eISSN: 2378-3176


Case Report Volume 9 Issue 2
1Internal Medicine Department, Dr Soliman Fakeeh Hospital, Jeddah, KSA
2Intensive Care Department, Dr Soliman Fakeeh Hospital, Jeddah, KSA
3Fakeeh College of medical sciences, Jeddah, KSA
4Internal Medicine Department, King Fahad Hospital, Jeddah, KSA
5Urology & Nephrology center, Mansoura University, Mansoura, Egypt
Correspondence: Ahmed Akl MD, FACP, FASN, DR. Soliman Fakeeh hospital, Jeddah, KSA, Urology & Nephrology center, Mansoura University, Egypt
Received: March 21, 2021 | Published: April 16, 2021
Citation: Al-Khatib NR, Al AA, Al-Shobaki R, et al. A successful management of acute cholemic nephropathy secondary to acute liver abscess and pylephlebitis associated severe sepsis by ERCP, combined CVVHDF and stepwise hemodialysis. Urol Nephrol Open Access J. 2021;9(2):43-45. DOI: 10.15406/ unoaj.2021.09.00306
Cholemic nephrosis or yellow kidneys, is a rare condition and can be associated with acute kidney injury secondary to various etiologies. We are reporting a difficult case presented with fatal severe sepsis associated with hepatic, pancreatic and renal injury secondary to impacted biliary stone at the ampulla of vater and complicated by infection. With proper management and early drainage of biliary system and continuous renal replacement therapy the patient survived. The early recognition and interference leads to reversal of symptoms and improvement of renal and patient survival.
Keywords: acute hepatitis, cholestatic hepatitis, septic shock, acute kidney injury, renal replacement therapy, ascending cholangitis
Cholestatic liver disease affecting kidney function by different mechanisms and is described by different names: bile cast nephropathy or cholemic nephrosis, biliary nephrosis, jaundice-related nephropathy or yellow kidneys.1 It carry a various hazards on kidney function ranging from hemodynamic changes accounting for pre-renal hypo-perfusion, ischemic injury and direct tubular toxicity induced by hyperbilirubinemia and bile casts.1,2 Its prevalence is increasing with more reporting of identified cases compared to previously documented.3–8 The early recognition and interference leads to reversal of symptoms and improvement of renal and patient survival. Choledocholithiasis, is associated with acute kidney injury is accompanied by typical histological changes, including tubular epithelial injury, together with intraluminal bile cast formation.9,10
Biliary tract disease is the most common condition associated with liver abscess.11 This includes infection (cholangitis) that may occur secondary to choledocholithiasis, biliary stricture, or malignancy.12
A 59-year-old female with multiple co-morbidities including ischemic heart disease with coronary artery bypass grafting in 2016, diabetes mellitus, hypertension. She presented with fever, abdominal pain related to chronic calcular cholecystitis and poor oral intake referred to examined by general surgery and they recommend to start antibiotics course and to be re-assessed again in a week time. After four days, patient came to the emergency department with severe septic shock, blood pressure as low as 80/40 mmHg refractory to fluids resuscitation. Radiological investigations revealed severe ascending cholangitis, impacted biliary stone at level of ampulla of vater, complicated by liver abscess and anuric acute kidney injury with refractory hyperkalemia and metabolic acidosis requiring urgent renal replacement therapy. Patient was transferred immediately to intensive care unit. In view of dilated biliary radicles with signs of biliary stone impaction, urgent endoscopic retrograde cholangiopancreatography (ERCP) was performed, with stent insertion and pulling out of a large pigmented stone and drainage of biliary muddy fluid (Figure 1). Immediate continuous renal replacement therapy in the form of continuous venovenous hemodiafiltration (CVVHDF) was initiated to correct the metabolic and electrolytes disturbances in order to save the patient life.

A) Pigmented biliary stone obstructing Ampula of Vater.
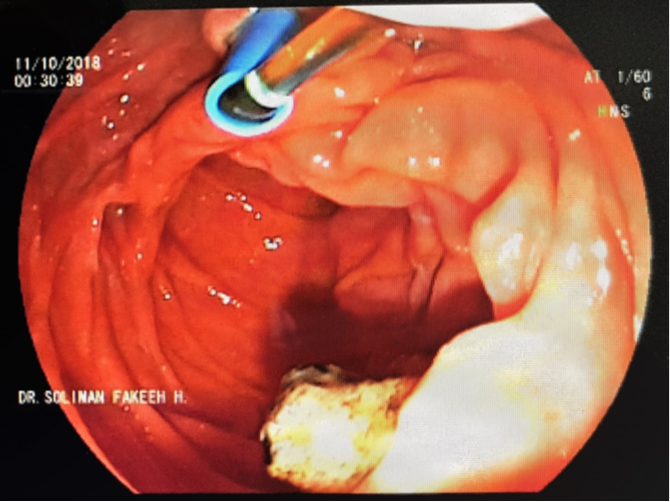
B) Stent of the common bile duct for drainage.
Figure 1 ERCP and dislodge of impacted biliary stone at ampulla of Vater.
Abdominal ultrasound imaging revealed a constant interval of the liver abscess and postal vein thrombosis (pylephlebitis). Pylephlebitis and severe cholangitis were managed by a total of 4 weeks of intravenous antibiotics and therapeutic heparin infusion. Aspiration of the liver abscess was done and culture revealed negative growth. Repeated abdominal us showed improved pylephlebitis and patent portal vein. The patient was evaluated by general surgery, with their recommendation being to postpone the cholecystectomy till after resolution of the liver abscess. She was discharged home after 4 weeks to complete 6 weeks to 3 months of antibiotics or until complete resolution of the abscess at outpatient follow up basis. Regarding the state of anuria in setting of acute kidney injury, the patient had required daily continuous renal replacement therapy in the intensive care unit for 1 week. Thereafter, her hemodynamic improved and shifted to slow inefficient dialysis daily (SLEDD). Clinically improved with improvement of her urine output (Figure 2) the need for hemodialysis declined to 3 times per week, then twice per week, till reaching a requirement of once per week. The patient’s urine output improved to around 2L/day in the few days prior to discharge, with her last creatinine clearance estimated to be 10 ml/min. She was discharged on furosemide twice per oral daily and bicarbonate tablets, as well as oral anti-hypertensive medications. At the outpatient clinic, her kidney function improved with serum creatinine reaching basal level 1.8 mg/dl, eGFR (EPI) 30 ml/min and normal electrolytes with no hemodialysis. Her abdominal us shows normal biliary radicles and patent portal vein.
The mechanisms of kidney injury described with bile cast nephropathy is similar to to the injury caused by myeloma or myoglobin casts. Bile casts may lead to oxidative stress and trigger the inflammasome signaling cascade, leading to interstitial inflammation.13 Definitive diagnosis of bile cast nephropathy is by renal biopsy, as there is no validated non-invasive specific diagnostic test and it is frequently diagnosed at time of autopsy or on kidney biopsy.13 Histological land marks appears in distal tubules in the form of dilated tubules and obstruction by intraluminal casts. The bile casts can be confirmed by periodic-acid Schiff (PAS) stains showing red to dark red colored casts15 or Masson trichrome using aniline green, bile casts show a green color.16 Besides bile casts, kidney histology may show varying degrees of acute tubular injury characterized by tubular epithelial cells with attenuated cytoplasm or loss of proximal tubular brush borders or regenerative changes and interstitial inflammation.15
Also, the presence of mononuclear inflammatory cells in the vasa recta has been previously reported15 Given the current lack of non-invasive methods to diagnose bile cast nephropathy and that kidney histology is the single established diagnostic test, conventional kidney biopsy is relatively risky in patients with liver disease, especially with impaired blood coagulation. Additionally, distal nephron segments, which have been reported to be of specific diagnostic importance for establishing the diagnosis of CN, are probably not reached by conventional kidney biopsy, since this also carries a significant risk for bleeding. Whether a trans-jugular approach may represent a suitable and safe alternative to significantly reduce such risks in this group of patients as was shown.17 In our case we could not do renal biopsy because of the severe sepsis and coagulopathy status. Due to the rarity of bile cast nephropathy, there are currently no established treatment guidelines. Interventions to reduce bilirubin burden, such as relief of biliary obstruction via ERCP with stent placement and hemodialysis, have been attempted to improve outcomes. While this appears to be an effective strategy early in the disease course, its efficacy in established disease is uncertain.18–21 Plasmapheresis may additionally be beneficial.22
In conclusion, early diagnosis of obstructive cholangitis and drainage which followed by hemodiafiltration improved patient condition and enhanced recovery from severe sepsis, hyperbilirubinemia and bile salt nephropathy.
We would like to thank our ICU, RDU, Inpatient nurses teams, our residents and all other hospital stuff for their hard work taking care of our patient.
The author declares there is no conflict of interest.

©2021 Al-Khatib, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.