eISSN: 2378-3176


Case Report Volume 4 Issue 5
Urology Department, King Fahd Central Hospital, Saudi Arabia
Correspondence: Alaa Mohamed Shaaban, Professor of Urology Minia University, Egypt, Consultant Urology, King Fahd Central Hospital, Gizan, Saudi Arabia, Tel 966597714417
Received: April 27, 2017 | Published: May 29, 2017
Citation: Alfaifi H, Abuazzawayed I, Abdelhafeiz A, et al. Spontaneous intraperitoneal bladder rupture, a report of two cases. Urol Nephrol Open Access J. 2017;4(5):173-175. DOI: 10.15406/unoaj.2017.04.00146
Introduction:Spontaneous bladder rupture (SBR) is a rare surgical emergency that occurs mostly in men with infravesical obstruction in presence of pathological bladder. Delayed and misdiagnosis of such clinical condition may lead to high morbidity and mortality rates. We here in present two cases with SBR.
Case presentation: The first case is a 54 year old male presented with peritonitis and high creatinine level. This patient was misdiagnosed as perforated viscus but exploration revealed intraperitoneal bladder rupture which was secondary to prolonged infravesical obstruction (urethral stricture). The Second case was a 65 year old female that was referred from a peripheral hospital comatosed, desaturated and intubated. Patient had intraperitoneal bladder perforation and urinary ascites that was diagnosed by non-contrast CT cystogram. On exploration Bladder was contracted and inflamed that may be the underlying cause of SBR.
Conclusion:SBR is a devastating and life threatening clinical condition. It is usually difficult to recognize preoperatively, so it has to be kept in mind among other causes of acute peritonitis.
Keywords: Infravesical obstruction; Bladder; Intraperitoneal; rupture; Spontaneous
Bladder rupture occurs usually following trauma. The normal anatomical position in the true pelvis and its elasticity are protective [1]. On the other hand, spontaneous rupture of the native non-malignant bladder is extremely rare and life threatening clinical condition [2]. It is more common in men with infravesical obstruction. These cases are usually overlooked and presented with peritonitis, high serum creatinine with high mortality rate up to 50% [3]. Predisposing causes for spontaneous bladder rupture (SBR) include: inflammation, tumor, tuberculosis, stones, diverticulum or surgical scar [3]. Other predisposing causes are altered sensitivity [4], radiotherapy [5,6] and obstructed labor [7,8]. We present 2 cases of spontaneous bladder rupture, one male and one female.
A 54 year old male presented to peripheral hospital with peritonitis and septic shock according to the referral report. Non- contrast CT was done there and showed free intraperitoneal fluid collection with big vesical stone (4.5 cm) and 3 stones in the proximal bulbar urethra (12, 4 and 2 mm). Laboratory investigations were done where serum creatinine, blood urea nitrogen (BUN), hemoglobin (HB) and White blood cells (WBCS) were 551 mg/dl /l, 41 mmol/l, 13gm and 30000 respectively. Patient was diagnosed as perforated viscus and shifted to operating room (OR) where exploratory laparotomy was done and showed moderate intraperitoneal collection with multiple adhesions and pockets of pus, congested bowel loops with no signs of perforation. A large urinary bladder perforation about 3 cm was found at the bladder dome through which the vesical stone was extracted and a trial for urethral catheter insertion was failed. The urologist was not able to push the bulbar stone back into the bladder, so the edges of the perforation was refreshed and closed with 2/0 polyglactin in 2 layers with insertion of suprapubic Foley's catheter (SPC). Lavage was performed for the peritoneal cavity and the wound was closed with drainage.
Post-operatively, The SPC was not draining well with persistent suprapubic urine leakage, so the patient was referred to our hospital 2 weeks following the primary surgery. On examination; patient was conscious, well- oriented with average general condition. Abdominal examination showed gapping of suprapubic wound with leakage of turbid urine; the SPC was not functioning well. A stone was felt in the bulbar urethra during perineal examination. Patient gave history of left nephrectomy 2 years before for a nonfunctioning kidney. Serum creatinine, BUN, HB, and WBCs were 64 mg/dl, 3.4 mmol/l , 9.9 gm, and 6640 respectively. Non- contrast CT showed no intraperitoneal fluid collection, right moderate hydroureteronephrosis, dilated left ureter with 2 stones in its lower end and 3 stones in the proximal bulbar urethra (Figure 1). Retrograde urethrocystogram showed a 3 cm stricture segment at the distal bulbar urethra and another annular stricture at the proximal bulbar urethra in addition to an urethral diverticulum in between containing the stone and grade 4 right vesico-ureteral reflux (Figure 2).

Patient was then booked for endoscopy and possible exploration. Visual internal urethrotomy was done for the proximal and distal bulbar strictures, the neck of the urethral diverticulum was seen with the stone inside. An 18 Fr. urethral catheter was passed through the urethra to the bladder and the patient was placed in the lithotomy position where the urethral diverticulum was excised together with the stones through a small perineal incision. Post-operatively, the patient was shifted to the surgical ward and parenteral antibiotic was given for 7 days according to the result of culture and sensitivity of the pre-operative wound discharge. Post-operative recovery was uneventful and the suprapubic wound became clean, dry and healed by secondary intention. Patient was discharged 7 days post-operatively with the urethral catheter which was removed one week later in the outpatient clinic, thereafter the patient voided well and scheduled for follow up.
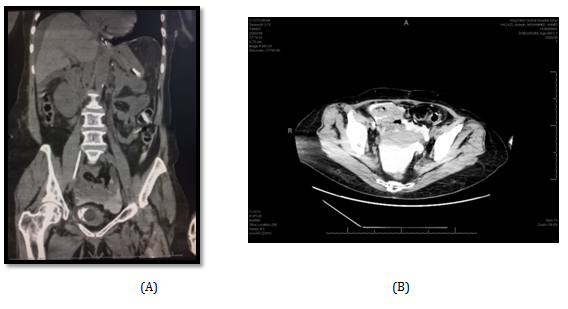
A 65 year old female referred from a peripheral hospital to the emergency comatosed, desaturated and intubated. Her relative gave history of long standing hypertension. On examination; patient was afebrile, intubated, Blood pressure was 160/100.Laboratory investigations were done and revealed a serum creatinine of 1990umol/l, BUN 74 mmol/l, serum K 6.3 mmol/l, Hb 8.2 gm, and WBCs 20110. Patient was admitted in ICU and diagnosed as uremic encephalopathy with pulmonary edema. Glasgow Comma Scale (GCS) was 8/15 and urethral catheter which was already placed drained 1000 ml/ 24 hours, turbid urine. Proper parenteral antibiotic was given according to culture and sensitivity test and patient underwent one session of hemodialysis(HD). Thereafter, serum creatinine dropped to 1002 mg/dl should be placed) BUN 54.3mmo/l and serum K 3.7 mmol/l. Non-contrast CT scan was performed combined with retrograde cystogram and showed mild bilateral backpressure, intra-abdominal free fluid collection and extravasation of contrast into the pelvis and abdominal cavity (Figure 3A & B).
Patient was shifted to OR on the next day where cystoscopy was done first and showed small sized bladder with perforation in the upper part of the posterior bladder wall, so exploratory laparotomy was done and showed moderate amount of intraperitoneal turbid fluid and perforation in the posterior wall of UB near the dome (about 2.5cm) with inflamed edges. Biopsy was taken from the edges of the perforation and sent for histopathology that showed later only inflammatory reaction with no malignancy. The edges of the perforation was then closed with 2/0 polyglactin sutures in 2 layers. The bladder capacity was markedly reduced, so only urethral catheter was left for drainage. After peritoneal lavage, the wound was closed with intraperitoneal drainage. Patient was then shifted to the surgical ICU, then 2 days later she was transferred to the surgical ward. Post-operative recovery of the patient was uneventful. Patient has been improved and regained consciousness. Average urine output was 1800 ml/24 hours, patient started oral fluid on the 3rd post-operative day and commenced normal diet on the 5th day. Parenteral antibiotic continued for 7 days and the patient was discharged home on the 11th postoperative day with a serum creatinine of 229 umol/l, BUN 8.5 mmol/l, serum K3.4 mmol/l and Hb 9gm.
Spontaneous Bladder Rupture (SBR) is a rare and extremely urgent surgical emergency that is often life threatening especially when diagnosis is delayed. These cases are usually overlooked and should be suspected when the predominating symptoms include acute peritonitis, sudden abdominal pain, peritoneal cavity fluid, oliguria, hematuria with increased serum creatinine, BUN and potassium levels [9]. Most of the reported cases occurred in men with infravesical obstruction [1,3,10]. However, few cases of SBR has been reported in females during or shortly after obstructed labor [7,8]. Other predisposing factors include inflammation of the bladder, tumor, stones and surgical scar [3]. Games et al. [4] reported SBR due to altered bladder sensation following alcoholism.
In our first reported case, the underlying cause of SBR was prolonged infravesical obstruction due to urethral stricture with subsequent cystitis, stone formation and weakness of detrusor. The case was diagnosed as peritonitis possibly due to perforated viscus. CT is the standard for diagnosis of intraperitoneal fluid collection but it cannot determine the cause or detect bladder wall perforation. On the other hand, CT cystogram is the gold standard for diagnosis by demonstrating the migration of contrast into the peritoneal cavity.(10) Serum creatinine is significantly increased in SBR as a result of urinary ascitis, combined with hypovolaemia [10]. In the second presented case cause of perforation was due to contracted bladder with subsequent chronic cystitis. The high incidence of suspicion had led to early diagnosis and accurate management of the case despite of late presentation to our hospital. Treatment of SBR include 2 layer closure of debrided perforation edges, urinary drainage by urethral catheter or SPC or both and adequate management of the predisposing cause either immediate or by delayed surgery.
SBR is a devastating clinical emergency that is usually overlooked and may be misdiagnosed as gastrointestinal tract perforation. A high index of suspicion is always required for correct diagnosis and early treatment. Non-contrast CT cystogram is the gold standard for the diagnosis.

©2017 Alfaifi, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.