eISSN: 2378-3176


The American Urological Association guidelines now explicitly place partial nephrectomy as the standard of care for T1a renal tumors (<4cm). The reduction of estimated eGFR increases the risk of death, cardiovascular events, and hospitalization. Therefore, partial nephrectomy may prevent these comorbidities by preserving renal function and eGFR. Partial nephrectomy without clamping in a solitary kidney was associated with superior preservation of late eGFR. Our main goal is to present our technique with a robotic assisted Laparoscopic partial nephrectomy without ischemia time in a solitary kidney.
Pt is a 63yo obese male who had a history of a left nephrectomy due to renal trauma many years ago. He presented to our practice with an incidental finding on a Ct-scan of the abdomen/pelvis, these finding showed a right renal mass, measuring 5.2cm, upper pole, posterior, enhancing, close to the collecting system, no renal vein or inferior vena cava (IVC) thrombus, 1 artery, RENAL nephometry score 5p, eGFR 60.0 and Creatinine =1.1mg/dl and BMI=36. He Underwent an uneventful Right Robotic Assisted Laparoscopic Partial Nephrectomy (RALPN) (Video), No ischemia time, the right renal artery was identified and dissected but was not clamped. Estimated blood loss 500cc, fluids during the surgery 2500 of Lactated ringer, and 1 unit of packed red blood cells, Surgery time 3 hrs and 30 minutes, length of stay in the hospital was 3 days, no post-operative complication.
RALPN can increase the number of PN offered to patients, and may enable progression to more challenging cases like T1b (4-7cm) and solitary kidney with renal a mass. In solitary kidneys there are some finding suggesting that renovascular clamping is the only statistically significant determinant of postoperative renal dysfunction. Long-term follow up and prospective randomized studies may need to include ischemia vs no ischemia time in their PN group, especially in solitary kidney.
Keywords: small renal mass, partial nephrectomy, laparoscopic partial nephrectomy, robotic assisted laparoscopic partial nephrectomy, kidney cancer, solitary kidney, no ischemia time
eGFR, estimated glomerular filtration rate; RALPN, robotic assisted laparoscopic partial nephrectomy; PN, partial nephrectomy; RN, radical nephrectomy; EBL, estimated blood loss; IVC, inferior vena cava; ccRCC, clear cell renal cell carcinoma; ECOG-PS, eastern cooperative oncology group performance status; CT, computed tomography
Partial nephrectomy has evolved since 1991 when Dr. Novick published his outcome in the first 14 patients.1 The reduction of eGFR increases the risk of death, cardiovascular events, and hospitalization.2 Recent publications comparing partial nephrectomy with and without clamping in solitary kidneys suggests that renovascular clamping is the only statistically significant determinant of postoperative renal dysfunction.3,4 In patients with 2 kidneys ischemia time and parenchymal loss have been important factors to preserve eGFR.5 Here we described our surgical steps of a RALPN without ischemia time in a solitary kidney.
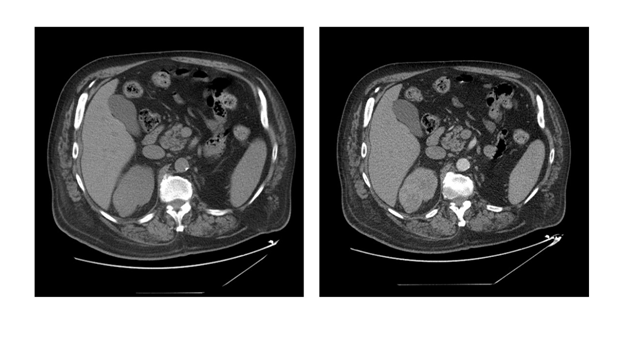
Pt is a 63years obese male who had history of a left nephrectomy due to renal trauma manyyears ago. He presented to our practice with an incidental finding on a Ct-scan abdomen/pelvis: these finding showed a right renal mass, measuring 5.2cm, upper pole, posterior, enhancing, close to the collecting system, no renal vein or inferior vena cava (IVC) thrombus, 1 artery, RENAL nephometry score 5p (Figure 1) (Figure 2). He had IVC filter placed and is taking Coumadin for previous pulmonary embolisms. He was smoker for 40years and he stopped about 10years ago. His ECOG-PS is 0. He denies coughing, chest or bone pain. Patient has a family history of diabetes, heart disease and stroke. His weight 255Lbs (115kgs), blood pressure 110/70mmHg, Temp 97 F, Height 5’10’’ (178cm), BMI= 36. Urine Analysis was negative for hematuria or microscopic hematuria, Chest X ray= negative for lung metastasis. Creatinine 1.1mg/dl and eGFR 60.0. ALk Phos 98U/L, Ca 9.5mg/dl, Albumin 3.6g/dl. Hemoglobin 15.0g/dl, Hematocrit 45.2%, Platelet count 221thou/cm, WBC 9.2 thou/cm, all values were within normal range. His stage was T1bNoMo, Right renal mass, suspicious for RCC. We offered him Right RALPN without ischemia time.

He Underwent an uneventful Right RALPN (Video), No ischemia time, the right renal artery was identified and dissected but was not clamped. Estimated blood loss 500cc, fluids during the surgery 2500 of Lactated ringer, and 1 unit of packed red blood cells, Surgery time 3 hrs and 30 minutes, length of stay in the hospital was 3 days, no post-operative complication. Patient was 24hrs in the intensive care units, there he received an additional 1 unit of PRBC his Hemoglobin/Hematocrits was 7.2g/dl/26%, vital signs were stable and he was transferred to the floor, his bladder catheter was removed on postoperative day 2 and JP drain was removed 24 hrs later. He was tolerating a regular diet at 24hr after surgery and pain was controlled by mouth medication. At the time of discharge his laboratories were: Creatinine 1.5mg/dl and eGFR 49.850. Ca 8.8mg/dl. Hemoglobin 9.5g/dl, Hematocrit 29%, Platelet count 189 thou/cmm, WBC 6.2thou/cmm. He was ambulating and had good bowel function. At 4months after his surgery his creatinine was 1.3ml/dl and eGFR 55 similar to his pre-op values. Pathology report was consistent with moderately differentiated ccRCC. There is no evidence of invasion through the capsule into the surrounding fat and uninvolved renal parenchyma is noted suggesting complete excision. No tumor necrosis, final Stage T1bNoMo.
The American Urological Association guidelines now explicitly place partial nephrectomy as the standard of care for T1a renal tumors (<4cm) and as an alternative option for T1b tumors (4-7cm).6 By 2007, 13.5% of newly diagnosed renal tumors measured <2 cm, 37% <3 cm and close to 60% <4 cm. This trend is a clear stage migration favoring stage I tumors and a significant decrease in tumor size even within the stage I group.7,8
With the rapid uptake of minimally invasive technology by the urological community, laparoscopic partial nephrectomy and, more recently, robot-assisted laparoscopic partial nephrectomy have emerged as viable alternatives to open partial nephrectomy for the management of suspected renal malignancy. Among its potential advantages, robotic technology offers high definition 3-dimensional visualization, a wide range of wristed instrument motion and scaling of surgeon movements. RALPN appears to have a shorter learning curve than laparoscopic PN and, as such, may facilitate and promote the use of minimally invasive nephron sparing surgery.9
Radical nephrectomy was associated with an increased risk of overall mortality (HR 1.38, p<0.01) and greater number of cardiovascular events after surgery (p<0.05).10 A recent publication had a controversial finding about RN vs PN, where both methods provide excellent oncologic results. In the intention to treat population, PN seems to be significantly less effective than RN in terms of overall survival.11 In another publication 31,728 patients and 51 studies were analyzed comparing PN vs RN. Partial nephrectomy has 19% reduction in all causes of mortality, 29% reduction in cancer specific mortality, 61% reduction in CKD.12
Recent publications comparing a partial nephrectomy with and without clamping in solitary kidneys suggests that renovascular clamping is the only statistically significant determinant of postoperative renal dysfunction. Studies comparing a partial nephrectomy with and without clamping demonstrate that ischemia is associated with a risk of acute renal failure, advanced CKD, and renal replacement therapy. Oncologic outcomes and complications in partial nephrectomy without clamping are similar to those with clamping.3,4
Functional volume preservation after a partial nephrectomy is a primary determinant of kidney function.5 R.E.N.A.L. and centrality index nephrometry scores were associated with changes in the percent functional volume preservation and the perioperative functional decrease. Tumors classified as highly complex, with a centrality index score of 1.5 or less and a R.E.N.A.L. score of 10 or greater, were associated with an average 28% to 30% functional parenchymal volume loss of operated kidneys. A mean 8% difference in percent functional volume preservation was observed among low, intermediate and high tumor complexity categories for R.E.N.A.L. and centrality index scores.5 Therefore, complex renal masses may have a decrease of renal function after RALPN.
RALPN can increases the number of PN offered to patients, and may enable progression to more challenging cases like T1b and/or solitary kidney with a renal mass. Minimally invasive surgery may offer a faster recovery and no-ischemia time or minimal ischemia time <25min are equally effective preserving renal function and eGFR, in patients with 2 kidneys. In solitary kidneys there are some finding suggesting that renovascular clamping is the only statistically significant determinant of postoperative renal dysfunction. The main goals of any approach should be remove cancer, preserve renal function with minimal complications. RALPN without ischemia time on T1b Renal Mass, are challenging cases and EBL can increase as compared to T1b with arterial clamping, so it is recommended to advice the patient about the possibility of transfusion and discuss it with the anesthesia team before surgery; however the oncologic outcomes and renal function are preserved maintaining the minimally invasive approach. Long-term follow up and prospective randomized studies may need to include ischemia vs no ischemia time in their PN group, especially in a solitary kidney.
None.
The author declares no conflict of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.