eISSN: 2378-3176


Case Report Volume 2 Issue 5
Department of Urology, Gauhati Medical College Hospital, India
Correspondence: Sasanka K Barua, Department of Urology, Gauhati Medical College Hospital, Guwahati, India, Tel 91 9864096583
Received: October 24, 2015 | Published: November 23, 2015
Citation: Barua SK, Gupta N, Rajeev TP, et al. A typical presentation of vesical paraganglioma. Urol Nephrol Open Access J. 2015;2(5):143-146. DOI: 10.15406/unoaj.2015.02.00053
Paragangliomas are extra adrenal pheochromocytoma arising from the chromaffin tissue of sympathetic nervous system. It accounts for 15% of all the pheochromocytomas. Paraganglioma of urinary bladder is an extremely rare entity and difficult to diagnose in absence of typical symptoms of catecholamines excess. They usually have typical symptoms of hypertensive episodes specifically during voiding or sexual activity. Calcification within paraganglioma is even rare entity and often mimics vesical calculus. Partial cystectomy remains the treatment of choice and confirmation of diagnosis requires immunohistochemical staining. Here we report a case of calcified paraganglioma of urinary bladder with atypical presentation and review of pertinent literature.
Keywords: urinary bladder, paraganglioma, metanephrines, partial cystectomy
TURBT, transurethral resection of bladder tumor; HR, heart rate; RCC, renal cell carcinoma
Paragangliomas of urinary bladder is an extremely rare tumor which arises from chromaffin tissue of sympathetic nervous system. The occurrence of urinary bladder paraganglioma was first reported by Zimmerman et al.1 It accounts for less than 0.06% of total urinary bladder tumors and less than 1% of all pheochromocytomas.2 They usually present with the typical tetrad symptoms like micturitional syncope, sweating, palpitation and hematuria.3 However in the extremely rare circumstances they may be non functional with absence of the typical signs and symptoms of catecholamine excess.4 In rare instances, they may be associated with extensive calcification mimicking vesicolithiasis making the diagnosis more difficult.5 However post extirpation histological examination with immunochemistry aids in achieving proper and correct diagnosis.6
Although these neoplasms are considered as benign they may exhibit typical characteristics of local invasion in extraordinary situations.7 In 10%-15% of the cases these tumors may be malignant, characterized by local invasion, lymph node involvement or distant metastasis.8 We here-in describe a case of calcified paraganglioma of urinary bladder with atypical presentation in a 45years old female which was successfully treated by open partial cystectomy.
A 45years old non hypertensive married female was referred to us with the complaints of dysuria and vague lower abdominal discomfort since last 4months and was diagnosed elsewhere as a case of vesical calculus based on presence of a radio-opaque shadow in pelvis on plain radiograph (Figure 1A.xray pelvis). Her general and systemic examination were unremarkable and all the laboratory parameters were within normal limits. Urine routine and microscopy was within normal limits and urine culture was sterile. Ultrasonography of abdomen revealed a calcified heteroechoic space occupying lesion of approximately 4x4cms in right posterolateral wall of urinary bladder (Figure 1B. USG). Subsequent contrast enhanced CT revealed 4.5x4.7cms hyper vascular enhancing mass lesion with surface calcification in right posterolateral wall of urinary bladder. There was no evidence of pelvic lymphadenopathy on imaging studies (Figure 1C. CECT). Urine cytology for malignant cells was negative.
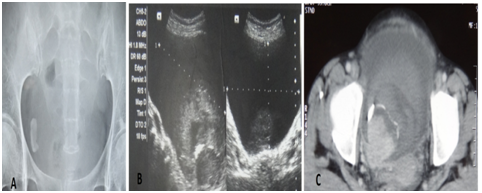
Figure 1 Figure 1A. X ray pelvis showing radio-opacity in right hemipelvis. Figure 1B. USG showing urinary bladder mass with calcification. Figure 1C. CECT showing urinary bladder mass with surface calcification and enhancement.
Patient was planned for trans urethral resection of bladder tumor (TURBT). During pre-TURBT cystoscopy, moderate cystodistension with irrigant resulted in sudden and severe hypertensive crisis with blood pressure rising to 240/130 mm Hg and a heart rate (HR) upto 160beats/min. The urinary bladder was evacuated immediately and procedure was abandoned which resulted into normalization of BP and heart rate within a minute. This adverse intraoperative event led us to the suspicion of urinary bladder paraganglioma. On subsequent investigation, 24hour urinary metanephrines, and serum cortisol were found to be within normal range (24hour urinary metanephrines–295micrograms/24hrs, serum cortisol-13.95micrograms/dl). When retrospectively eliciting the history, there was no history of headache, palpitation, sweating, flushing or any other symptoms of catecholamine excess in past.
Patient was started on low dose alpha blocker and was taken for open partial cystectomy. During the resection, patient had an episode of intraoperative hypertension which was well controlled and tumor was successfully excised (Figure 2). There was no intraoperative or perioperative adverse event. Histopathological examination of the specimen revealed it to be a urinary bladder paraganglioma, confirmed by immunohistochemistry which was positive for synaptophysin, chromogranin and S-100 protein and negative for CK7 and CK20 (Figure 3). Patient recovered well in the post operative period and was discharged on fourth post-operative day. Patient is on regular follow up since last 8months without any symptoms.
First described by Zimmerman in 1953, urinary bladder paragangliomas are an extremely rare entity with varied presentation.1 Paraganglioma of urinary bladder constitute less than 1% of pheochromocytomas and 0.06% of all urinary bladder tumors. Morphologically they mimic transitional cell carcinoma of urinary bladder which makes the diagnosis more difficult. However presence of typical tetrad symptoms of headache and micturition syncope, sweating, palpitation and hematuria in the presence of a urinary bladder mass should raise the suspicion of urinary bladder paraganglioma,3 particularly when such symptoms are precipitated by micturition, defecation or ejaculation.5
In rare instances paraganglioma may be non-functional together with the absence of symptoms of catecholamine excess as seen in our case. Sometimes these tumors undergo extensive calcification and may mimic vesicolithiasis similar to present case. Vahidi K. et al.,9 has described characteristic imaging signs for urinary bladder paraganglioma which are presence of nodular mass with homogeneous or heterogeneous density/signal with well-defined borders with soft tissue attenuation on a plain CT scan and slightly higher signal intensity than that of the gluteal muscle on pre-enhanced T1-weighted imaging (T1WI), and hyper intensity compared to gluteal muscle on T2WI. They also observed that paragangliomas are extremely vascular and exhibit greater enhancement than that of urinary bladder wall. Jian-Hua Deng et al.,3 have highlighted that octreotide scintigraphy has a higher specificity while MIBG has a higher sensitivity in diagnosing functional urinary bladder paraganglioma.
These tumors are usually well circumscribed and nodular, mostly located to the lateral wall of urinary bladder and amenable to partial cystectomy which can be done either by open or laparoscopic approach.10 Usually large multiple polypoidal lesions with broad base are likely to be malignant while small single, round or ovoid tumors are more likely to be benign.2 Transurethral resection should be avoided as it may lead to extensive hemorrhage because of the rich vascularity and may simultaneously precipitate hypertensive crisis which may lead to considerable morbidity or even death.5 Since it originates from the intramural portion of urinary bladder, routine TURBT may not be able to excise the tumor entirely.2 Moreover high recurrence rates have been observed in those who underwent TURBT for urinary bladder paraganglioma. In the presence of radiologically detectable pelvic lymphadenopathy, bilateral pelvic lymph node dissection is advocated to achieve optimal cure.7 However deep local invasion with lymph node involvement and metastasis warrants radical cystectomy and urinary diversion.11
The typical histological characteristic of paraganglioma is described as “zellballen” pattern characterized by large tumor cells extensive stromal vascularity, granular cytoplasm and low nuclear to cytoplasmic ratio.12 The histological examination of our case showed large tumor cells with smaller nuclei, consistent with the findings of paraganglioma. The tumor cells usually grow in nested pattern but rarely diffuse pattern of cellular arrangement may be seen. Accurate cytological analysis is of paramount importance to establish a diagnosis of vesical paraganglioma since there may be histological overlap between urothelial carcinoma, particularly nested variant of transitional cell carcinoma. In a retrospective analysis Menon et al.,6 have identified certain variable histological features of vesical paraganglioma which lead to misdiagnosis like focal sheet-like pattern, ribbon-like growth pattern, and focal necrosis, presence of intra-cytoplasmic brownish melanin pigment and muscularis propria invasion. The authors further opine that frequent involvement of detrusor muscle, associated significant post TURBT cautery artifacts can also lead to misdiagnosis. Many a time’s malignant melanoma, metastatic renal cell carcinoma (RCC), prostate carcinoma, carcinoid tumors, and granular cell tumor morphologically mimic as urinary bladder paraganglioma.
Immunohistochemistry plays a pivotal role in establishing the diagnosis of urinary bladder paraganglioma particularly in case of conflicting histological features. Kovacs K et al.,13 have highlighted that chromogranin, synaptophysin and NSE can help to identify neural tissue and neuroendocrine cells, and paragangliomas having their origin from chromaffin tissue are usually positive for chromogranin and synaptophysin. The immunohistochemistry of our case was positive for chromogranin, synaptophysin and S-100 protein establishing the diagnosis of vesical paraganglioma. Deng et al.2 has observed that advanced stage (>T3), multifocal tumors and tumors with Chromogranin A (CgA) expression were high risk factors of recurrence, metastasis, and even death from disease.3 In view of this, yearly follow up with endoscopy and imaging is advocated for early detection of recurrence and metastasis.
Urinary bladder paragangliomas are rare tumors of chromaffin tissue with varied presentation. Apart from characteristic symptoms of catecholamine excess, they may be non functional with absence of typical symptoms. In rare instances extensive calcification over vesical paraganglioma may mimic vesicolithiasis. Because of histological overlap with many other urinary bladder tumors immunohistochemistry plays a pivotal role in achieving the diagnosis. These tumors are usually treated by partial cystectomy either by open or laparoscopic approach, although bilateral pelvic lymphadenectomy is advocated in presence of radiologically detected lymphadenopathy. As far as possible TURBT is avoided to prevent intraoperative catastrophy and incomplete resection of tumor. In view of possible recurrence or metastasis, patient should be followed up yearly lifelong.
None.
The author declares no conflict of interest.

©2015 Barua, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.