eISSN: 2378-3176


Review Article Volume 6 Issue 5
1Medical student at St. George?s University, Grenada
2Professor of Clinical Urology, Tulane Medical School, Louisiana, USA
Correspondence: Neil H Baum, Tulane Medical School, 3525 Prytania Street, Suite 614, New Orleans, LA 70115, Tel (504) 891-8454
Received: May 05, 2018 | Published: November 26, 2018
Citation: Miller S, Mobley D, Rathore C, et al. Watchful waiting vs. active surveillance: Which treatment option is right for patients with localized prostate cancer? Urol Nephrol Open Access J. 2018;6(6):173-176. DOI: 10.15406/unoaj.2018.06.00228
Currently, active surveillance is an acceptable option for the management of low risk prostate cancer. Watchful waiting, which is different from active surveillance, is an option for certain high risk men or older men with multiple co-morbidities. Since these two options are often confused or not understood by patients, this article is intended to differentiate the two options and provide guidelines for which men are candidates for either active surveillance or watchful waiting. As a result, physicians caring for men with localized prostate cancer will have the proper information and data to help men make a decision regarding treatment.
Keywords: prostate cancer, watchful waiting, active surveillance, definitive treatment for prostate cancer
Prostate cancer is a slow-growing malignancy. Approximately 17 out of 100 men in the United States will develop prostate cancer; however, only 3 of these 17 will die of prostate cancer.1 Moreover, 97% will die of something other than prostate cancer.1
Because of the indolent nature of some prostate cancers (especially in patients who are older or have other serious health problems and limited life expectancy), these men may never need treatment for their disease. Thus, an option that may be preferred and more clinically appropriate for these men is offered. The two options are referred to as watchful waiting and active surveillance.
Watchful waiting and active surveillance are often mistakenly interchanged. Both options are generally offered to men with low-risk, low-grade prostate cancer (Gleason score ≤6 and low PSA ≤10).2 However, the two management options for prostate cancer are separate strategies with different enrollment criteria and separate purposes.
Watchful waiting is a viable option for older men and\or for men who have significant comorbidities. Its purpose is to avoid risks and complications associated with definitive prostate cancer treatment, such as erectile dysfunction and urinary incontinence.
In contrast, active surveillance is a more appropriate option for younger men (<65 years of age) with a considerable life expectancy (>10 years) and low risk disease. Active surveillance has curative intent; it is considered “deferred treatment,” or an opportunity to move to definitive treatment in the event of tumor reclassification and/or disease progression. In these cases, patients can have an interim freedom from the potential side effects of definitive therapy. Some variability exists in the monitoring and protocols for active surveillance. Many urologists would recommend PSA testing and symptom assessment every 3-4 months for 2 years and then every 6 months thereafter.3 A digital rectal exam is usually performed periodically. A repeat prostate biopsy is recommended one year following the diagnosis of prostate cancer. The interval of subsequent prostate biopsies is typically increased to every 2 years. A rise in PSA level, a suspicious change in the digital rectal exam, or concerning symptoms would prompt an earlier biopsy. Consideration of MRI and/or genomic testing (discussed later) may further stratify the risk of disease progression. Of course, this intense follow up would not be necessary for patients enrolled in a watchful waiting protocol.
Watchful waiting is sometimes falsely perceived as “doing nothing.” Rather, watchful waiting is a recognized, purposeful strategy designed for older and/or health-compromised men with localized prostate cancer. It is a conservative management style based on the idea that localized, or micro-focal, prostate cancer is pervasive and part of the aging process.3 The prevalence of localized prostate cancer has increased since 19914 with the advent of PSA screening.5 The new PSA era has led to over-diagnosis with the ubiquitous identification of indolent, slow-growing prostate cancers. In response to over-diagnosis, watchful waiting was suggested as a method to avoid overtreatment with its attendant complications.
Patients on watchful waiting tend to be 65 or older, with a lower stage prostate cancer (T1c stage), lower PSA (<10ng/ml), and lower Gleason score (Gleason score of 6) at time of diagnosis.6 They also tend to be patients at a high competing risk of mortality from other comorbidities. One widely accepted protocol for watchful waiting originates from studies like the Prostate Cancer Intervention Versus Observation Trial (PIVOT). These patients are usually followed with PSA level, digital rectal exam, and symptom assessment every 6 months for the first 2 years, then yearly. If this approach leads to further concerns, additional testing can include imaging such as bone scan, CT, or MRI. Again, watchful waiting is directed more towards minimizing the complications of the disease rather than providing a cure.
If there is disease progression or the patient becomes symptomatic, he is offered palliation in the form of androgen deprivation therapy. Androgen depravation therapy reduces testosterone to castrate levels and results in a decrease in growth of the primary tumor as well as the metastatic lesions.
Physician guidance
Physician guidance is an all-important component behind a well-informed patient who is aware of all of his options. Appropriate candidates will opt for watchful waiting or active surveillance when offered these options.7 Watchful waiting candidates who proceed to active treatment are often those who are not presented with watchful waiting as an option at diagnosis.7 Similarly, although the data is lacking, active surveillance is likely underutilized. Those who do choose watchful waiting or active surveillance should certainly be presented with all options, including their benefits and consequences. These men cite the helpfulness and reassurance of being fully informed as significant contributions to their decision-making.7
The physician’s point of view is influential in the decision-making process. Physicians serve as a trustworthy, knowledgeable source for professional opinion on personal healthcare decisions. Even in the technological age of instant Internet information available on the Internet, a physician’s medical opinion is of utmost help to patients. A common reason for choosing expectant management is the physician’s assurance that watchful waiting is a reasonable alternative to definitive treatment in the appropriate patient.8
Quality of life
Quality of life is a serious consideration for men deciding among watchful waiting, active surveillance, and curative treatment. Men consider side effects such as erectile dysfunction, urinary incontinence, and lower urinary tract symptoms as part of their decision-making among these options.9 Their pre-diagnosis level of function in these three areas may also influence their decision. The higher likelihood of side effects from definitive treatment in older patients is another argument for watchful waiting in this age group.
Non-clinical factors
In addition to physician guidance and quality of life, patients’ decisions are also influenced by non-clinical factors such as marital status, psychological stress, and the pressure to “do something.” Studies show that men who are widowed or never married are more likely to choose watchful waiting.10 Many men experience anxiety with the idea of conservative management because they are bothered by the continued presence of prostate cancer and the possibility of disease progression. To intentionally accept watchful waiting when curative treatments are available is difficult for some men and their families.
In most situations, the decision to select a watchful waiting approach to prostate cancer is a decision that is made between the patient and his physician. This is a discussion that lays out the risks and complications associated with definitive treatment. The patient and the physician review the patients’ tolerance for risk and side effects. Patients who are sexually active or who have a fear of incontinence may find watchful waiting the preferable approach.
There are formulas that can assist physicians caring for patients with prostate cancer to help with the decision-making. The Charlson Index looks at comorbidities and can provide a predictive value for 10-year survival.11 Comorbidities that are part of the decision-making equation may include recent myocardial infarction, congestive heart failure, poorly controlled diabetes, chronic obstructive pulmonary disease, chronic renal failure or liver disease. Any of these comorbid conditions will impact the decision-making on behalf of the patient and lean in the direction of watchful waiting.
There is a wide variety of approaches to expectant management. This group of prostate cancer patients is best managed with a team approach by the urologist and primary care physician. A patient’s personal physician can provide both convenience for some of the testing and another level of reassurance. Watchful waiting should be directed towards avoidance of unnecessary testing and treatment. On the other hand, active surveillance should be focused on detecting early signs of progression, while avoiding potential side effects of definitive therapy. Figure 1 demonstrates a suggested protocol outlining the management of these low-risk prostate cancer patients.
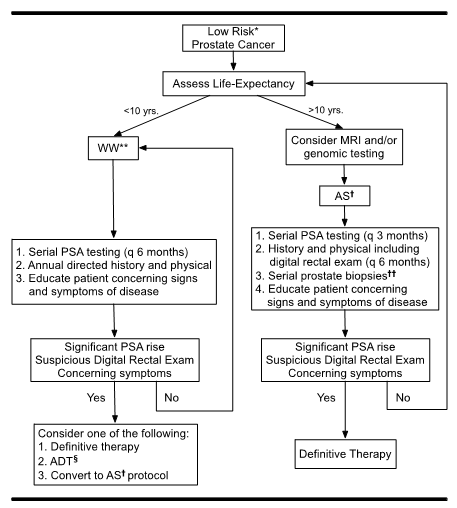
Figure 1 Suggested approach to the newly-diagnosed, low-risk prostate cancer patient.
*Risk assessed with D'Amico system, NCCN guidelines (National Comprehensive Cancer Network), or CAPSURE (Cancer of the Prostate Strategic Urologic Research Endeavor).
**Watchful waiting.
†Active surveillance.
††lnitial repeat biopsy at one year with subsequent increase in interval per doctor discretion.
§Androgen deprivation therapy.
More on PSA Monitoring
The advent of PSA screening, demonstrated in a comparison of the SPCG-4 and PIVOT trials, is what, importantly, lends to the current guidelines of watchful waiting clinical management. The SPCG-4 (Scandinavian Prostate Cancer Group Study Number 4) trial provided one of the earlier watchful waiting protocols. The SPCG-4 trial, conducted between 1989 and 1999, assigned men with early prostate cancer to watchful waiting or radical prostatectomy based mainly on palpable nodule in physical exam and/or self-reported urologic symptoms.12 Results of the trial showed that 200 of 347 men in the surgery group and 247 of the 348 men in the watchful waiting group died. Of the 200 surgery group deaths, 63 of them were prostate cancer-specific deaths; of the 247 watchful waiting, 99 were prostate cancer-specific.12 However, within a decade of the SPCG-4 trial, one very important diagnostic tool – the PSA blood test - surfaced to begin a new method of early prostate cancer detection. The PIVOT trial began in the PSA era, which allowed important questions to be answered concerning long-term benefit of surgery and if surgical intervention does in fact reduce prostate-cancer specific mortality.13 PSA testing profoundly changed screening for prostate cancer. Results of the PIVOT trial indicated that long-term benefit of surgery applies more to younger men (<65 years of age) and does not significantly reduce prostate-cancer mortality or overall mortality.13 The PIVOT trial laid the groundwork of today’s more appropriate criteria in managing men on watchful waiting.
Multiparametric MRI
Developing prostate MRI technology can be coupled with PSA or other prognostic tools to increase screening specificity. The multiparametric MRI (MP-MRI), unlike the PSA blood test, provides an anatomical assessment.14 This additional assessment pinpoints lesion volume and location and, consequently, determines overall tumor burden and likelihood of local spread through assigning the lesions a 1-5 score.14 The European Society of Urogenital Radiology (ESUR) proposed a numeric system called the Prostate Imaging Reporting and Data System, or PI-RADS using a 1-5 scale, for prostate cancer detection.15 It is based on an earlier system for breast imaging.
This MRI technology tends only to reveal intermediate and high-grade cancers and, thus, has the potential to reduce overtreatment of indolent disease. The MP-MRI has high prognostic value in identifying those men who can safely pursue active surveillance or move to a more definitive therapy. However, MP-MRI probably has limited value for a watchful waiting candidate, since the treatment decision in this group is driven more by advanced age and/or comorbidities rather than further risk stratification.
Genomic testing
As with MP-MRI, genomic testing may provide further risk stratification. A growing list of commercially available products can examine the gene expression of prostate cancer cells present in an individual patient’s biopsy specimen. This information is then compared to a historical cohort of patients with known clinical outcomes in order to predict disease progression or other clinical endpoints. Genomic testing has the potential of improving risk stratification over clinical pre-treatment methods such as the commonly used NCCN guidelines, D’Amico classification, and CAPSURE system.
Androgen deprivation therapy
As with all of the definitive treatment options (e.g., surgery, radiation, high intensity focused ultrasound), several contingency treatments are available for those who progress despite appropriate management on watchful waiting or active surveillance protocols. As such, androgen deprivation therapy (ADT) deserves particular mention. When the cancer has progressed, ADT is used to suppress further growth of cancerous cells by depriving androgens needed for their survival. In addition to slowing the growth of cancer, ADT can reduce associated pain and extend life. ADT drugs include LHRH agonists such as goserelin (Zoladex ®), histrelin (Vantas ®), leuprolide (Lupron ®, Eligard ®), and triptorelin (Trelstar ®) as well as LHRH antagonists like degarelix (Firmagon ®) and abiraterone (Zytiga ®), enzalutamide (Xandi) and apalutamide (Erleada).16 Although ADT is associated with some significant symptoms and health risks, these risks have decreasing concern in men advancing age. ADT may also be suitable for men with symptomatic or higher risk localized disease who are not candidates for surgery or radiation due to their limited life expectancy and other serious health conditions.
The long-term results of watchful waiting compared to those of active surveillance and definitive treatment are not yet conclusive. Although it is not always clear which “expectant management” option patients should pursue, i.e., watchful waiting versus active surveillance, physicians should recognize that active surveillance patients are much more likely to eventually choose definitive therapy. However, these latter patients will still have benefited from a period of freedom from the potential side effects of definitive therapy. Also, this additional time allows for further emotional acceptance of the disease and facilitates more opportunity for informed decisions. Certainly, watchful waiting or active surveillance are not a one-size-fits-all approach for men with low grade, low stage prostate cancer. Nevertheless, watchful waiting and active surveillance have the potential to play an increasingly important role in the management of prostate cancer as less advanced disease is detected and methods are refined for identifying low-risk patients. Each man and his physician should have a careful discussion of the benefits versus the risks of watchful waiting at the time of diagnosis in order to select the most suitable option.
None.
Authors declare there is no conflicts of interest.

©2018 Miller, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.