Advances in
eISSN: 2377-4290


Case Report Volume 1 Issue 2
1Department of Ophthalmology, Augenklink Mainfranken Schweinfurt, Germany
2Department of Ophthalmology, Philipps University Marburg, Germany
Correspondence: David Kubiak, Department of Ophthalmology, Augenklink Mainfranken Schweinfurt, Germany Am Oberen Marienbach, 197421 Schweinfurt Germany, Tel 49 6021 7934272
Received: August 05, 2014 | Published: August 29, 2014
Citation: Kubiak D, Kicova N, Bertelmann T, et al. Central serous chorioretinopathy after caesarean section. Adv Ophthalmol Vis Syst. 2014;1(2):27-29. DOI: 10.15406/aovs.2014.01.00008
Background: We report a case of central serous chorioretinopathy (CSCR) after caesarean section of a 37-year-old Caucasian woman. Four days after an uneventful delivery of twins, the patient noticed blurry vision, metamorphopsia and central scotoma of her right eye.
Methods: At presentation, the visual acuity of the right eye was 8/20 and funduscopy revealed a central serous detachment of the retina. Optical coherence tomography displayed an increase of macular thickness to 558μm and fluorescein angiography showed “pinpoint” leakage at the foveolar avascular zone. Non-steroidal, anti-inflammatory eye drops and acetazolamide tablets were administered.
Results: Five months later, macular morphology returned to normal, with a macular thickness of 276μm and a visual acuity of 20/20. Although CSCR has been reported during pregnancy, this is, to the best of our knowledge, the first report of a CSCR following an uneventful caesarean section.
Conclusion: CSCR should be taken into account in the differential diagnosis of impaired vision following caesarean section. Women giving birth via caesarean should be informed of the possibility of a postpartum CSCR.
Keywords: caesarean section, central serous chorioretinopathy, optical coherence tomography
CSCR, central serous chorioretinopathy; RPE, retinal pigment epithelium; FA, fluorescein angiography; OCT, optical coherence tomography
Central serous chorioretinopathy (CSCR) is a serous detachment of the neurosensory retina, respectively retinal pigment epithelium (RPE) caused by a focal breakdown of the outer blood-retina barrier resulting in an accumulation of fluid between the photoreceptor outer segments and the RPE.1 This disease usually affects middle-aged men and has been associated with A-personality, psychological stress, hypertension, elevated cortisol, epinephrine blood levels and arterial hypertension.2 Patients complain about a decrease of vision, metamorphopsia, central scotoma and micropsia. Episodes of CSCR are often self-limited with a resolution of the subretinal fluid occuring within one to four months.3 CSCR has been reported before in pregnancy and following rhinoplasty,4 but there has been no association to caesarean section up to date.5
A 37-year-old woman (gravida 2, para 1, abortus 0), following an uncomplicated pregnancy except for a history of insulin-dependent gestational diabetes with good glycaemic control and a local Varicella-Zoster infection which treated successfully, underwent elective caesarean section under spinal anaesthesia with bupivacaine hydrochloride (10mg). Surgery was uneventful and two healthy twin-girls were delivered. Corticosteroids were at no point given. Antibiotics were given intraoperatively. Four days after the caesarean section the patient experienced a sudden decrease of visual acuity combined with a central scotoma and metamorphopsia in her right eye. At presentation, best-corrected visual acuity of the right eye was 8/20 with metamorphopsia, a central scotoma in Amsler's grid and blurred vision. Funduscopy of the right eye revealed a serous elevation of the macula (Figure 1 (A−C)). Fluorescein angiography (FA) disclosed three expanding points of fluorescein leakage at the foveolar avascular zone. Optical coherence tomography (OCT) sections through the macula showed a neurosensory retinal detachment with an increase in retinal thickness equal to 558μm.

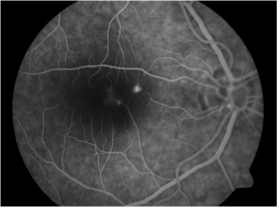
Medical treatment consisting of non-steroidal, anti-inflammatory eye drops and acetazolamid tablets was started. Five months later- the patient missed her 2 months examination- the patient gained full visual acuity (20/20). The OCT showed a complete resolution of the neurosensory retinal detachment with a foveal thickness of 276μm (Figure 2). A second FA was not performed with respect to the patient, who was at that time still breastfeeding.
CSCR is a chorioretinal disorder characterized by serous detachment of the retina at the posterior pole due to a dysfunctional endothelium, leading to acute vision loss, accompanied by micropsia, metamorphopsia and a central scotoma. The exact pathogenesis of CSCR is still unknown, but there is an association with male gender, A-personality, steroid therapy and stress as risk factors.6 Funduscopy and OCT of the macula typically show a serous detachment of the neuroretina and/or RPE. The FA displays a “pinpoint” or an “umbrella”-sign. This describes a small hyper-fluorescence in the early phase of angiography, which progresses into a broader leakage. In 90% of the patients, visual acuity returns to normal and the serous detachment disappears within one to four months and visual acuity returns to normal regardless of any treatment.7 Treatment for CSCR includes focal photocoagulation or systemic medication of carbonic anhydrase inhibitor acetazolamide.
As the spinal anaesthesia with bupivacaine hydrochloride has no systemic effect on endogenous cortisol level, the perioperative stress exposition throughout the abdominal surgery of the caesarean section might have triggered an endogenous cortisol increase and therefore promoting the development of CSCR. It has been postulated that cortisol changes choriocapillaris' permeability and therefore plays an important role in the development of CSCR.8,9 High cortisol levels are found in most risk factors for CSCR, such as type A-personality, male gender, pregnancy and perioperative stress response.10 Usually 72 hours after surgery the perioperative stress response ends and all increased levels returned to normal limits.
In our case, this coincides with the beginning of CSCR, which was 4 days after surgery. Stress situation such as abdominal surgery in terms of cesearean section seem to play a pivotal role in the development of CSCR. However the exact pathogenic mechanisms of CSCR still remain unknown. Cases of CSCR during third trimester of pregnancy due to high cortisol level have been reported before.5 To the best of our knowledge a CSCR after caesarean section and a normal pregnancy has not been previously described. CSCR should be taken into account in the differential diagnosis of impaired vision following caesarean section. Women giving birth via caesarean should be informed of the possibility of a postpartum CSCR.
None.
Authors declare that there is no conflict of interest.

©2014 Kubiak, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.