Soon after steroid pulse therapy, the subretinal septa resolve completely. Subretinal septa can cause multilobular dye pooling in serous retinal detachment associated with acute VKH disease. We assume that the subretinal septa are comprised of inflammatory products such as fibrin, which usually resolves after steroid pulse therapy.
Most common findings in the acute uveitis stage are: disseminated spotted choroidal hyper fluorescence and choroidal hypo fluorescence. In the chronic uveitic stage: spotted hyper and hypo fluorescence and optic disc hyper fluorescence. In the convalescent stage: spotted hyper and hypo fluorescence and blockage of choroidal fluorescence. Retinal vasculitis is found not very often. A reticular hypo fluorescent pattern with no clinical correlation is found. Swelling obscures the fine granular structure of the fundus and causes typically an intense glisten of the internal limiting membrane (ILM). Vogt-Koyanagi-Harada's (VKH) disease is reported to be closely associated with the HLA class II antigen, HLA-DR4.1
Central serous chorioretinopathy (CSC) is a chorioretinal disorder characterized by serous detachment of the neurosensory retina. CSC occurs most frequently in mid-life and more often in men than in women. Major symptoms are blurred vision, usually in one eye only and perceived typically by the patient as a dark spot in the centre of the visual field with associated micropsia and metamorphopsia. Normal vision often recurs spontaneously within a few months. The condition can be precipitated by stress and hypercortisolism. Ophthalmoscopic signs of CSC range from mono- or paucifocal RPE lesions with prominent elevation of the neurosensory retina by clear fluid – typical of cases of recent onset – to shallow detachments overlying large patches of irregularly depigmented RPE. The spectrum of lesions includes RPE detachments. Granular or fibrinous material may accumulate in the subretinal cavity. Serous detachment often resolves spontaneously (Figure 1B).
The primary pathology of acute CSC is thought to begin with disruption of the choroidal circulation. The RPE then decompensates and allows exudation from the choroidal vasculature to pass into the subretinal space. Detected RPE abnormalities such as a pigmentary epithelium detachment (PED), were within areas of choroidal vascular hyperpermeability. Fundus fluorescein angiography (FA) of acute CSCR typically shows focal leaks at the level of the RPE in 2 main patterns: “smokestack” or “inkblot” RPE dysfunction is also often demonstrable on FFA and indocyanine green (ICG) angiography (Figure 1C).
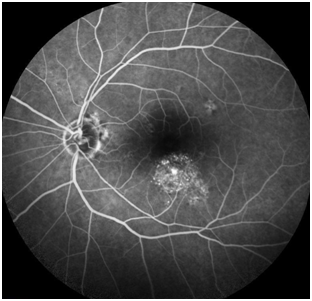
Figure 1C Fundus angiography of left eye shows patches of irregularly depigmented RPE and a focal leak in a case of CSCR.
When the retina is detached, the appearance of the outer retinal layer changed; the external limiting membrane persisted, although the IS/OS could not be detected in all eyes, as recently reported by Ojima et al. In the acute phase, the thickness of the probable photoreceptor outer segment increased in the entire area of the detached retina. The increased thickness of the photoreceptor outer segment in the detached retina then gradually decreased, and the outer segment’s appearancechanged to granular until the reattachment.2
Case 1
Woman of 55 years with Hashimoto´s thyroiditisand diabetes type 2. Previous history of ocular inflammation episode resolved with systemic steroids as concerned. No reports are provided. Presentation is bilateral VA reduction. On examination, objective VA is20/50in her right eye and 20/40 in her left. The anterior segment findings show no cells. The IOP is normal in both eyes. The fundus shows 1+ cell. Foci are seen with serous subretinal septa in the right eye temporal arcades and macular serous detachment in her left eye. And increase of the brightness of internal limiting membrane in the posterior pole of both eyes (Figure 1D&1E). The OCT revealed the presence of septet neurosensorial detachment in the posterior pole of both eyes (Figure1F&1G). The FA shows papillary hyper fluorescence in both eyes, hyper fluorescent lesions in the right eye temporal arcades and hyper fluorescent lesion in the left eye with macular pattern "smokestack" or "umbrella" that recalls the CSCR (Figure 1H&1I). The patient has been treated with systemic steroids, with good ocular response butsevere imbalance of metabolic control of diabetes. During the decreasing doses of steroids has been a resurgence of clinical state. Cerebral magnetic resonance imaging (MRI) was performed in case Adalimumab was indicated. Cortical demyelination and white matter pathologic changes were detected. Neurology Service evaluated the patient. Adalimumab was not recommended after MRI findings.
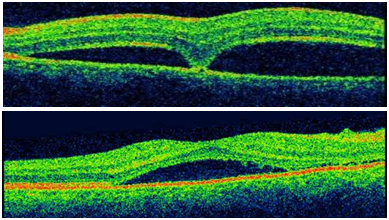
Figure 1F & 1G OCTs showing macular detachment in both eyes. Notice that in the right eye the detachment is tabicated.
Systemic steroids treatment was reinitiated. This time associated with Cyclosporine A and Methotrexate as an insulin infusion.But ocular response was incomplete, persisting visual acuity impairment and neurosensorial macular detachment in both eyes (Figure 1J−1M). In spite of an incomplete clinical response, steroid treatment was withdrawn in three weeks, in decreasing doses, in order to avoid systemic complications. After cessation of steroids treatment, visual acuity improved to 20/40 in right eye and 20/30 in left eye. Macular detachment was resolved in both eyes. An epiretinal membrane development in right eye was detected in OCT (Figure 1N−1R). Immunosuppressive treatment was stopped because of an undercurrent respiratory infection. In the follow up visits, VA was stable and no recurrence of ocular inflammation was detected. Acuphene and patches of vitiligo in her hands had appeared.
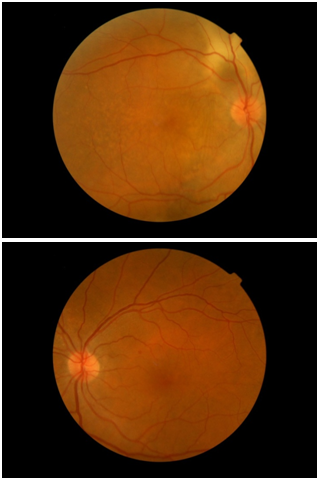
Figure 1I & 1K Retinographies showing choroidal exudation and increased brightness from the ILM in posterior pole.
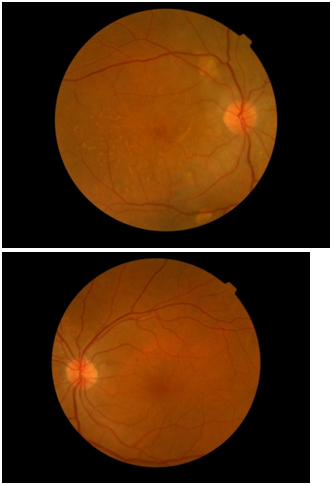
Figure 1N & 1O, OCT reveals macular detachment in both eyes. Notice that in the right eye the detachment is severely tabicated.
Case 2
Caucasian woman aged 22 who attends derived from another center with a diagnosis of unilateral CRCS after abruptly presented severe decrease in visual acuity (VA) in her left eye.Do not have a personal or family history of interest. The picture is not accompanied by systemic signs or symptoms. On examination, VA is 20/20 in her right eye and counting fingers in her left. The IOP is normal in both eyes. The anterior segment examination shows no signs of inflammation. The fundus examination shows a brightening of the internal limiting membrane in the posterior pole of both eyes and a macular neurosensory detachment with a brownish hue in the left eye (Figure 2A&2B). The FA shows hyper fluorescent macular lesion in the right eye with multiple hyper fluorescent spots inside, taking a look of “starry night”, and hyper fluorescence of the optic disc in both eyes (Figure 2C&2D). The OCT of the right eye shows large loculated neurosensory detachment in the macular area. The OCT of the left eye shows neurosensory detachment (Figure 2E& 2F).

Figure 2A & 2B, Retinographies showing choroidal exudation and increased brightness from the ILM in posterior pole of both eyes.
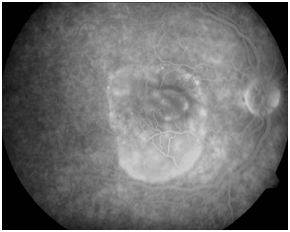
Figure 2C FA of right eye shows disseminated spotted choroidal hyper fluorescence and choroidal hypo fluorescence in macular area.
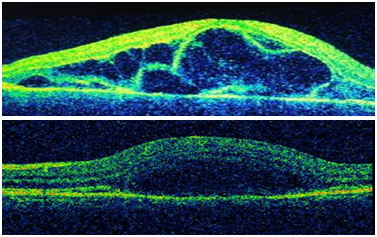
Figure 2E & 2F, OCTs showing macular detachment in both eyes. Notice that in the right eye the detachment is severely tabicated.
The ocular ECO showed mild thickening of the choroid. But no “T sign” was observed.
Biochemistry, microbiology and autoimmunity parameters were normal. HLA-DR4 was positive. The patient was treated with oral steroids prednisone 60 mg every 24 hours and omeprazole, 20 mg c/24h. A week later, the VA's OI has improved to 20/30 and the exploration of the fundus and the OCT showed a decrease macular neurosensory detachment striking her left eye. After a month of treatment, VA was 1 in both eyes and the fundus and OCT scan were normal (Figure 2G&2H).
The differential diagnosis of macular neurosensory detachment must include the following entities
Central serous chorioretinopathy (CSCR): Usually unilateral, most often affects middle-aged men. It can be triggered by steroids exposure. Fluorescein angiography (FA) of fundus in acute CSCR usually shows leaks at the level of the retinal pigment epithelium (RPE) in two main patterns: "Smokestack" or "inkblot." EPR dysfunction is also often demonstrable in indocyanine green angiography (ICG).
Posterior scleritis: Usually unilateral inflammatory condition. The clinical form depends on the location and severity of inflammation. Mostly affects women (14:1) with a mean age of 26. It is associated to systemic diseases in 29% of cases. The most common symptoms are decreased VA due to macular exudation and retro orbital pain that typically increases with external ocular movements (EOM). Ocular ultrasonography shows a marked thickening of the sclera. Retrobulbar edema surrounding the optic nerve is called "T sign".
Harada disease: Inflammatory immune disorder that typically affects middle-aged adults. Bilateral granulomatous panuveitis occurs. In addition to the ocular involvement, may affect other organs that contain melanocytes as skin, ear, and meninges. Vitiligo patches and acuphene can be present. Aseptic meningitis often can be detected after lumbar puncture.
The acute phase of the disease is characterized by neurosensory retinal detachments associated with multiple points of choroidal exudation. It may appear optic disc swelling. Treatment with high doses of systemic corticosteroids often quickly resolves exudative lesions in the acute phase. It requires maintenance therapy with low doses for months to prevent recurrences. To prevent complications associated to long term steroid treatment, immunosuppressive treatment is often recommended. In the chronic phase, recurrences of anterior segment inflammation can appear without new lesions in posterior segment. Others: choroidal neovascularization, punctate inner choroidopathy, B lymphoma, choroidal metastasis, choroidal hemangioma, acute posterior multifocal placoid pigment epitheliopathy, etc.
In our case 1, the ocular findings were typical of Harada disease, as presence of cells in vitreous cavity, serous septet detachmentand the increase of the brightness of internal limiting membrane in the posterior pole of both eyes.3 The prompt good response in the first period of treatment with steroids also supports the Harada diagnosis. The recurrence of inflammation after the withdrawn of steroids treatment could have been avoided reducing very slowly the dose of steroids. In diabetic patients, we recommend a very close follow up of metabolic state by Endocrinology Department from the beginning of the treatment with steroids.
In the second cycle of steroids treatment, the response was unsatisfactory. The angiographic pattern in "smokestack" or "umbrella" pattern made us suspect an episode of CSCR. After suppressing steroids treatment, the serous detachments were solved and the VA improved. We did not continue immune suppressive treatment because of a respiratory infection. But, in follow up visit, no recurrence of macular serous detachment or inflammation was detected. Acuphene and patches of vitiligo in her hands had appeared supporting the Harada diagnosis. We understand this is a case of Harada disease that developed an episode of CSCRtriggered by the steroid treatment. We recommend bearing in mind that steroid treatment usually leads to improvement in inflammatory conditions, including chorioretinal diseases, but at the same could trigger an acute CSCR that may confound us.4
In our case 2, CSCR diagnosis had been made wrongly after finding a serous macular detachment in a young woman. We would like to point out that in the absence of systemic involvement, clinical ocular findings such as serous detachment septations, the brightness increased from the ILM, or angiographic pattern "in Starry Night" as well as positive HLA DR1 and DR4 should guide us to the diagnosis of Harada disease. Also not forget lumbar puncture to demonstrate Linfocitary meningitis may be performed although not without risks. The treatment with steroids in our case was satisfactory; which also supports the Harada diagnosis. In CSCR, steroids should by the contrary be avoided.
We would like to remind the importance of this differential diagnosis since the treatment recommended for Harada is contraindicated in CSCR. And in the other hand, in CSCR the attitude is frequently observation that would lead us to untreate our patients in case our diagnosis is not CSCR but Harada disease.5
None.
None.
The authors have no conflicts of interest to declare.

©2015 Neila. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.