eISSN: 2378-3176


Research Article Volume 5 Issue 6
1Department of urology, Federal clinical center of high medical technology of FMBA of Russia, Russia
2Department of Urology and Andrology, IPPE of AI Burnazyan SSC FMBC of FMBA of Russia, Russia
Correspondence: Alexey Kaputovskij, Urologist, Department of urology Federal clinical center of high medical technology of FMBA of Russia, Novogors district, Khimki, Moscow region, 141435, Russia, Tel 7 916 923 91 85
Received: November 19, 2017 | Published: December 19, 2017
Citation: Biktimirov RG, Martov AG, Kaputovskij AA, Biktimirov TR (2017) Minimal Invasive Simple Prostatectomy for Treatment Benign Prostate Hyperplasia with Volume Over 80 Ml: The Smart Option for Simultaneous Surgery. Urol Nephrol Open Access J 5(6): 00191. DOI: 10.15406/unoaj.2017.05.00191
Introduction: Open simple prostatectomy, holmium laser enucleation and bipolar enucleation are current standard for surgical treatment of benign prostatic hyperplasia (BPH) with volume over 80 ml. Minimal invasive simple prostatectomy (MISP) remains under evaluation and more data are required. The authors describe own experience using of MISP for surgical treatment of BPH.
Materials and methods: The data of 79 patients, who underwent laparoscopic extraperitoneal transcapsular simple prostatectomy from 2011 to 2016, were analyzed retrospectively. Shapiro-Wilk test and Fisher’s exact test were used for statistical analysis.
Results: The mean age was 68 (range from 53 to 84) years, the mean preoperative prostate volume was 134 (range from 80-300cc), the mean operative time was 206 (range from 100 to 450) minutes, and the mean blood loss was 256 (range from 30 to 1200) ml. The improvement of IPSS was minus 18, 3 points; Qmax was plus 12 ml/s, V res dropped from 147 ml to 28 ml. Postoperative complications rate was 12.6% (10 patients). There was no conversion to open surgery. One case of incidental prostate cancer. There has not been reoperation for bladder outlet obstruction during ear follow up. Patient’s database was divided into two study groups. Group I, only MISP – 44 (46%) patients. Group II MISP plus simultaneous procedures - 35(44%) patients (mainly inguinal hernia and cystolithotomy). No statistically significant differences were found in age of patients, prostate volume, complications, and blood loss between the two study groups. The significant difference was found in the duration of the operation (group I (mean) – 185 min; group II (mean) -230 min p<0.05).
Conclusion: Minimally invasive simple prostatectomy is a safe and efficacy. It may be smart way for simultaneous surgical treatment BPH and contaminant condition.
Keywords: benign prostatic hyperplasia; minimally invasive simple prostatectomy; open simple prostatectomy
BPH, benign prostatic hyperplasia; MISP, minimal invasive simple prostatectomy; TUR, transurethral resection; DRE, digital rectal examination; PSA, prostate specific antigen; IPSS, the international prostate symptom score
Open simple prostatectomy, holmium laser enucleation and bipolar enucleation are current standard for surgical treatment of benign prostatic hyperplasia (BPH) with volume over 80 ml. The laser vaporization, thulium enucleation and (TUR) may be second line. MISP remains under evaluation and more data are required.1 Some systematic review and meta-analysis shows benefits MISP versus open surgery. The benefits are less blood loss, shorter hospital stage, but MISP requires more operation’s time.2 Laparoscopic and extraperitoneal approaches are used, only laparoscopic or robot-assisted with transcapsular, transvesical and transvesical-prostatic access to adenomas.3-8 The authors describe own experience using of MISP for surgical treatment of BPH. The distinctive sing of our study is advanced using minimal invasive approach for simultaneous procedures.
The data of 79 patients, who underwent laparoscopic extraperitoneal transcapsular simple prostatectomy from 2011 to 2016, were analyzed retrospectively. We have not used open simple prostatectomy since 2011. MISP and monopolar TUR are utilizing. Before the surgery, history taking, physical examination, digital rectal examination (DRE), routine lab tests, IPSS, ultrasonography, prostate-specific antigen (PSA) measurement, uroflowmetry and were performed. General anesthesia was performed for MISP in the Trendelenburg position with bilateral arms at each side. In other words, patient, surgeons and equipment locations are same with laparoscopic radical prostatectomy. The Foley catheter was introduced into the bladder, and the skin was incised 1 to 1.5 cm along the fold beneath the umbilicus. The anterior sheath of the rectus abdominis muscle was transversely incised. After incision, the rectus muscle was exposed and spread bilaterally to expose the posterior sheath. Digital dissection of the preperitoneal space was performed. A balloon dilatator with a 10 mm-trocar was inserted between the rectus abdominis muscle and the posterior sheath, and the balloon was inflated with air to get enough extraperitoneal space under the direct vision. Placement of five trocars in an inverted U-shape were used (Figure 1).

Figure 1 The placement of surgeons and trocars (№1- surgeon, №2- assistant, №3- camera- assistant; red circles - 5 mm trocars; white with black border – 10 mm trocars).
The main steps of MISP were:
Step 1
Extraperitoneal dissection of the Retzius space (the endopelvic fascia was not opened). We have made preparation for inguinal hernia repair during this step.
Step 2
The completely dissection of the fat covering the prostatic capsule the boundary between the bladder and the prostate was clearly identified by moving the Foley catheter.
Step 3
The capsular incision was made on the anterior part of the prostatic capsule until the plane between the surgical prostate capsule and the adenomatous tissue was exposed. Ultrasound or monopolar energy was used for incision. Bipolar coagulation was used for large venous vessels (Figure 2).
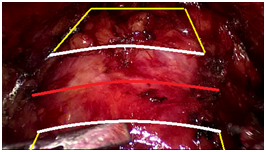
Figure 2 The scheme of prostatic capsule incision (red line - line of incision, yellow and white shapes are boundary of prostatic venous complex and bladder neck).
Step 4
The adenoma dissection along the surgical capsular plane in the same fashion as the open procedure. Once the catheter was identified, the dissection proceeded until the completely adenomatous tissue had been freed. We divided the adenomatous tissue into two lobes (right and left) to ease its dissection and posterior excision. The Foley catheter may be removed for manipulation that is more convenient. The median lobe removed with bladder mucosa. The ureteral orifices must be clear identified. After excision of the adenoma, the specimens were placed in the endobag sack. The bleeding of the prostatic capsule and prostatic fossa was controlled by bipolar or monopolar energy (Figure 3).
Step 5
The trigonization of prostatic fossa (Vicryl 3-0 running sutures) and the Foley catheter replacement.
Step 6
The anterior prostatic capsule incision was closed by barbed suture. Saline solution was irrigated through the Foley catheter, and the bladder was filled with the saline solution to check whether the sutured region leaked. The specimen was finally removed through the 10 mm port site beneath the umbilicus. As for a large adenoma, a wider dissection was applied to allow for an intact retrieval. The polypropylene allograft (size 10x15 cm) was used for inguinal hernia repair with hernia stapler fixation. We removed stones from separate urinary bladder incision (Figure 4). Complications were recorded with the Clavien-Dindo system. Shapiro-Wilk test and Fisher’s exact test were used for statistical analysis, p-values of <0.05 were considered statistically significant.
The mean age was 68 (range from 53 to 84) years, the mean preoperative prostate volume was 134 (range from 80-300cc), the mean operative time was 206 (range from 100 to 450) minutes, and the mean blood loss was 256 (range from 30 to 1200) ml. The improvement of IPSS was minus 18, 3 points; Qmax was plus 12 ml/s, Vres dropped from 147 ml to 28 ml. Simultaneous procedures were in 35(44%) cases. Intraoperative complication was recorded in one case. It was damage ofprostatic venous complex brunch without consequences. Postoperative complications rate was 12.6% (10 patients). Grade IIIb and IVa were occurred in five cases. There was no conversion to open surgery. One case of incidental prostate cancer. There has not been reoperation for bladder outlet obstruction (follow up period was a year). Patient’s database was divided into two study groups. Group I, only MISP - 44 (46%) patients. Group II MISP plus simultaneous procedures - 35(44%) patients. Simultaneous procedures were inguinal hernia repair unilateral -10; inguinal hernia repair bilateral -3; cystolithotomy-16; cystolithotomy and ureterolithotomy-1; cystolithotomy and inguinal hernia repair-3; diverticulectomy and cystolithotomy -1; diverticulectomy -1. The same surgical approach was used for simultaneous procedures. No statistically significant differences were found in age of patients, prostate volume, blood loss and complications between the two study groups. The significant difference was found in the duration of the operation (group I (mean) - 185 min; group II (mean) -230 min p<0.05).
Minimally invasive simple prostatectomy is a safe and efficacy. It may be smart way for simultaneous surgical treatment BPH and contaminant condition.
None.
The author declares there is no conflict of interest.

©2017 Biktimirov, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.