Advances in
eISSN: 2377-4290


Research Article Volume 9 Issue 3
1Sivas Cumhuriyet University, School of Medicine, Department of Ophtalmology, Sivas, Turkey
2Sivas Numune State Hospital, Department of Ophtalmology, Sivas, Turkey
Correspondence: Yuksel Demirci, Sivas Cumhuriyet University, School of Medicine, Department of Ophtalmology, Sivas, Turkey
Received: May 21, 2019 | Published: June 28, 2019
Citation: Demirci Y, Toker MI, Bozali E, et al. Comparison of visual functions and contrast sensitivities between monoblock hydrophobic acryrlic monofocal and monoblock hydrophobic acryrlic multifocal intraocular lenses. Adv Ophthalmol Vis Syst. 2019;9(3):85-90. DOI: 10.15406/aovs.2019.09.00352
Purpose: To compare monoblock hydrophobic acryrlic monofocal ultraflex (UF) and monoblock hydrophobic acryrlic multifocal revision (RV) intraocular lens implantations on visual acuities and contrast sensitivities after bilateral cataract extraction.
Setting: Cumhuriyet University, Faculty of Medicine, Department of Ophtalmology.
Design: Prospective, randomized-controlled clinical study.
Methods: Sixty eyes of 45 patients [Group 1 (n=30 UF); Group 2 (n=30 RV)] with cataracts operated by phacoemulsification technique were included. The patients were examined at one day, one week, and one month, postoperatively. At three months, contrast sensitivity tests for distance were performed at 1.5,3,6,12 and 18 cpd as photopic with/without glare and mesopic with/without glare. Patients with corneal astigmatism >1.00 diopter, glaucoma or retinal detachment history, corneal disease, previous corneal or intraocular surgery, abnormal iris, pupil deformation, trauma-related zonular defects, iris and lens capsule defect, macular degeneration or retinopathy, neuro-ophthalmic disease, history of amblyopia, and ocular inflammation, intraoperative capsular defects and vitreous loss, and postoperative visual acuity <0.5 were excluded.
Results: Although it was not statistically significant (p>0.05), compared to Group 1, visual acuity was superior in Group 2. Spectacle independency for Distance visual acuity of the groups were similar (P>0.05). The visual acuity was increased with -3.00 and -3.50 refraction values in defocus curve in Group 2. In all spatial frequencies, contrast sensitivity test values were higher in Group 1 than Group 2.
Conclusion: Our study results show that although both lenses provide comparable visual acuity level, UF lens has a better optic performance on the contrast sensitivity test.
Keywords: contrast sensitivity, mesopic, photopic, multifocal intraocular lens
The quality of life following cataract surgery may be reduced in patients who become partially or completely dependent on eyeglasses. After cataract extraction and the implantation of a monofocal intraocular lens in patients with unilateral cataract, binocular visual functions can be compromised at intermediate and near vision. The main goal of multifocal IOL models is to restore both distance and near visual function. This improvement in the ability of reading is important in today’s information-based society.1,2 Multifocal IOLs are used to compensate for pseudophakic presbyopia and thus improving functional distance, near, and even intermediate vision.3−6 Beside offering good uncorrected near visual acuity in most cases,2,7,8 multifocal IOLs provide also better uncorrected distance visual acuity (UDVA) than most of the monofocal IOLs. The design of multifocal IOLs depend on two optical principles: diffraction, refraction or a combination of diffraction and refraction.9 With the introduction of novel technologies, incoming light rays are distributed to two principal focal points, near vision and distance vision, or to several foci.3,5,10,11 However, several optical side effects including decreased contrast sensitivity, glare disability, or the presence of halos, were reported.8,10,12−18 These effects may significantly affect the patient’s visual performance due to decreased retinal image quality.5 In this study, we aimed to compare monoblock hydrophobic acryrlic monofocal ultraflex (UF) and monoblock hydrophobic acryrlic multifocal revision (RV) intraocular lens implantations on visual acuities and contrast sensitivities after bilateral cataract extraction.
This prospective randomized-controlled clinical trial, a total of 60 eyes of 45 patients (Group 1: n=30 UF; Group 2: n=30 RV) with cataracts were operated by phacoemulsification technique using either monoblock hydrophobic acryrlic monofocal UF lens or monoblock hydrophobic acryrlic multifocal RV lens at Cumhuriyet University, Faculty of Medicine, Department of Ophtalmology between november 2012 and may 2013 were included. In our study, eyes in Group 1 and Group 2 had similar preoperative characteristics. The study adhered to the tenets of the Declaration of Helsinki and was approved by the local ethical committee. Informed consent was obtained from all patients after the nature and possible consequences of the study were explained. Exclusion criteria included more than 1.00 diopter (D) of corneal astigmatism, history of glaucoma or retinal detachment, corneal disease, previous corneal or intraocular surgery, abnormal iris, pupil deformation, trauma-related zonular defects, iris and lens capsule defect, macular degeneration or retinopathy, neuro-ophthalmic disease, history of amblyopia, and ocular inflammation. In addition, intraoperative exclusion criteria were capsular defects and vitreous loss, while postoperative exclusion criteria were visual acuity <0.5. We used a hydrophobic acrylic monoblock, Zaraccom RV (Zaraccom, Sivas, Turkey) with 19 refractive optical zones on the posterior surface, as a diffractive multifocal IOL. This IOL has 360-degree square edge design for decreasing the posterior capsule opacification (PCO) rate. The biconvex diffractive bifocal IOL has an optic diameter of 6.0 mm and an overall diameter of 12.5 mm. It provides +4 D near addition power. The IOL is available in powers ranging from 0.00 to +40.00 D.
We used foldable hydrophobic acrylic IOL, Zaraccom UF (Zaraccom, Sivas, Turkey), with an optic diameter of 6.0 mm and total diameter of 12.5 mm. Zaraccom UF and Zaraccom RV were created by photopolymerization technique. Immersion A – scan biometry was used to measure preoperative IOL power and the SRK-T (Sanders, Retzlaff and Kraff) formula was used to make biometric calculations. The A – constants for Zaraccom RV is 117.5 and Zaraccom UF is 118.4. All operations were performed by a single surgeon (M.I.Toker). Under topical anaesthesia, 2.4 mm clear corneal tunnel incision at the steepest meridian, 5.0–5.5 mm capsulorhexis, hydrodissection, phacoemulsification of nucleus, aspiration of the cortical remnants, and the IOL implantation in capsular bag were done. The mplantation of Zaraccom RV and Zaraccom UF IOLs were performed using a specific injector (Zaraccom-S24 cartridge). The postoperative therapy involved the application of ofloxacin 0.3% and dexamethasone 0.2% eyedrops four times per day for two weeks and ketorolac tromethamine 0.5% (Acular) for two to four weeks. Patients were followed at one week, two weeks, one month, and three months postoperatively. During each visit, refractive status, and distance and near visual acuities were recorded, and slit-lamp examinations, tonometry, and fundoscopy were performed. Distance and near visual acuities were measured with the Snellen chart.
At the third postoperative month, subjective refractions and monocular distance and near best-corrected visual acuities were measured. Binocular distance and near uncorrected visual acuities were determined. Through-focus binocular Snellen charts acuity (defocus curve) was also measured. The patients observed a distance the Snellen chart through pairs of negative lenses increasing from +0.00 to–5.00 D in 0.50 D steps. Contrast sensitivity for distance was measured using the Stereo Optical Functional Acuity Contrast Test (FACT, Stereo Optical Co, Chicago, IL, USA) in all groups. The FACT test allows presentation of sine-wave gratings of different spatial frequencies (1.5, 3, 6, 12, 18 cycles per degree [cpd]) with contrasts varying in steps of 0.15 log10 CS. The CS measurements were taken under photopic illumination condition (85 candelas per square meter). The contrast sensitivity tests at 1,5,3,6,12 and 18 cpd were performed in all patients, as photopic with glare- without glare and mesopic with glare – without glare.
|
Mesopic Without Glare |
UF Contrast Sensitivity Scores ±S |
RV Contrast Sensitivity Scores ±S |
Result |
|
1.5cpd |
25.06±4.91 |
19.70±5.34 |
T=4.04; P=0.001* |
|
3cpd |
31.40±6.32 |
22.53±7.45 |
T=4.96; P=0.001* |
|
6cpd |
26.36±6.89 |
20.53±8.39 |
T=2.94; P=0.005* |
|
12cpd |
12.73±2.63 |
10.50±3.72 |
T=2.58; P=0.010* |
|
18cpd |
5.00±1.14 |
4.80±1.34 |
T=0.61; P=0.539 |
Table 1 Contrast sensitivity scores in spatial frequencies in mesopic conditions without glare with FACT
|
Mesopic with Glare |
UF Contrast Sensitivity Scores ±S |
RV Contrast Sensitivity Scores ±S |
Result |
|
1. 5cpd |
23.10±5.09 |
15.83±4.47 |
T=5.87; p=0. 001* |
|
3cpd |
27.53±6.46 |
17.76±4.68 |
T=6.70; p=0.001* |
|
6cpd |
24.80±8.29 |
16.53±4.32 |
T=4.84; p=0.001* |
|
12cpd |
12. 60±3.20 |
9.16±2.03 |
T=4.95; p=0.001* |
|
18cpd |
5.13±1.13 |
4.46±1.13 |
T=2.27; p=0.027* |
Table 2 Contrast sensitivity scores in spatial frequencies in mesopic conditions with glare with FACT (Functional Acuity Contrast Test)
|
Photopic Without Glare |
UF Contrast Sensitivity Scores ±S |
RV Contrast Sensitivity Scores ±S |
Result |
|
1. 5cpd |
25.76±4.59 |
22.70±4.70 |
T=2.55; p=0.013* |
|
3cpd |
40.10±9.86 |
29.70±9.58 |
T=4.14; p=0.001* |
|
6cpd |
39.13±7.23 |
29.03±9.72 |
T=4.56; p=0.001* |
|
12cpd |
18.96±5.17 |
12.20±4.83 |
T=3.68; p=0.001* |
|
18cpd |
7.06±2.21 |
5.73±2.44 |
T=2.21; p=0.030* |
Table 3 Contrast sensitivity scores in spatial frequencies in photopic conditions without glare with FACT (Functional Acuity Contrast Test)
|
Photopic With Glare |
UF Contrast Sensitivity Scores ±S |
RV Contrast Sensitivity Scores ±S |
Result |
|
1. 5cpd |
25.56±7.38 |
21.70±4.30 |
T=2.47; p=0.016* |
|
3cpd |
37.46±7.41 |
26.60±7.69 |
T=5.57; p=0.001* |
|
6cpd |
38.73±7.23 |
27.26±9.92 |
T=5.11; p=0.001* |
|
12cpd |
17.90±4.93 |
13.40±4.18 |
T=3.81; p=0.001* |
|
18cpd |
6.60±1.49 |
5.66±1.89 |
T=2.11; p=0.039* |
Table 4 Contrast sensitivity scores in spatial frequencies in photopic conditions with glare with FACT (Functional Acuity Contrast Test)
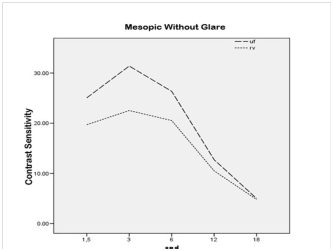
Figure 1 Contrast sensitivity scores in different spatial frequencies in mesopic conditions without glare.
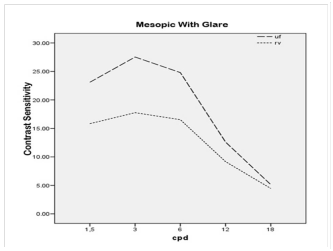
Figure 2 Contrast sensitivity scores in different spatial frequencies in mesopic conditions with glare.
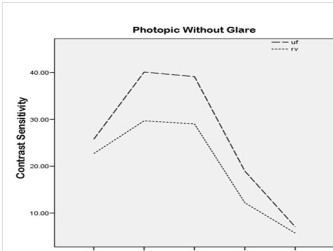
Figure 3 Contrast sensitivity scores in different spatial frequencies in photonic conditions without glare.
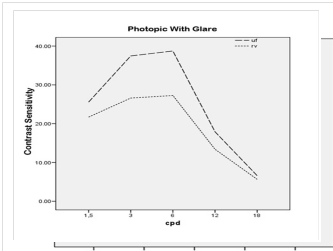
Figure 4 Contrast sensitivity scores in different spatial frequencies in photonic conditions with glare.
|
Eye glasses |
|||
|
Groups |
Gl |
Gz |
|
|
UF |
15 |
15 |
|
|
|
% |
50.0 |
50.0 |
|
|
RV |
9 |
21 |
|
|
% |
30.0 |
70.0 |
|
Total |
24 |
36 |
|
|
% |
40.0 |
60.0 |
|
Table 5 Distribution of spectacle use in distance vision
In the earlier years, multifocal oils were developed to provide functional near and intermediate vision by increasing the depth of field in the eye.3 Currently, there are three types of multifocal oils used in clinical practice: multi-zone refractive, diffractive, and a combination of these two IOLs.3,19 Multifocal diffractive IOLs have concentric rings in the posterior or anterior surface. The rings form two primary focal points independent of the pupil size.3,19 On the other hand, multifocal diffractive IOLs restore both distance and near visual function. However, several optical side effects have been reported with multifocal IOLs; these include induction of halos and glare, and loss of contrast sensitivity.13−15,20,21 In this study we compared the visual acuity outcomes and the ocular and intraocular optical quality in patients with diffractive multifocal IOLs and patients with conventional monofocal IOLs to identify which one provides the highest spectacle independency as well as to establish possible relationship between the optical performance and clinical visual outcomes. In a study, patients with multifocal IOLs reported less spectacle dependency than patients with monofocal IOLs.22 Nonetheless, the visual acuity is not the only critical factor in the assessment of visual function. Although patients have high visual acuity levels, they may still suffer from low contrast sensitivity-related vision problems. In this study, the FACT test was used to identify the contrast sensitivity function (CSF), as this test is one of the reliable methods available for testing the contrast sensitivity.
In our study, eyes in Group 1 and Group 2 had similar preoperative characteristics. This allowed us to compare the postoperative outcomes between similar groups. We found no statistically significant difference in age and sex between the groups. In addition, we observed no statistically significant difference in the postoperative distance-vision outcomes between the multifocal IOL group and the monofocal IOL group. However, the multifocal IOL group had significantly improved near visual acuity. Furthermore, the defocus curve is useful in assessing the visual behavior of a specific IOL model. The curve represents the results with different levels of defocus.23 In our study, there were two peaks of maximum visual acuity at a defocus of approximately 0.00 D and approximately -3.50 D in all eyes in the multifocal IOL group. In a study, the range of focus in near vision was significantly larger in the multi- focal IOL group with peaks of maximum visual acuity approximately at the 0.00 D and +3.00 D levels of defocus.5 In another study, there were two peaks at the expected near focus and far focus (corresponding to 0.00 D and approximately -3.00 D, respectively) in both IOL groups with relatively reduced acuity (0.3 logmar [equivalent to 20/40]) at intermediate distances.24 In addition, there are multiple images focused on retina with the use of multifocal IOLs, therefore, it is inevitable to lose contrast sensitivity. Review of the literature has shown several studies on this subject. In a study, Cillino et al.25 reported that multifocal IOLs produced better postoperative visual acuity, compared to monofocal IOLs. The authors concluded that multifocal IOLs offered sufficient mid and near visual acuity and spectacle independency was higher with multifocal IOLs. Likewise, Goes et al.26 also observed similar findings in their study. Using both static and dynamic contrast sensitivity programs, Vingolo et al.27 found higher contrast sensitivity values in the eyes with monofocal IOLs than diffractive multifocal IOLs In patients with multifocal IOLs, binocular CSF was better than the monocular CSF and the difference in CSF between the conventional monofocal IOL implanted eyes and multifocal IOL implanted eyes seemed to be reduced based on the binocular assessment compared than monocular assessment. The authors reported that 92% of the patients achieved spectacle independency with restor (Alcon Laboratories Inc., Texas, USA) multifocal IOLs.22 In another study with diffractive IOLs, Souza et al.28,29 showed that monocular photopic CS values with Restor IOL were lower than monofocal Acrysoft IOLs, however, there was no significant difference in binocular values between the two types of IOLs. Similarly, Nijkamp and Blaylock28,29 also reported consistent results with the previous study findings.
The IOL technology provides a wide range of focus with no significant decrease in the optical quality. It also offers significantly better uncorrected near visual acuity (UNVA) and distance corrected near visual acuity (DCNVA) than the monofocal IOL. Additionally, Yuvacı et al.30 observed that the contrast sensitivity levels were lower at one month in both mesopic and photopic environment with multifocal IOLs for near vision, in particular. At three months, the relatively low levels remained in mesopic environment at high spatial frequencies for near vision.30 Furthermore, Mesci et al.6 compared monofocal IOLs with multifocal IOLs (refractive and diffractive) and accommodative lenses in terms of visual acuity and contrast sensitivity. The authors demonstrated that multifocal IOLs produced better results in near visual acuity; however, found no significant difference in the distance visual acuity among the groups. In addition, monofocal and accommodative lenses had higher contrast sensitivity than multifocal IOLs. Similarly, our study findings were also consistent with the aforementioned study results.
Multifocal IOLs may offer better near visual acuities, however, lower CS scores, compared to monofocal IOLs. Therefore, we conclude that, the patients who are scheduled for multifocal IOL implantation should be selected carefully. Given the fact that the social needs and today’s information-based society requires better mid-range visual acuity, their occupations and the need of near-mid-distance acuity should be thoroughly interrogated.
What was known
Higher success rate of multifocal IOLs in offering better near visual acuities comparing to monofocal IOLs has been reported in the literature. Multifocal IOLs has also been reported to be associated with lower contrast sensitivity than monofocal IOLs. However, in none of those studies comparing multifocal and monofocal IOLs, Zaraccom IOLs with either multifocal or monofocal property were used for comparisons.
What this paper adds
This is the first study using Zaraccom trademark IOLs to compare IOLs with multifocal and monofocal properties. In our study, we also found that Zaraccom IOLs with multifocal property offer better near visual acuities comparing to monofocal IOLs. Additionally, constrast sensitivity was also lower with Zaraccom multifocal IOLs compared to monofocal IOLs.
Nil.
There are no conflicts of interest.

©2019 Demirci, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.