eISSN: 2378-3176


Case Report Volume 7 Issue 1
Department of Nephrology Madras Medical Mission India
Correspondence: Georgi Abraham MD FRCP L FRCP G Department of Nephrology Madras medical mission Chennai 4 a Dr JJ Nagar Mogappair Chennai 600037 India, Tel +919841710992
Received: December 27, 2018 | Published: February 8, 2019
Citation: Yuvaraj A, Vijayan M, Mathew M, et al. Unusual cause of bilateral lower limb edema in a male with ADPKD. Urol Nephrol Open Access J. 2019;7(1):4-6. DOI: 10.15406/unoaj.2019.07.00232
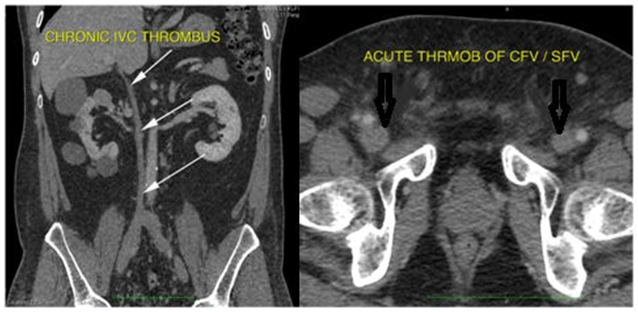
A 53 year old male presented with vague pain and worsening swelling of both lower limbs since one week. Venous doppler study of lower limbs unmasked DVT involving bilateral saphenofemoral, superficial popliteal and popliteal veins with a high total plasma homocysteine of 29.76umol/L (5.46-16.20umol/L. CT Venogram showed chronic thrombosis of the IVC and bilateral renal veins with acute thrombosis in bilateral common iliac, external/internal iliac, bilateral common femoral and superficial femoral veins. Colonoscopy showed multiple colonic diverticulae. 2-D ECHO showed myxomatous AML suggestive of mitral valve prolapsed (MVP).
Keywords: polycystic kidneys, deep vein thrombosis, homocysteine, colonic diverticulae, mitral valve prolapse
A 53 year old male vegetarian, not diabetic or hypertensive and did not have a history of cardiovascular, hepatic or kidney disease, presented to us with vague pain and worsening swelling of both lower limbs since 1 week. Physical examination was unremarkable except for bilateral tender pitting edema of feet, legs and thigh. Investigations showed Hb 116g/L,WBC count 8.9 X 109/L, platelet 301 X 109/L, ESR 72mm/hr, blood urea nitrogen 21mmol/L, serum creatinine 132 micromol/L, Urine albumin nil. Saturation was 98% in room air. Chest X ray was unremarkable. Venous doppler study of lower limbs unmasked DVT involving bilateral saphenofemoral, superficial popliteal and popliteal veins with normal arterial doppler. Tc-99m lung perfusion was normal. LFT, fasting lipid profile, electrolytes and thyroid function were normal. HIV, HBsAg and anti HCV were negative. Protein C, protein S activity, antithrombin III, factor V leiden mutation, APLA were unremarkable but a high total plasma homocysteine of 29.76umol/L(5.46-16.20umol/L). B12 level was low (188pg/ml) and he was given IM. methylcobalamin 1000mcg for 7 days. CT Venogram showed chronic thrombosis of the IVC and bilateral renal veins with acute thrombosis in bilateral common iliac, external/internal iliac, bilateral common femoral and superficial femoral veins (Figure 1).
CT Abdomen with contrast showed right kidney 10X6.1cm with >10cysts, Left kidney 9.6X5.1cm with 3-4 cysts, the largest cyst on either side measuring about 6cm (Figure 2). Tc-99m Isotope renogram scan revealed total GFR 65ml/min (left kidney 52ml/min, right kidney 13ml/min).

Prostate malignancy was ruled out. Plasma CEA and CA19-9 were normal, stool occult blood negative, upper GI endoscopy showed gastric ulcer with duodenal erosions with biopsy from lesions ruling out malignancy, colonoscopy showed multiple colonic diverticula (Figure 3).
2-D ECHO showed good biventricular function, EF-62%, type 1 diastolic dysfunction, myxomatous AML suggestive of mitral valve prolapse(MVP) (Figure 4).
He was treated with Inj. Enoxaparin 60mg s/c BID followed by oral warfarin to maintain the PTINR between 2 and 3. Patient also received additional B6 and folic acid for hyperhomocystinaemia.
Venous thrombosis and hypercoagubility is a common complication of malignancy1 and hypoplasia of the IVC, described as an incidental finding, should be taken into account when otherwise unexplained DVT develops in young people.2 Hyperhomocysteinemia is a risk factor for recurrent venous thrombosis in patients between 20 and 70 years of age.3 Our patient had a hypoplastic IVC as depicted by thinned out IVC with mild to moderate hyperhomocystinaemia explaining the probable cause for venous thrombosis. However an extensive workup to detect malignancy was negative.
ADPKD is associated with MVP in up to 25%.4 There are rare case reports of thrombosis in the inferior vena cava (IVC) due to enlarged cysts in autosomal dominant polycystic kidney disease.5 Our patient showed number of cysts to meet the required criteria for ADPKD6, with Stage II CKD, MVP, multiple colonic diverticulae and IVC thrombosis, had no positive family history, with only elder brother having late onset minimal change disease. Genetic workup for ADPKD is done. Literature review did not show association of IVC hypoplasia with cystic kidney disease.
None
Authors declare there is no conflict of interest.

©2019 Yuvaraj, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.