eISSN: 2378-3176


Opinion Volume 4 Issue 5
Department of Nephrology & Transplantation, Urology & Nephrology Center, Egypt
Correspondence:
Received: April 19, 2017 | Published: April 24, 2017
Citation: Elsaftawy MM, Akl A. Approach to post kidney transplantation anemia. Urol Nephrol Open Access J. 2017;4(5):136. DOI: 10.15406/unoaj.2017.04.00140
Anemia; Kidney transplantation; Anemia post-transplantation; CKD; Immunosuppression
Post-Transplant Anemia (PTA) is an important issue in kidney transplant recipients. Anemia is a major player in the non-immunological causes of graft dysfunction. The precipitating causes of anemia post transplantation include immunosuppressive drugs, iron deficiency, infections, older donor age, rejection episodes, and an increased inflammatory state [1]. In case of one kidney transplantation, the transplanted kidney function seems to be only partially restored, resulting in an incomplete correction of anemia. This post-transplantation anemia (PTA) likely contributes to chronic ischemic injuries and eventually graft loss on the long term [2].
When to consider post transplantation anemia?
Evaluation of PTA should be undertaken when hemoglobin fails to normalize by 3 months after transplantation. Evaluation of PTA should take place when the hemoglobin falls to less than 11 g/dl in pre-menopausal females or to less than 12 g/dl in males and postmenopausal females [3]. The definition of anemia is established by the World Health Organization and was subsequently adopted by the American Society of Transplantation, which defines anemia as hemoglobin concentration <12 g/dl in women and <13 g/dl in men [4].
Transplant recipients differ from other patients with chronic kidney disease because they bear the additional burden of therapy with immunosuppressive drugs that may directly exacerbate anemia. Indeed, the wide variation in the reported prevalence of PTA likely reflects differences in the use of anti-proliferative immunosuppressive agents (e.g., azathioprine, mycophenolate mofetil, and sirolimus) that may directly but variably inhibit erythropoiesis [5]. Other factors commonly associated with PTA include recipient age and female gender, donor age, and the use of angiotensin converting-enzyme inhibitors or angiotensin receptor blockers, the latter likely related to the influence of these drugs on angiotensin II type I receptors that are increased on erythroid progenitors in patients with PTA [6]. More recent data have suggested strong associations of anemia with graft failure and mortality [7]. We recommend the following diagram to guide PTA management (Figure 1).
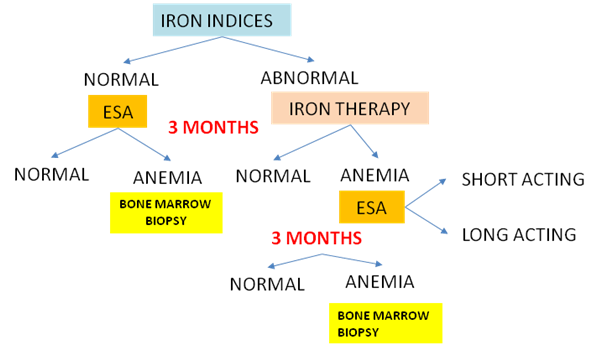
Figure 1: POST TRANSPLANTATION > 3 MONTHS, IF HEMOGLOBIN <13 g/Dl in males and post menopausal women and <12 g/dL in pre-menopausal women.
PTA correction with erythropoietin hormone in transplant recipients with moderate renal dysfunction slows the decline in glomerular filtration rate, reduces the incidence of end stage kidney disease, and improves quality of life (Qol) without increasing the risk of cardiovascular events. This Study provides evidence that kidney disease in transplant recipients constitutes a particular entity and that the results from nephron protection studies conducted in CKD patients should not be directly extrapolated to transplant recipients. Additional studies should be carried out to confirm whether complete correction of anemia in transplant recipients might impact patient survival and establish the optimal hemoglobin target level in transplant recipients [8].

©2017 Elsaftawy, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.