Advances in
eISSN: 2377-4290


Case Report Volume 8 Issue 4
Department of Ocular Pathology, Sri Sankaradeva Nethralaya, India
Correspondence: Dipankar Das, Department of Ocular Pathology, Uveitis & Neuro-Ophthalmology Services, Sri Sankaradeva Nethralaya, Guwahati- 781028, India
Received: June 29, 2018 | Published: July 18, 2018
Citation: Dhir P, Das D, Agarwal B, et al. The masquerading squamous cell carcinoma. Adv Ophthalmol Vis Syst. 2018;8(4):217-219. DOI: 10.15406/aovs.2018.08.00305
We report a unique case of squamous cell carcinoma with intraocular spread to anterior chamber & ciliary body, which was diagnosed as grade II pterygium initially. Clinical markers with characteristic findings on UBM, high resolution AS-OCT & MRI, and histological identification of keratin pearl in enucleated sample helped in establishing the diagnosis of intraocular squamous cell carcinoma.
Keywords: pterygium, squamous cell carcinoma, masquerade, impression cytology
This 36year-old male patient presented to us with pain & redness in right eye (OD) since last 2months and decreased vision since childhood attributed to injury with stone. Best corrected visual acuity (BCVA) in OD was counting fingers @3mt & in left eye (OS) 20/60. Slit lamp examination revealed conjunctival congestion in OD along with tissue growth over corneal surface, pigments on corneal endothelium, quiet anterior chamber (AC), with clear lens. The growth had limbal fixity and was extending from 7 to 10 clock hours over lateral aspect of cornea without any prominent vasculature. Fundus examination showed para-foveal scarring. OS was unremarkable. Intra ocular pressure was 20 & 18mmHg respectively. Diagnosis of OD pterygium was made and patient underwent pterygium excision with conjunctival autograft. Histopathology was inconclusive. Postoperatively patient was on antibiotics, steroids and lubricants for period of 6weeks and doing well. Patient re-presented to us, 3months post surgery when he noticed an abnormal growth on temporal side of cornea.
On examination white coloured mass in temporal irido-corneal angle (Figure 1B) which was pre-occluding the iris along with surface changes, was noted (Figure 1A). The unhealthy looking tissue was lisamine green positive.
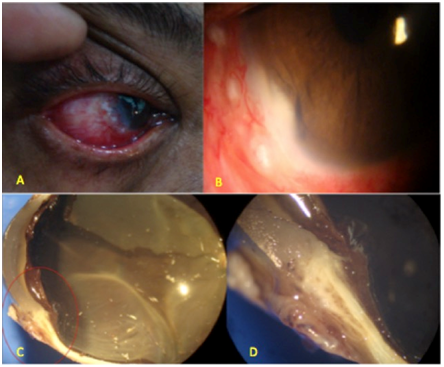
Figure 1 Torch light (A) & Slit lamp examination B showed a white coloured mass in temporal irido-corneal angle which was pre-occluding the iris along with surface changes. Gross visualization (C & D) after En-block enucleation.
Ultrasound Biomicroscopy (UBM) showed Figure 2 mass in infero-temporal quadrant with ciliary body infiltration from external lesion with no involvement of iris tissue. Angles were open with external ocular coats being thickened. AS-OCT Figure 3 showed irregular iris surface along with involvement of ciliary body.
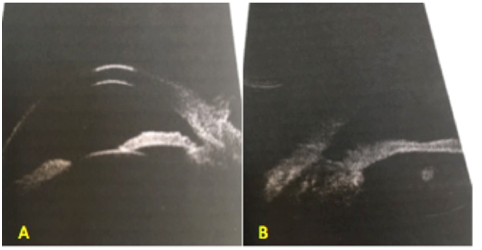
Figure 2 UBM showed a mass in infero-temporal quadrant with ciliary body infiltration from external lesion with no involvement of iris tissue.
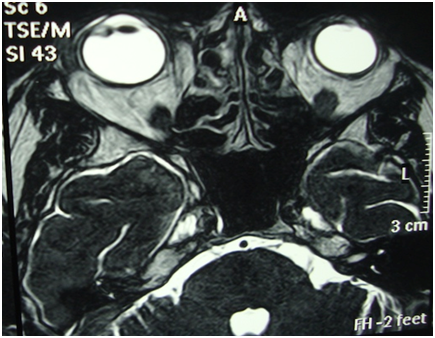
Figure 3 MRI showed an enhancing lesion measuring 5x4mm inside ciliary body on lateral aspect with associated preseptal soft tissue swelling.
MRI Figure 3 showed an enhancing lesion measuring 5x4mm inside ciliary body on lateral aspect with associated preseptal soft tissue swelling. Systemic evaluation for HIV, HPV and Hepatitis came out to be clean.
On basis of clinical appearance, UBM and MRI findings diagnoses of Squamous Cell Carcinoma with intraocular and lacrimal tissue spread were made. En-block enucleation with Mitomycin C application (Figure 4C) (Figure 4D) along with lacrimal tissue resection and cryotherapy to vortex veins was done and ball implant was placed. Margins of conjunctiva were resected till it was free of altered cells on frozen section. Histology of enucleated eye Figure 4D showed keratin pearls (Figure 4A) along with atypical undifferentiated cells (Figure 4B) (Figure 4C) and confirmed it to be Squamous Cell Carcinoma of Grade-II involving Conjunctiva, Limbus, Anterior Chamber, Ciliary Body and Retina (With localized exudative RD) with no involvement of Lacrimal Gland.
Ocular surface squamous neoplasia (OSSN) is an uncommon disease. Squamous cell carcinoma is the third most common ocular tumor after lymphoma and melanoma, and it is the most common primary malignancy of the conjunctiva.1,2 Lee & Hirst described all primary dysplastic carcinomatous lesions arising from epithelium of conjunctiva, cornea and coined the term OSSN.2 Association of OSSN with high levels of ultraviolet B exposure along with high preponderance in patients suffering from AIDS or Human Papilloma Virus (HPV).3 These tumors arise most commonly in the limbal region and may not be distinguished from pterygium on clinical grounds alone.
Clinically OSSN may present as conjunctivitis, interstitial keratitis, corneal thinning or melt, inflamed pterygium or an abnormal growth at limbal area. Histologically, OSSN includes
Epithelial Dysplasia
Hot markers for pterygium progressing to surface neoplasia
Ultrasound Biomicroscopy (UBM) is useful to clinical examination in determining the presence of deep invasion. The tumor surface is usually hyperechoic while the tumor stroma is generally hypoechoic Specific UBM findings suggestive of ocular tumor extension
Confocal microscopy is a noninvasive imaging technique Cellular anisocytosis, pleocytosis, and an-isonucleosis,7 high reflective cytoplasm with enlarged nuclei -high nuclear to cytoplasmic ratio, and indistinct cytoplasmic borders are seen in cases of squamous cell carcinoma.8 Ultra High Resolution (UHR-OCT) findings included epithelial thickening and hyper-reflectivity, whereas pterygia and pingecula showed a subepithelial mass under thinner epithelium.7
Impression Cytology (IC) rare nowadays but it can be useful in diagnosis & has been shown to correlate closely with histopathology. In IC, superficial epithelial cells are collected by applying bio pore membrane & then mounted on slide for analysis It is not possible to differentiate intraepithelial lesions from invasive squamous cell carcinoma given the superficial sampling of cells, thus limiting the utility of IC in diagnosing invasive disease
Lissamine green and rose bengal considered as diagnostic dyes are routinely used to stain and delineate the extent of OSSN lesions but since these dyes are nonspecific and stain many other ocular surface conditions, it is not possible to diagnose OSSN with the use of these dyes alone.9 Biopsy with Histopathology (Figure 4D) (Figure 4A) is the gold standard for diagnosing a case of OSSN Depending on the level and thickness of epithelial involvement varying grades of dysplasia are classified As the lesion progresses from mild to severe dysplasia, the cells differentiate less gradually losing their squamous features until eventually the full thickness of epithelium is made of undifferentiated atypical cells which can even have basaloid like appearance
Pterygium should not be assessed as a simple case depending on its clinical appearance; it can masquerade as CIN or invasive SCC, leading to severe ocular morbidity Several diagnostic modalities including Impression Cytology, vital dye staining, UBM, Confocal Microscopy and UHR-OCT can assist in the early diagnosis and monitoring of OSSN lesions but histopathology remains the gold standard An early correct diagnosis of OSSN could change the entire modality of treatment from destructive procedure of enucleation to start of topical anti-cancer medication
Authors declare that there is no conflict of interest

©2018 Dhir, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.