Advances in
eISSN: 2377-4290


Research Article Volume 2 Issue 6
1Department of Pediatric Ophthalmology and Clinical Optics, Jyotirmay Eye Clinic and Ocular Motility Laboratory, India
2Department of Pediatric Ophthalmology, Mahatme Eye Hospital and Eye Bank, India
Correspondence: Mihir Kothari, Jyotirmay Eye Clinic for Children and Adult Squint, Ocular Motility Lab and Pediatric Low Vision Center, 205 Ganatra Estate, Khopat, Thane West 400601, Maharashtra, India, Tel +912225478081
Received: August 12, 2015 | Published: August 24, 2015
Citation: Kothari M. Direct Ophthalmoscopic Indirect Ophthalmoscopy (DIDO) and Estimation Dynamic Distance Direct Ophthalmoscopy (E-DDDO), the two novel uses of direct ophthalmoscope! Adv Ophthalmol Vis Syst. 2015;2(6):202-205. DOI: 10.15406/aovs.2015.02.00068
Aim: To describe two novel uses of a direct ophthalmoscope. 1) Direct ophthalmoscopic indirect ophthalmoscopy (DIDO) for the evaluation of the posterior pole of the eye from a distance using a direct ophthalmoscope and 2) estimation dynamic distance direct ophthalmoscopy (E-DDDO) for the objective measurement of accommodation in children.
Subjects and methods: In this prospective observational study, DIDO and E-DDDO were performed on children< 16 years and compared with the current gold standard, the binocular indirect ophthalmoscopy (BIDO) and dynamic retinoscopy (DR), respectively.
Results: Of 31 consecutive cases, DIDO identified all 5 patients who had retinal pathology diagnosed by BIDO. Seventeen children, aged 9.6±3.1 years underwent the E-DDDO and DR. The accommodative amplitude with E-DDDO was 8±2.3D, (range 4-11D) and that with DR was 8.5±2.7 D, (range 4-14D). One patient with asthenopia & hypo-accommodation was identified on both DR and E-DDDO. The Pearson r for E-DDDO & DR was 0.9. There was no statistical difference between the values obtained on two different techniques (Paired t test–p=0.6).
Conclusion: DIDO and E-DDDO are two valid techniques; DIDO can be used for a rapid screening of the posterior pole of the fundus especially in uncooperative children and E-DDDO can be used to objectively assess the amplitude of accommodation in preverbal children and uncooperative children or adults.
Keywords: Direct ophthalmoscopy, indirect ophthalmoscopy, accommodation in children, photorefraction, dynamic retinoscopy, dynamic distance direct ophthalmoscopy, objective evaluation of accommodation, accommodation in preverbal children, ophthalmoscopy in children
DIDO: direct ophthalmoscopic indirect ophthalmoscopy; BIDO: binocular indirect ophthalmoscopy; E-DDDO: estimation dynamic distance direct ophthalmoscopy; DR: dynamic retinoscopy
The direct ophthalmoscope, built on the principle of coaxial illumination was introduced by Helmholtz1 for the evaluation of the posterior pole of the eye. Later the direct ophthalmoscope was used to evaluate the media opacities, afferent pupillary defect and amblyogenic factors.2–4 In a recent study, the principle of coaxial photorefraction was exploited to use direct ophthalmoscope in the assessment of accommodation in preverbal children.5
When used in combination with 20D condensing lens, the ophthalmoscope can be used to perform indirect ophthalmoscopy! It is very useful in children who are apprehensive of eye examination especially due to close proximity of the examiner. Direct ophthalmoscopic indirect ophthalmoscopy (DIDO) can allow the ophthalmologist to visualise the posterior pole of such a child from distance. In this study I have described the technique of DIDO, the optics of DIDO, the performance as well as the advantages and limitations of DIDO. I have also found out that ‘retinoscopy rack’ and the ophthalmoscope can be used together to ascertain the accommodative amplitude of the eyes which may be very useful in preverbal or uncooperative children! Patients with Down syndrome, cerebral vision impairment, internal ophthalmoplegia, ectopia lentis etc. Suffer from poor accommodation and need bifocals for the appropriate management. In this paper, I present the techniques of DIDO and estimation dynamic distance direct ophthalmoscopy (E-DDDO) and compare them with the existing gold standards, binocular indirect ophthalmoscopy (BIO) and Dynamic retinoscopy (DR).
Thirty one consecutive children aged 1-16 years underwent fundus evaluation of each eye using 20D lens and a direct ophthalmoscope after pupil dilatation followed by the examination of the fundus using a binocular indirect ophthalmoscope. The same examiner who performed the (DIDO) performed the BIO. The examination findings from both the techniques were compared. Seventeen children (6-16 years) underwent evaluation of the accommodative amplitude of each eye using E-DDDO followed by DR). The difference in the accommodation measured and the Pearson’s r (Correlation coefficient) was calculated for the comparison.
Description of the techniques
Direct Ophthalmoscopic Indirect Ophthalmoscopy (DIDO)
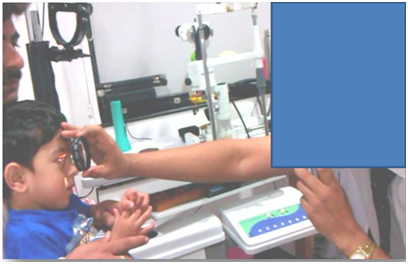
Figure 1 Photograph demonstrating the technique of direct ophthalmoscopic indirect ophthalmoscopy. Note the distance and the position of the patient, 20D condensing lens, direct ophthalmoscope and the examiner.
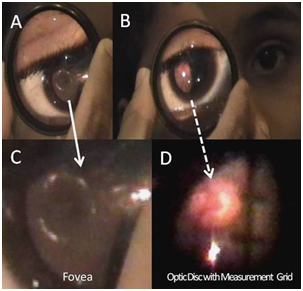
Figure 2 Photographs from the direct ophthalmoscope using the DIDO technique demonstrating the details of the fovea (A and C) and the optic disc (B and D).
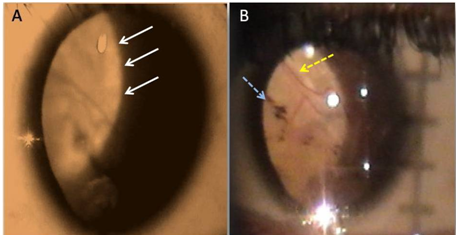
Figure 3 Peripheral retina seen through the direct ophthalmoscope showing (A) the retino-choroidal coloboma (white arrows) and (B) the vasculature and the pigment nests in the inter calary tissue within the colobomatous area.
Estimation Dynamic Distance Direct Ophthalmoscopy (E-DDDO)
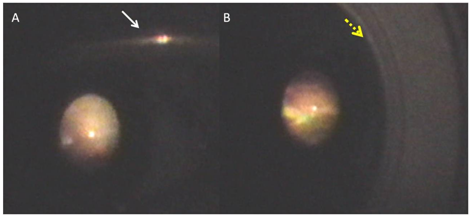
Figure 4 Estimation dynamic distance direct ophthalmoscopy photographs demonstrating (A) a superior bright (emmetropic) crescent in a 7 years old child wearing the spectacle (white arrow) and fixating at a distance of 6 meter and (B) +0.5D lens (yellow arrow) in front of the same child neutralising the emmetropic crescent.
Of 31 consecutive cases, DIDO identified all 5 patients with pathology on BIDO (coloboma, foveal hypoplasia, primary optic atrophy, Coat’s disease (stage 3A) and Stargardt’s disease). Of 17 patients who underwent the E-DDDO and DR, the mean age was 9.6±3.1years. The accommodative amplitude with E-DDDO was 8±2.3D, (range 4-11D) and that with DR was 8.5±2.7 D, (range 4-14D). One patient with asthenopia& hypo accommodation was identified on both DR and E-DDDO. The Pearson r for E-DDDO & DR was 0.9 indicating an excellent correlation between the two techniques. There was no statistical difference between the values obtained on two different techniques (Paired t test–p=0.6). The time taken to perform E-DDDO though not measured in this study seems to be lesser than that with DR. Using an E-DDDO; accommodation could be measured from both the eyes simultaneously unlike that with DR.
The direct ophthalmoscope produces an upright, or unreversed, image of the fundus with approximately 15 times magnification. For a good view, the ophthalmoscope needs to be used at a very close distance which can be very intimidating in some children and occasionally embracing socially. When used with a condensing lens such as a 20D lens, the image characteristic changes to what is seen with BIO. The image visualised in DIDO is inverted, laterally reversed and real. The optics of the DIDO and BIO (Figure 7&8) are similar.
The biggest advantage of DIDO over the direct ophthalmoscopy is that DIDO can be performed from an arm length which is less ‘threatening’ in young children. Another advantage is wider visual field (approximately 5 times larger) as compared to the conventional direct ophthalmoscopy. The optics utilised are similar to that seen in panoptic fundoscope. One more advantage of DIDO is an extremely high portability of the direct ophthalmoscope versus BIO. We do not consider DIDO can replace a BIO as lack of binocularity and inability to visualise the equator or periphery with DIDO would be unacceptable consequences and can result in missing important fundus abnormalities in clinical practice. Also, the light reflexes from the coaxial illumination of a direct ophthalmoscope results in inferior image quality with DIDO as compared to BIO and prevents it to be performed in undilated pupils.
I feel the most important use of the DIDO is for a quick screening of the posterior pole in children who are uncooperative for BIO and direct ophthalmoscopy, to assess the extra foveal fixation and to assess the relative position of the fovea in comparison of the optic disc in evaluation of ocular torsion in cyclovertical squint. The use of direct ophthalmoscope and the optics of dynamic distance direct ophthalmoscopy in the assessment of accommodation were recently described by Kothari et al.5 They did not attempt to quantify the accommodation in that paper. Nevertheless, it is important to quantify the accommodative deficits in children with accommodation failure for the appropriate optical correction as well as monitor the deterioration or improvement in the condition.
In the present study on a small group of normal subjects, I found E-DDDO was as good a technique as DR in the objective evaluation of accommodative amplitude in children. An important limitation of E-DDDO was inability to separately evaluate different meridian which is possible with DR. However, variable accommodative response in different meridia of an eye is rare and suspected to occur in the ciliary body/zonule coloboma. The E-DDDO was advantageous over DR as it was faster and could be done on both eyes to rule out aniso accommodation (different accommodative responses in the eyes of a patient). I found the E-DDDO was easier to learn and perform as compared to DR among the ophthalmic residents and fellows. However, further studies are needed to evaluate E-DDDO in patients with accommodative defects and intra test as well as intertester reliability with adequate sample size.
This manuscript reports two new uses of direct ophthalmoscope. Both the diagnostic techniques are valid and have relevant place in the diagnostic armamentarium of the ophthalmologists. Further studies are needed to evaluate both the techniques in different clinical settings with different diseases of variable magnitude.
None.
I thank Dr William Good, Smith Kettlewell Eye Research Institute for making me aware of the technique of DIDO during my fellowship in Pediatric Neuro-ophthalmology at San Francisco in 2011.
The authors have no conflicts of interest to declare.

©2015 Kothari. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.