eISSN: 2378-3176


Case Report Volume 3 Issue 2
1Department of Nephrology, Urology & Nephrology center, Egypt
2Department of Radiology, Urology & Nephrology center, Egypt
Correspondence: Ahmed Akl, Urology & Nephrology center, Mansoura, Egypt
Received: March 01, 2016 | Published: February 23, 2016
Citation: Akl AI, Megahed MA, El Hadedy MA, et al. Improvement of renovascular malignant hypertension after angioplasty. Urol Nephrol Open Access J. 2016;3(2):39-42. DOI: 10.15406/unoaj.2016.03.00069
Malignant hypertension in young female with disparity in kidney size raise the attention toward non-essential renovascular hypertension. In this case we describe a young female suffered severe hypertension associated with deterioration of kidney function and disparity in kidney size by ultrasound. Hemodialysis was started because of electrolytes imbalance and fluid overload which is unusual with unilateral renal artery stenosis. Management by traditional antihypertensive medication was with limited benefit and patient condition required intensive care monitoring. Balloon dilatation angioplasty with stent insertion in the left renal artery was performed, blood pressure started to respond to anti-hypertensive medications but she became anuric. Daily hemodialysis session was done, after few days her condition started to improve and serum creatinine returned to normal base 1.1mg/dl without dialysis support. The patient presentation was not classic toward either unilateral renal artery stenosis or reno-parenchymal disease.
Keywords: secondary hypertension, malignant hypertension, renal artery stenosis, interventional radiology, angioplasty
RAS, renal artery stenosis; RAAS, renin-angiotensin-aldosterone system; US, ultrasonography; PTA, percutaneous transluminal angioplasty; FMD, fibromuscular dysplasia; ASTRAL, angioplasty and stenting for renal artery lesions
Renal artery stenosis (RAS) is a common treatable cause of hypertension and is on the increase in the present population due to atherosclerosis and associated risk factors.1 Current treatment measures include lifestyle with medical management, revascularization using angioplasty (+/−stenting) and bypass surgery. Since leading experiment in 1934, RAS has increasingly been recognized as an important cause of clinically atypical hypertension and chronic kidney disease, the latter by virtue of renal ischemia. RAS is the clinical consequence of activation of the renin-angiotensin-aldosterone system (RAAS). Renal artery occlusion creates ischemia, which triggers the release of renin and a secondary elevation in blood pressure. Hyper-reninemia promotes conversion of angiotensin I to angiotensin II, causing severe vasoconstriction and aldosterone release. The ensuing cascade of events varies, depending on the presence of a functioning contralateral kidney.2 When two kidneys are present, aldosterone-mediated sodium and water retention is handled properly by the non-stenotic kidney, precluding volume from contributing to the angiotensin II–mediated hypertension. By contrast, a solitary ischemic kidney has little or no capacity for sodium and water excretion; hence, volume plays an additive role in the hypertension. Herein, we describe a rare case with unilateral renal artery stenosis and malignant hypertension.
A 26-year-old female presented with severe hypertension blood pressure 190/120mmHg, with disparity in kidney size by ultrasonography (US). Doppler US revealed left renal artery dampened wave suggesting renal artery stenosis. Isotope renogram was carried out and revealed poor uptake & excretion of TC-99m-MAG3 by left kidney & impaired right kidney (Figure 1). Doppler US carotids were normal. Poor kidney function, serum creatinine 5.9gm/dl rose in two days to 8mg/dl with electrolytes imbalance; K+ 5.9mg/dl, PH 7.2 and urine output was less than 400 ml/day. Acute kidney injury was suspected, hemodialysis initiated to improve general condition and prepare patient to renal biopsy from the right kidney. However, blood pressure never been ameliorated neither pharmacological nor by ultra filtration with shooting up to 240mmHg systolic/130mmHg diastolic that endangered patient life. Tight monitoring in the intensive care unit, glyceryl trinitrate infusion was started and titrated to control blood pressure; immediate angiography was carried out once blood pressure reached 160/110mmHg and revealed long stenotic segment of left renal artery and poor-perfused kidney (Figure 2A).
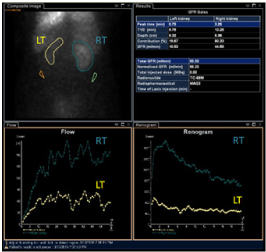
Figure 1 Poor perfused left kidney (LT) with poor excretion of TC-99m compared to right kidney (RT) on isotope renogram.
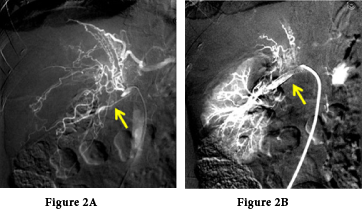
Figure 2 Left renal artery angiography. A) Non perfused left kidney with severe left renal artery stenosis, collaterals are noted on angiography. B) Perfused left kidney after balloon dilatation and stent insertion on angioplasty.
Balloon angioplasty was done followed by stent insertion to maintain renal artery dilatation (Figure 2B). Patient was referred back to ICU; and blood pressure started to be under control by oral antihypertensive medications only. However, patient became anuric, hemodialysis sessions maintained to control fluid overload and improve general condition, serum creatinine reached 12.6mg/dl. Hemoglobin 8.6g/l but with no evidence of bleeding, erythropoietin was not initiated because of hypertension. In the following days blood pressure improved dramatically that enabled successful weaning of antihypertensive medications, urine output started to increase with spontaneous drop of serum creatinine without performing hemodialysis. In two weeks, blood pressure was maintained at systolic 120mmHg/80mmHg diastolic without antihypertensive medication with normal serum creatinine 1.1mg/dl and hemoglobin 11g/l on discharge from hospital (Figure 3).
Renal Artery stenosis is a common cause of hypertension and impaired renal function. There have been advances in both medical treatment and endovascular techniques used in the treatment of reno-vascular hypertension.1 The debate is ongoing as to the preferred method of treatment especially with regard to endovascular intervention. The invasive and surgical options for treatment of RVHT include percutaneous transluminal angioplasty (PTA), surgical revascularization, and nephrectomy. Intravascular stents may be placed during angioplasty, although research has called the clinical benefit of this into question.3
In adults, reno-vascular disease tends to appear at different times and affects the sexes differently. Atherosclerotic disease affects mainly the proximal third of the main renal artery and is most common among older men. Fibromuscular dysplasia (FMD) involves the distal two thirds and branches of the renal arteries and is most common among younger women.4 FMD involves fibrous or muscular hypertrophy of the vessel tunica media with fibrous intimal hyperplasia; accordingly, it is sometimes referred to as fibromuscular hyperplasia. Often, post-stenotic dilatation is also present. The process may range from mild occlusion to complete occlusion of the vessel. On radiographs, FMD produces the classic string-of-beads appearance less often in children than in adults; rather, it tends to show short discrete or longer tubular segments of stenosis.5
Previously there has been much controversy in the timing and methods of initiating revascularization in cases of renal artery stenosis.1 There have been a number of studies looking at the benefit of angioplasty compared with medical treatment in renal artery stenosis. Most of the studies were small and the majority showed there was no significant difference in outcome with angioplasty when compared to medical treatment.6–8 This was shown in a recent large study, the Angioplasty and Stenting for Renal Artery Lesions (ASTRAL) study.9 This was a large randomized control trial comprising patients with atherosclerotic reno-vascular disease who then underwent revascularization and medical therapy or medical therapy alone. Over 5years it still found no evidence to suggest clinical benefit from revascularization as opposed to medical therapy.9 However, the study itself has been heavily criticized, especially with regards to its methodology.10
All studies so far regarding renal revascularization have had significant flaws and bias, and have given no conclusive evidence as to the indications for angioplasty or the best treatment of renal artery stenosis. CORAL trial has been started to compare revascularization with medical therapy in patients with clear indications for renal artery revascularization.11 These results may give a more definite answer. Long-term maintenance of blood pressure improvement ranges from 38% to 90%. Guzzetta et al.,12 and Tyagi et al.,13 found that approximately 25% of patients treated with PTRA developed restenosis. Casalini et al, evaluating PTRA in a selected group of 36 children with RVHT, found that 34 (94%) of the patients were normotensive 2years after the procedure.14 Placement of intravascular stents during angioplasty may be helpful in preventing re-stenosis and managing RVHT. Primary renal artery stenting in patients with atherosclerotic RAS has a high rate of technical success and a low rate of complications.15,16
In case of renal artery stenosis where there is malignant hypertension and where individuals have normal renal function prior to angioplasty, it has been suggested that early surgical intervention is beneficial.17 However, in our case renal function was impaired. Percutaneous Transluminal Angioplasty (PTA) and stenting has long been used as a revascularization technique in renal artery stenosis and has gradually replaced open surgical procedures. Despite inconclusive evidence of the benefits of angioplasty in renal artery stenosis, this technique has been increasingly used for treatment of renovascular hypertension. Our case shows good outcome of angioplasty balloon dilatation and stent insertion in unilateral renal artery stenosis. However, contrast nephropathy risk was inevitable, overcome by the improvement in renal perfusion and normalization of hypertension.
We present a case with life threatening malignant hypertension, intensive blood pressure control associated with angioplasty balloon dilatation and stent insertion lead to control of blood pressure and normal kidney function.
None.
The author declares no conflict of interest.

©2016 Akl, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.