Advances in
eISSN: 2377-4290


Case Report Volume 8 Issue 4
1Department of Ophthalmology, King Saud University, Saudi Arabia
2Department of Pathology, King Saud University, Saudi Arabia
Correspondence: Hind Manaa Alkatan, International member, COS, Assistant Professor, Chief of Ophthalmic, Pathology Division, Consultant Departments of Ophthalmology and Pathology, Director of KSU Residency, Training Program in Ophthalmology, Assistant Director, External Accreditation unit, Post-Graduate Medical, Education, College of Medicine, King Saud University, PO Box 18097, postal code 11415, Riyadh, Saudi Arabia, Tel 966504492399, Fax 966112052740
Received: July 07, 2018 | Published: July 20, 2018
Citation: Alqahtani F, alkatan HM, Husain S, et al. Neglected left periocular neuroendocrine tumor with a debatable origin: histopathological case report and brief review of the literature. Adv Ophthalmol Vis Syst. 2018;8(4):227-229. DOI: 10.15406/aovs.2018.08.00308
The most common location of small cell neuro endocrine tumor (NET) is pulmonary. Extrapulmonary NET is less observed and has been reported in various anatomic locations including the orbit; however, primary orbital NET is not common, and majority of cases are metastatic. NET of the eyelid is a rare entity that has not been reported extensively in the ophthalmic literature. In this case report we describe a case of an aggressive neglected NET involving the left eyelids and anterior orbit. The case, was diagnosed based on histopathological features and immuno histo chemical staining, however the origin of the tumor remained debatable.
Keywords: small cell carcinoma, neuro endocrine, eyelid, periocular, orbital, metastasis
The most common location of small cell neuro endocrine tumor (NET)is pulmonary, while the overall incidence of extra pulmonary NET is less observed. The extra pulmonary sites include the salivary glands, sinuses, thyroid, larynx, trachea, pleura, thymus, gastrointestinal tract, genitourinary tract, ovary, uterus, cervix, brain, lymph nodes, skin and eyelids.1 Non-ocular NET has been reported in various anatomic locations; however, primary orbital NET is uncommon, and majority of cases are metastatic.2 The orbit has been reported to be involved by NET in only 4-5% of all orbital metastatic cases.3 NET of the eyelid is a rare entity that has not been reported extensively in the ophthalmic literature.4 In this case report we describe a case of an aggressive neglected NET involving the left eyelids and anterior orbit. The case, was diagnosed based on histopathological features and immuno histochemical staining, however the origin of the tumor remained debatable.
An 87year old woman presented with progressive left lower lid swelling of one-year duration. The patient started to notice the mass one year prior to presentation and the lesion has been progressively increasing in size with an aggressive obvious rapid growth over the last 2months. The patient denied any history of associated pain or discharge in relation to the lesion. Her right eye was lost since childhood after history of trauma. She is a known case of uncontrolled hypertension and end-stage renal failure (ESRD) on hemodialysis. Upon examination, she had no light perception using her right eye, which also showed total corneal scarring with no further details of the anterior or posterior segments. The external examination revealed a huge left orbital and eyelids mass with totally obscured left globe. The mass was non-tender with marked telangiectasia, feeder blood vessels, areas of hemorrhage and crusting (Figure 1A) (Figure 1B). There were no palpable pre-auricular or neck lymph nodes.
Computerized tomography (CT) scan of the brain and orbits demonstrated a large oval-shaped heterogeneous mass noted in the antero-inferior aspect of the left orbit. The mass showed increased vascularity and approximately measured: 4.2 x 3.9min the axial plane, 5.0 x 4.0cm in the coronal plane, and 4.9 x 3.9cm in the sagittal plane. The mass appeared radiologically to be originating from the left lower eyelid and to be intimately abutting the left globe, which was displaced postero-laterally. There was no evidence of intra-ocular extension of the mass into the left globe. The extra-ocular muscles as well as the left optic nerve appeared both preserved on the left side. The left bony orbital margins did not show any evidence of erosion or destruction (Figure 1C) (Figure 1D). Further imaging with contrast media was not possible because of the patient’s general health condition and ESRD.
Incisional biopsy under local anesthesia was performed and the histopathological examination demonstrated proliferating sheets of small blue cell tumor (Figure 1E) (Figure 1F) with numerous mitotic activity consistent with a high grade malignant small cell neuro endocrine tumor (NET).This was further confirmed by immuno histochemical staining. The tumor cells showed diffuse cytoplasmic staining with CK 8/18 (Figure 2A), CK Cocktail, CK7, and Epithelial membrane antigen (EMA) (Figure 2B).The cells also expressed Synaptophysin, Neuron specific enolase (NSE) (Figure 2C) (Figure 2D) in addition to CD56.Very weak focal positivity was seen with thyroid transcription factor 1 (TTF-1) antibodies, thus ruling out pulmonary adenocarcinoma (Figure 2E). The tumor cells failed to express the following: CK20, CK5/6, p63, CD45, CD99, S-100, HMB-45, Vimentin, Neuro filament, and Chromogranin. The Ki67 proliferation index was 100% (Figure 2F). The case was discussed in the tumor board and the plan was to go for palliative radiation. No further follow up was documented. An informed General Consent has been taken, which includes using patient’s anonymous information for this report.
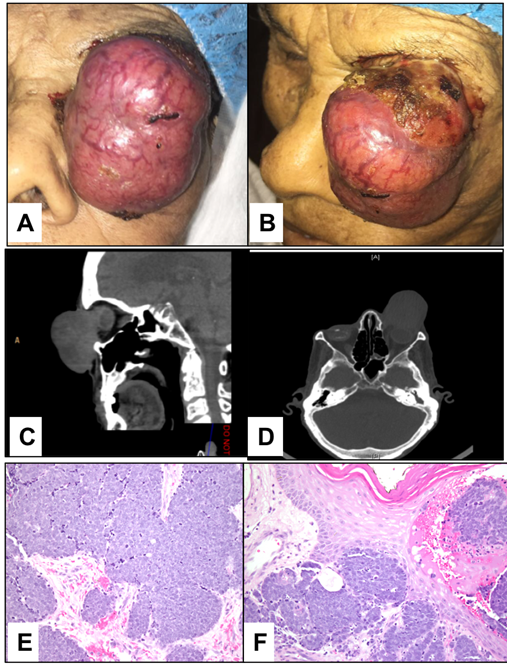
Figure 1 The clinical appearance of the huge periocular mass on the left side with extensive eyelid involvement (A and B). Computed tomography scan (CT) of the brain and orbits demonstrating a large oval-shaped heterogeneous mass lesion noted in the antero-inferior aspect of the left orbit. It appeared to be arising from the left lower eyelid. The mass measured approximately 4.9 x 3.9cm in the sagittal plane (C) and 4.2 x 3.9cm in the axial plane (D). (E) The histopathological appearance of the tissue obtained by incisional biopsy showing high grade proliferating small blue cells. (Original magnification X200 Hematoxylin and eosin). (F) The close proximity of the tumor proliferation to the overlying eyelid skin. (Original magnification X400 Hematoxylin and eosin).
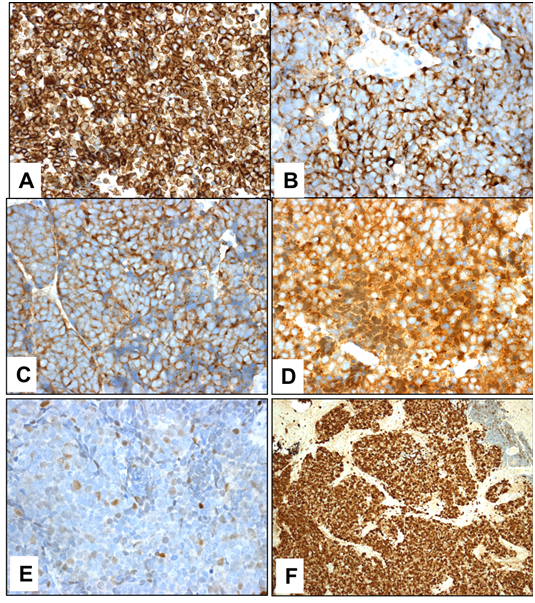
Figure 2 The tumor cells of the small cell carcinoma expressing CK 8/18 in (A) and EMA (B) (Original magnification X400). (C and D), Positive staining of tumor cells with antibodies of neural tissue markers synaptophysin and neurone specific enolase (NSE) respectively (Original magnification X400). (E), Weak focal expression of thyroid transcription factor 1 (TTF-1) ruling out metastatic lung adenocarcinoma (Original magnification X400). (F), The highly malignant tumor showing high proliferation index (Original magnification X100 Ki67).
The specific etiology and histo pathogenesis of small cell neuroendocrine carcinoma is uncertain. Typically, small cell neuro endocrine carcinoma exhibits an aggressive biologic behavior with specific immuno histochemical features, and often spreads hematogenously to distant sites with guarded prognosis.4 Histopatho logically, it may be difficult to distinguish this tumor from other small round cell tumors such as metastatic pulmonary small cell carcinoma, high grade melanoma, malignant lymphoma, and notably Merkel cell carcinoma.5 Therefore, the mainstay modality to reach the diagnosis of small cell neuro endocrine carcinoma is by immuno histochemistry which has unique features such as the frequent reactivity to Chromogranin A and Synaptophysin in addition to NSE, which is highly sensitive, but not specific as a marker for NET.6 The diagnosis in our case was confirmed by the immuno histochemical staining profile. Owing to the fact that this might have been a NET originating in the eyelid, Merkel cell carcinoma had to be ruled out.In all of the case series reviewed, Merkel cell carcinomas were positive to CK20 antibodies.7 Metz in his series of Merkel cell carcinoma demonstrated expression of CK 20, while 4 out of 6 cases were positive to neuro filament immunostaining. However, some studies have shown little percentage of Merkel cell carcinomas that were negative to CK20. The combined positivity with antibodies to CK 7 and negativity with antibodies to CK 20 and neuro filament was sufficient for us to rule out Merkel cell tumor. Llombart also demonstrated similar expression of CK20 and CD99 in more than 90% of the Merkel cell carcinoma cases studied.8 Absence of expression of some other IHC markers by the tumor cells such as thyroid transcription factor 1 (TTF-1) and CD 99 has an additional value in the differential diagnosis of a primary small cell neuro endocrine carcinoma. Hanly reported that 85% of small cell carcinomas arising in the lung express positive reactivity for TTF-1.9 A metastatic small cell carcinoma of the lung was ruled out by the very weak focal expression of TTF-1 by the tumor cells in our case. From the histopathological point of view, a secondary NET was favored with recommended further investigation, but the patient’s general condition hindered systemic work up to exclude a primary NET elsewhere. NET originating from a gastrointestinal primary location, usually metastasizes to the orbit, while primary bronchopulmonary NET often results in ocular uveal metastatic involvement. However, there have been unusual reported cases that do not follow this pattern.9 The tumor in our case was initially thought to be a metastatic NET owing to the extreme rarity of primary NET in the eyelid, however the history, clinical examination and the radiological findings were supportive of a primary eyelid lesion. Unfortunately, most of small cell neuro endocrine carcinoma have guarded prognosis.10 Our patient underwent palliative therapy irrespective of the final conclusion of her tumor to be considered primary or metastatic.
In conclusion, neuro endocrine cells exist throughout the body, thus, neuro endocrine carcinoma should be kept in mind as a differential diagnosis of primary eyelid tumors. In our case, we favor a primary small cell NET arising in the eyelid even though it is very rare, however metastatic lesion remains a possibility. We strongly believe that systemic workup must be done to rule out evidence of primary pulmonary, bronchial or gastro-intestinal NET.
None.
Authors declare that there is no conflict of interest.

©2018 Alqahtani, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.