eISSN: 2378-3176


Research Article Volume 11 Issue 3
Urology department, Aswan University Hospital, Aswan, Egypt
Correspondence: Mohmad Zaki El-Dahshoury, Prof. of urology & reconstructive urethral surgery, Urology department, Aswan university, Aswan-Egypt, Tel +20101636576
Received: September 10, 2023 | Published: September 27, 2023
Citation: El Dahshoury ZM, Hanna P. Different techniques in management of navicular fossa stricture, a single institution experience. Urol Nephrol Open Access J. 2023;11(3):89-93. DOI: 10.15406/unoaj.2023.11.00339
Background: Evaluation of the functional and cosmetic results after repair of different cases with fossa navicularis stricture by different techniques of urethroplasty.
Methods: This study included 43 male patients with different lengths of fossa navicularis stricture of different age groups (8-60 years). History, clinical examination, ascending urethrogram (AUG), and voiding cystourethrogram (VUG) were reported for all patients. Primary outcome was functional assessment using AUG and VUG. Secondary outcomes were cosmetic evaluation using the HOSE score and 90-day complications. Follow-up duration was 2 years (at the 6th month, the end of the first year, and the end of the second year) by clinical examination, flow rate, urethrogram, and urethrocystoscopy.
Results: Cosmetic and functional success was achieved in 39 patients (90.6%). Follow-up was for 24 months. The flow rate had improved up to 15.3ml/sec. Four patients developed complications, one patient with restricture, two patients with subcoronal fistula, and one with glanular disruption.
Conclusion: Different techniques were used for the repair of fossa navicularis stricture. The choice of suitable technique was according to different findings such as length of stricture, urethral caliber, associated Lichen sclerosus (LS), availability of penile skin, and hair distribution. The technique of repairing fossa navicularis stricture with the use of the transverse penile island flap with the glans cap keeps the glanular shape and configuration intact with optimum function.
Keywords: fossa navicularis, glans cap technique, urethral stricture, flap urethroplasty
AUG, ascending urethrogram; VUG, voiding cystourethrogram; LS, lichen sclerosus; VIU, visual internal urethrotomy; TURP, transurethral resection of prostate
Fossa navicularis stricture is a chronic urethral disease affecting all ages. Fossa navicularis stricture is a subcategory of anterior urethral stricture with unique characteristics in terms of treatment options that entail restoring functional urethra and cosmetically appealing glans.1 Treatment options are dilatation, meatotomy, and open reconstruction. Urethral dilatation has no role in the treatment of fossa navicularis stricture. Meatotomy results in a hypospadiac urethral meatus and disfigurements. Not all meatoplasties can achieve both satisfactory cosmetic results and urinary stream without spraying.2
The successful surgical repair of fossa navicularis stricture depends on the careful selection of non-diseased tissue for substitution. The healthy penile skin is the most suitable tissue substitute as it is characterized by a well-vascularized pedicle, non-hair bearing, and no contraction.3 If penile skin is unsuitable, (inflamed, scarred, deficient, or hairy), extragenital tissues such as (buccal mucosa, skin graft) or synthetic such as submucosal intestinal matrix are perfect alternatives to compensate for the strictured segment. Tissue transfer techniques should be considered for either augmentation of the dorsal or ventral aspects of the urethra or the whole urethral replacement and may be in one stage or two stages.4
Finally, the choice of glanuloplasty is particularly important in achieving a good cosmesis. A glans-cap repair is preferred because of the limited dissection required with this relatively simple and bloodless technique. A good selection of suitable urethral substitutes and the technique of glanular reconstruction is essential for the successful repair of fossa navicularis stricture.4 Therefore, we sought to evaluate the functional and cosmetic outcomes of different surgical techniques in management of fossa navicular stricture.
Between 2016 to 2020, a retrospective cohort study involved 43 male patients with fossa navicularis stricture at Urology Department at Aswan University Hospital. All patients were evaluated with uroflowmetry, and the mean peak flow rate was 9±2ml/sec. A preoperative retrograde urethrogram was performed in all patients to exclude proximal urethral strictures. The median follow-up duration was 24 months. Clinical examination, flow rate, urethrogram & urethrocystoscopy (if indicated) were performed for all patients at six months, the first year, and at the end of the second year.
Surgical technique
33 patients were managed by transverse penile island flap (with glans cap technique in 22 patients and split glanuloplasty among the other 11 patients), 4 patients were managed by Orandi repair, 3 patients had buccal mucosal graft, and the last 3 patients (LS) treated by 2 stages repair buccal graft. All urethroplasties were performed by a single surgeon. In the first 22 patients, exposure was done through a short transverse incision on the ventrum of the penis 0.5cm proximal to the coronal sulcus. The glans was dissected in the plane between the glans and corpus spongiosum to the site of the meatus as in supplementary Figure S1A. The incision was created ventrally and lateral around the urethral meatus down to the sub-urethral plane to connect with the proximal plane of dissection over the corpus spongiosum, so easy to access all the strictured fossa navicularis without disturbance of the glanular shape. A tunnel was created between the glans and the urethra and ventral stricturotomy along the strictured fossa navicularis till the healthy penile urethra as in Figure S1B. A ventral transverse penile island skin flap was outlined with a dimension according to the urethral caliber and length needed in Figure S2. Elevation of the ventral aspect of the glans with stay suture so all the strictured fossa navicularis could be exposed. The transverse penile island flap was rotated 90 to be vertically oriented over the strictured segment. The flap was sutured to the urethral edges starting proximally to distally till the meatus with interrupted 6-0 Vicryl sutures as in Figure S3A-S3B. Dartous layer was sutured over the anastomotic line. The elevated glans was fixed to the underneath tissues in its place so that its configuration was not disturbed. The subcoronal incision was approximated with 6-0 Vicryl. A suitable silicone urethral catheter was inserted for 3 weeks.
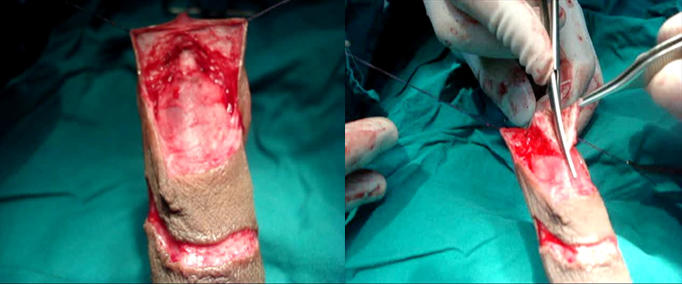
Figure S1A Plane of dissection created between the glans and the corpus spongiosum.
Figure S1B Ventral stricturotomy of the fossa navicularis and meatus.
Figure S1 Plane of dissection and ventral stricturotomy.
However, in the other 11 patients, who had been treated with transverse penile island flap and split glanuloplasty. Exposure was through a short transverse incision on the ventrum of the penis 0.5cm proximal to the coronal sulcus, & degloving of the ventral aspect deep to the dartos fascia. Ventral stricturotomy was carried out from the external meatus distally to the healthy penile urethra & glanular wings were created. Elevation of the transverse penile island flap was carried according to the length and caliber of the urethra needed as in Figure S2. A suitable silicone urethral catheter was inserted. The flap was rotated 90 degrees to be vertically oriented as in Figure S3A. Working from the proximal end, a submucosal suture with 5-0 Vicryl was taken to complete the urethral closure, another layer of dartous for augmentation of the suture, closure of the coronal incision and closure of the glanular wing with 5-0 Vicryl subcuticular suture. The incision at the coronal sulcus was approximated with a fine sub-cuticular suture. A suitable silicone urethral catheter was inserted for 3 weeks Figure S4.
In 4 patients the stricture was extended to the penile urethra and so we repaired them with Orandi flap. Ventral stricturotomy from the meatus to the healthy penile urethra. The lateral penile skin flap was marked on the lateral aspect of the incised urethra with a suitable length and width according to the urethral caliber that required care to preserve the pedicle of the lateral skin flap. The urethral edges were sutured to the flap on both sides distally up to the meatus with 6-0 Vicryl suture. Glanular wings were created and closed over the augmented urethra with 6-0 Vicryl suture. A suitable silicone urethral catheter was inserted for 3 weeks. In 3 patients, there was no sufficient penile skin as they had a history of repair of hypospadias many times so a buccal mucosa graft was the best choice. The penile skin was degloved until the healthy urethra. Ventral stricturotomy had been started from the meatus until the healthy urethra proximally. Buccal mucosa graft was harvested from the lower lip according to the urethral diameter that was needed. A suitable silicone catheter was inserted. The graft was sutured with 5-0 Vicryl suture to the urethral edge on one side starting proximally till the tip of the meatus and then the same for the other side. The graft was covered with a layer of dartous fascia to augment the suture line. Glanular wings were closed with 6-0 Vicryl suture subcuticular suture over the graft.
The last 3 patients with fossa navicularis stricture were proved by a biopsy to have LS. We had arranged to repair them in two stages. In the first stage, we excised the urethra completely till the healthy proximal segment with complete exposure of the glans and preparation of a well-vascularized bed as in Figure S5. Buccal mucosa was harvested from the lower lip according to the defect and a segment not more than 4cm in length and width of 1cm was folded to cover the entire defect. The graft was sutured with 6-0 Vicryl suture laterally to the skin edges on both sides till the tip of the meatus and proximally to the urethral meatus. The graft was meshed to prevent serous collection under the graft, and we had taken a tacking suture to fix the graft to the underlying tunica albuginea. A suitable silicone urethral catheter was inserted. The graft was fixed with gauze to prevent mobility. 2nd stage was after 6 months. U-shaped incision from the tip of the glans distally to around the urethral meatus proximally was carried. Lateral dissection was carried out subdermally with preservation of dartous pedicle and tubularization of the taken buccal graft with augmentation of the suture line with a second layer of dartous fascia using 6-0 Vicryl suture on a suitable silicone urethral catheter.
All patients were diagnosed with fossa navicularis stricture with or without penile urethral stricture. Their ages ranged from 8-60 years with a mean age of 35 years. In 3 patients, there was an associated subcoronal urethrocutaneous fistula after hypospadias repair, while another 3 patients had a scar from previous hypospadias repair. 9 patients had a history of Visual internal urethrotomy (VIU) and repeated dilatation with urethral sound in 8 patients. All patients had meatal stenosis and indurated distal part of the penile urethra in 7 patients. Manifestation of Lichen sclerosus (LS) was noticed in 3 patients as white patches on the glans & narrow depressed meatus.
Different etiologies of the stricture of our patients were listed in supplementary Table 1. The median follow-up time was 24 months. Cosmetic assessment of all patients was carried out using Hypospadias Objective Scoring Evaluation (HOSE score) Figure S6. The postoperative surgical outcomes were listed in the Table 1. Functional evaluation was done for all cases using flow rate and ascending urethrocystogram. Mean flow rate after the repair was 15.3 ml/sec. Follow-up with urethrogram had revealed patent urethra with no stricture or diverticular formation in 39 patients Figure S7.
|
Procedure |
Number of cases |
HOSE score (mean) |
Successful cases |
Failed cases |
Causes of failure |
|
Transverse penile island flap with glans cap technique |
22 |
15 |
22 |
0 |
0 |
|
Transverse penile island flap with wing glanuloplasty. |
11 |
13 |
9 |
2 |
(1) glanular disruption |
|
(1) fistula |
|||||
|
Orandi flap. |
4 |
15 |
4 |
0 |
0 |
|
Buccal graft. |
3 |
14 |
2 |
1 |
fistula |
|
2 stages repair buccal graft in lichen sclerosus |
3 |
14 |
2 |
1 |
Recurrent stricture |
Table 1 Results after each surgical procedure
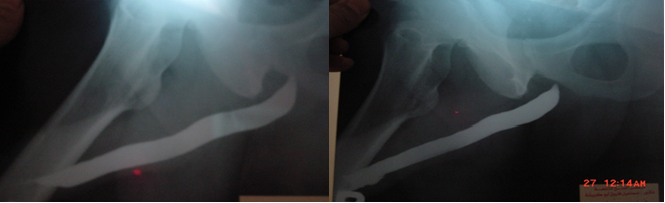
Figure S7 Ascending urethrocystogram showing fossa navicular stricture in image- preoperative (a) and normal postoperative normal urethral lumen in image- postoperative (b).
Two patients from those who were managed with transverse penile island flap and glanuloplasty developed complications; one of them had developed glanular disruption after 1 week and repaired after 3 months with simple tubularization and the other had developed coronal fistula after 2 weeks managed by simple closure after 3 months and completed their duration of follow up with no further complications. One patient from those who were managed with buccal mucosa developed an infection and subcoronal fistula, closed after 3 months with simple closure, and completed his follow-up duration with no further complications. One patient from those who had been repaired in two stages with buccal mucosa graft; had developed recurrent stricture after three months.
Urethral stricture disease is relatively common and is associated with significant debilitating outcomes affecting health-related quality of life.5 Distal urethral strictures confined to the fossa navicularis represent 18% of all anterior urethral strictures.6 These strictures can result from trauma, instrumentation, prior hypospadias surgery, and lichen sclerosis, which is the most common cause accounting for 12–42% of cases.7,8 Fossa navicularis stricture differs regarding the etiology and the treatment from any part of anterior urethral stricture. For reconstruction of fossa navicularis stricture, the patient should regain urethral patency and preserve cosmesis.9 In the study, different causes underlying the pathogenesis of the disease. The most common cause was previous transurethral endoscopic operations with the urethral catheter (iatrogenic, 45.6 %), then post hypospadias repair (18.6 %), previous prolonged catheterization (9.7 %), inflammatory process (LS) (7.3 %). These findings were replicated in a study conducted by Prakash Babu et al. who found that 40 % of patients with fossa navicularis stricture had prior instrumentation in the form of Transurethral resection of prostate (TURP) then prolonged catheterization representing 16 % of the patients.10
There are many techniques for the repair of fossa navicularis stricture. The choice of the technique depends on the length of stricture; the urethral meatus either normal or stenosed, the site of the meatus either at its normal site or not, the previous history of urethroplasty, dilatation, VIU, and the availability of the penile skin. Paramount to the success of any of the procedures is the careful selection of non-diseased tissue for substitution. If the penile skin is healthy, the preferred urethral substitute is the fasciocutaneous ventral transverse island flap. The inherent characteristics of this versatile flap (i.e., well-vascularized predictable pedicle, nonhair bearing, negligible contraction) provide for an excellent time-tested glandular urethral substitute. However, in case of penile skin inflammation or scarring (e.g., LS), extragenital tissue transfer techniques should be advocated.11 Many techniques have been used for the repair of fossa navicularis stricture starting from the minimally invasive to the advanced tissue transfer techniques. Y-V advancement flap can be used for a short segment, but meatal disfigurement is a common complication. Cohney described a technique for the repair of fossa navicularis stricture using a ventral penile skin flap, however, its limitation is the short length of the flap and increasing degree of ventral curvature.12
Jordan had described the use of a transverse ventral penile island flap that is now a universal technique for the repair of fossa navicularis and meatal strictures. As regards the glanular reconstruction, Jordan used the glans cap technique with a transverse penile island flap to preserve the glanular shape and cosmoses.3 McAninch used also a transverse ventral penile island flap but with split glanuloplasty for the repair of fossa navicularis stricture.13 In this study, 33 patients were repaired with transverse penile island flap as they had ample ventral non-hairy penile skin. 22 patients of them were treated with transverse penile island flap with glans cap technique as these patients have no scarring and so the plane of dissection was easy. Glans cap technique does not cause any change in glanular configuration and no residual scarring. Those cases that were repaired with this technique had no complications. Noel A et al. reported no complications with the use of the transverse penile island flap with the glans cap technique in the reconstruction of fossa navicularis stricture.13
In the remaining 11 patients, the transverse penile island flap was used with splitting glanuloplasty as marked scarring from previous operations (VIU and previous hypospadias repair); coronal fistula was developed in one case that was repaired after 3 months, and another one developed an infection and glanular disruption which was repaired after 3 months with simple tubularization 4 patients had a proximal extension of the stricture 1.5 cm-2 cm of the penile urethra, so, the Orandi flap was created to repair these cases as the ventral transverse island penile flap was not sufficient to augment that segment with no reported complications.14 El kassaby and colleagues used buccal mucosa patch graft for repair of anterior urethral stricture, and they recommended it because buccal mucosa has many advantages over any graft, being readily available, easy to harvest, no cosmetic defects, has thick epithelium, high elastin fiber, vascularized lamina propria, and less contraction. The rich blood supply of the glans makes it an ideal graft bed. Buccal mucosa can be used if penile skin is not available or diseased.15 In our study, 3 patients were treated with buccal mucosa graft as ventral onlay graft to augment the ventrum of the strictured fossa navicularis and distal part of the penile urethra as those patients had no sufficient penile skin due to failed previous hypospadias. 1 patient developed a coronal urethrocutaneous fistula due to an infection that was repaired after 3 months.
Fichtner and colleagues also used the buccal mucosa as onlay to augment the ventral aspect of the anterior urethra with a success rate of 88.2% & recurrent stricture rate of 11.8% at the proximal anastomotic site of the graft to the native urethra.16 Similar studies reported favorable outcomes using buccal mucosa graft in stricture urethra repair.17–19 The last 3 patients diagnosed as LS were treated in two stages, in the first stage the whole segment of fossa navicularis was completely excised, meshed buccal mucosa graft was applied on the bed and simple tubularization was carried out 3 months later. one patient of them developed restricture proximally at the anastomotic site which was corrected after 3 months with resection and anastomosis as it was short segment stricture (0.5cm). These findings were comparable to the study conducted by Deepak Dubey et al. who found that two-stage repair for LS patients with stricture urethra showed satisfactory outcomes but they are associated with a relatively higher revision rate.20 The limitations of our study are the relatively small sample size and its retrospective nature.
Fossa navicularis stricture is a special entity as regards anatomy, etiology, diagnosis, and treatment. The techniques of repair of fossa navicularis stricture depend on the length of stricture, availability of penile skin, and penile skin disease such as Lichen sclerosus. Repair of fossa navicularis stricture is challenging. Repair of fossa navicularis stricture should be in either one stage or two stages. The use of a ventral transverse penile island flap is the ideal technique with the glans cap technique as it preserves the glanular shape and configuration and if penile skin is not available or the length of stricture cannot be compensated by the transverse penile island flap or there is Lichen sclerosus so, another tissue transfer technique is a good alternative. The appropriate technique results in a successful functional and cosmetic outcome.
Informed consent was obtained from all individuals included in this study regarding their participation and publishing their data.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. This study was approved by the Institutional Review Board of Medical Research Ethical Committee – Faculty of Medicine-Sohag University (IRB00013006).
The authors have no relevant financial or non-financial interests to disclose.
No funding was received to assist with the preparation of this manuscript.
Zaki M. El Dahshoury: Project development, Data collection, Manuscript writing.
Hanna P.: Manuscript writing/editing, Data collection, Data analysis.

©2023 El, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.