eISSN: 2577-8285


Research Article Volume 3 Issue 1
1Department of Kinesiology, North Carolina A&T State University, Greensboro, NC, USA
2Department of Kinesiology, University of Mary, Bismarck, ND, USA
3Heart Institute Bnei-Zion Haifa Medical Center, Technion, Haifa, Israel
4Life Sciences Department, The Zinman College of Physical Education at the Wingate Collage, Netanya, Israel
Correspondence: Associate Professor of Clinical Exercise Physiology Chair, Department of Kinesiology, College of Health and Human Sciences, NC A&T State University Corbett Sport Center, Suite 215, room 216, John Mitchell Drive Greensboro, North Carolina 27411, USA, Tel 336.285.3560, Fax 336.334.7258
Received: February 15, 2019 | Published: February 28, 2019
Citation: Saghiv M, Welch L, Goldhammer E, et al. The effects of partial sleep deprivation and the maximal ndks exercise testing protocol on s-klotho, maximal oxygen uptake, and hemodynamic responses in young men. Sleep Med Dis Int J. 2019;3(1):25-30. DOI: 10.15406/smdij.2019.03.00062
Purpose: The purpose of the study was to examine the influences of partial sleep deprivation on young healthy trained men’s responses to the maximal NDKS exercise testing protocol.
Methods: 33 males 21.2±31 years of age, volunteered to participate in this study. Subjects underwent two maximal NDKS exercise tests, once after 7-8hours of sleep, and once after staying awake for 20hours. S-Klotho, blood pressure, and heart rate were obtained at baseline, immediate-post, and post a dynamic recovery of 15minutes. Oxygen uptake was measured throughout exercise.
Results: Significant differences were found between S-Klotho values at baseline and immediate-post of PSD and NPSD (463.31±18vs 651.17±70.81 pg·mL-¹, F(1,65) = 33.45, p = 0.01 and 463.31±64.18vs 727.14±81.3 pg·mL-¹, F(1,65) = 38.06, p = 0.01 respectively). Significant differences were found between conditions regarding PSD immediate-post S-Klotho concentration and that of NPSD (651.17±70.81 vs 727.14±80.3 pg·mL-¹, respectively, F(1,65) = 14.648, p = 0.02). Significant differences were found between conditions regarding baselinepost-recovery S-Klotho concentration and PSD(463.31±64.18 vs 522.68±51.98 pg·mL-¹, respectively, F(1,65) = 12.96, p - 0.03).Significant differences were found between immediate-post S-Klotho values and post-recovery (PSD: 651.17±70.81 vs 522.68±51.98 pg·mL-¹, F(1,65) = 31.2, p = 0.03) and (NPSD: 727.14±80.3 vs 513.41±55.24 pg·mL-¹, F(1,65) = 34.2, p = 0.02).
Conclusion: Partial sleep deprivation induced multiple negative significant differences in S-Klotho concentrations and in some cases, hemodynamic responses as well. Oxygen uptake was significantly lower while partially sleep deprived.
Keywords: men, partial sleep deprivation, s-klotho, NDKS, hemodynamic responses, exercise testing, blood pressure, maximal oxygen uptake, heart rate
The topic of aging and anti-aging has interested humanity from the start of time.1 In Greek myth (According to Hesiod's Theogony), the goddess Clotho spins the thread of life; the goddess Lakhesis determines the length of the thread; and the goddess Atropos cuts the thread.2 Different extents of sleep deprivation (partial and/or full) may negatively influence physiological responses, and function.3–8 Influences are characterized as endocrinological, behavioral, physiological, and neurological, as well as sex specific (male vs female).9–11 Negative influences reported include endothelial dysfunction, hypertension, decreased brain activity, cardiac dysfunction, heart rate variability, arrhythmias, blood pressure, renal function, and more.12–15 On the other hand, in humans and rats, various exercise modalities such as aerobic training, and resistance training negate part and/or all of the adverse effects via positive adaptation in nature.16–19 In humans, the S-Klotho enzyme, a type I membrane proteinis encoded by the KL gene.20,21 Without yet indicating the nature of the influence, the protein is associated with alcohol consumption, the degenerative process, bone lose, and acceleration of aging.22–26 As part of the growth process at the cellular level, S-Klotho helps determine the sensitivity to insulin, via mediating the binding of FGF19, FGF20, and FGR23 to their receptors.25 Via means of endothelium-derived Nitric Oxide production, S-Klotho protects the cardiovascular system,27,28 decreased TRPC6 expression, increases TRPV5expression, increases membrane expression of inward rectifier ROMK affecting cellular calcium homeostasis.
In mice, vitamin D hyper-vitaminosis is caused by under-expression of S-klotho; as well as altered mineral-ion homeostasis resulting in accelerated aging; a syndrome of accelerated aging; arteriosclerosis; impaired endothelium-dependent vasodilation; and impaired angiogenesis.25,29–31 Proven in mice, over-expression may prolong life span by 19-31%. In humans, adaptations to exercise positively influence Klotho gene expression epigenetically due to its increase.33 Increases in aerobic capacity, power output, and exercise tolerance increase circulating S-Klotho levels for the better.34,35 To the best of the authors’ knowledge, no prior published data exists as to the influences of partial sleep deprivation (less than 40hours of lack of sleep) on S-Klotho in men during and after a maximal exercise test of any sort. Thus, the aim of this study was to investigate the influences of partial sleep deprivation (20hours of lack of sleep) and a maximal Nustad, Dressler, Kobes, Saghiv (NDKS) exercise test on S-Klotho concentration (pg·mL-¹), heart rate (bpm), blood pressure (mmHg), and maximal oxygen uptake (mL∙Kg-1∙min-1) in young, healthy, and trained men.
Overview, subjects, recruitment and enrollment
After achieving Institutional Review Board (IRB) approval to conduct this study, subjects were asked to participate in the study. Thirty-threemen, 21.2±2.31years of age, volunteered to participate in this study. All participants were healthy and trained individuals. Subjects visited with the researchers 3-4times. Upon agreeing to participate, subjects received an informed consent form via email and/or hard-copy, read the form, and indicated in a clear manor they have fully understood its content, prior to signing the form. The subjects were given as many opportunities as needed and/or wanted to ask questions pertaining to every aspect of the study. Subjects then filled-out a health history questionnaire (HHQ) and signed the HHQ. The information in the HHQ and follow-up questions (if raised) was used to determine rather or not subjects were to be included or excluded from the study. Prospective subjects were excluded if they had diagnosed musculoskeletal injury, cardiovascular disease, pulmonary disease, mental health problems, endocrine instability, and/or were treated with medication for any reason.
Baseline measurements
Following inclusion in the study (as part of the first visit with the researchers), the subjects’ height, weight, heart rate, blood pressure, and a 5mL blood sample (from the median cubital vein) were obtained, recorded on file and/or labeled. Prior to leaving the lab, subjects were randomly assigned to their two maximal (NDKS) aerobic exercise tests. Using a table of random numbers, half of the subjects were assigned to be tested non-partially sleep deprived first (NPSD), and the other half, scheduled to be tested partially sleep deprived first (PSD). Subject were allowed to leave the lab in the absence of adverse reactions and/or return to baseline values.
Prior to exercise testing sessions
Instructions for all subjects included the completely avoidance of alcohol consumption of any sort, moderate/intensive exercise of any sort, caffeine of any amount, use of any over-the-counter medications, and/or stressful situations at least 8 hours prior to data collection. Subjects self-reported their compliance with these instructions.
Exercise testing (NPSD or PSD)
Subjects tested while partially sleep deprived, reported to the lab at 2am (up to four subjects were tested per data collection session; two at a time). Subjects were instructed to be completely awake from 6am the prior day (20 hours). Subjects were contacted via email, text message, and/or phone call the day before testing to assure compliance with the instructions. Only subjects that responded were tested. Others were rescheduled. Subjects tested while non-partially sleep deprived, reported to the lab at 6am (up to four subjects were tested per data collection session; two at a time). Subjects were instructed to sleep 7.5-8hours prior to testing. Subjects were contacted via email, text message, and/or phone call the day before testing to assure compliance with the instructions. Only subjects that responded were tested. Others were rescheduled. Upon arrival at the lab, the subjects were asked if they have complied with the pre-testing instructions. Subjects non-compliant with the instructions were rescheduled; all subjects were tested twice within a period of no more than two weeks in between tests. The least amount of time between tests was nine days.
Researchers assured that no intensive competitions or physical undertakings were scheduled in-between tests. Subjects compliant and without adverse signs were seated for five minutes, doing nothing. Afterwards, heart rate, and blood pressure were obtained and compared to the subjects’ baseline values. The subjects then continued to a warm up, followed by a NDKS maximal aerobic exercise test (see appendix A for actual protocol), and dynamic recovery following the test itself. The exercise test was terminated for the following reasons: 1) subject indicated he could not continue 2) no further increase in oxygen uptake was noted in light of workload increase. Heart rate, blood pressure, and gas exchange were obtained as the main variables of the study, while RPE (6-20 scale), and O2 sat were obtained every other minute during the exercise test for control reasons only (see appendix A). S-Klotho was obtained immediate-post as well as after subjects have undergone a dynamic recovery that included waking at 1.7miles per hour at 0% grade for the duration of fifteen minutes.
Samples and measurements
5mL blood samples were obtain (according to universal precautions for blood borne pathogens) from the median cubital vein and stored in BD Vacutainer™ Venous Blood Collection Tubes: SST™ Serum Separation Tubes with Conventional Stopperuntil analyzed; samples were then refrigerated. Subject without adverse reactions and upon return to baseline values were allowed to leave the lab. Blood samples were analyzed via Soluble Klotho (Human serum) Enzyme-Linked Immunosorbent Assay (ELISA) Kit SK00708-08 (Adipo Bioscience, Inc.), with a Standard range of 313-20,000 pg∙mL-1; Sensitivity of 80 pg∙mL-1; Intra-CV of 4-6%; and Inter-CV of 8-10%. Blood pressure was obtained utilizing an Omron sphygmomanometer; heart rate via Polar heart rate monitor and strap, oxygen saturation was obtained via AccuMed CMS-50D Pulse Oximeter Finger Pulse Blood Oxygen SpO2 Monitor. The treadmill used in this study was a NordicTrack C 990 Treadmill. Gas exchange analysis was conducted utilizing a Parvo Medics True One 2400 metabolic cart.
Statistical analysis
SPSS 23 for Windows was used to analyze the data, Comparisons between conditions (partial sleep deprivation vs non-partial sleep deprivation) were conducted via One-way repeated measures ANOVA and the Tukey post hoc test. Significance was set at p ≤ 0.05. We presented results as means±standard deviation.
In general
All subjects participated in this study without any prolonged adverse reactions. Some subjects had a temporary reaction to their blood being drawn (dizziness, elevated heart rate, hypertension, hypotension, and in four cases subjects reacted with syncope). All subjects left the lab without any adverse clinical signs.
Baseline measures
Presented in Table 1 are data for height, weight, BMI, heart rate, and blood pressure.
|
Variable |
Mean±SD |
|
N |
33 |
|
Height (cm) |
174±6.53 |
|
Weight (Kg) |
75.32±5.16 |
|
BMI (Kg∙m-2) |
24.81±0.78 |
|
HR (bpm) |
67.7±3.94 |
|
SBP (mmHg) |
115.01±6.22 |
|
DBP (mmHg) |
68.42±5.01 |
Table 1 Baseline values for height, weight, BMI, heart rate, and blood pressure (mean±SD)
BMI, Body Mass Index; HR, heart rate; SBP, systolic blood pressure; DBP, diastolic blood pressure; O2sat, Oxygen saturation; cm, centimeters; Kg, kilograms; m, meter; bpm, beats per minute; mmHg, millimeter mercury.
S-Klotho: S-Klotho concentrations were significantly higher immediate-post compared to baseline and post-dynamic recovery for both PSD and NPSD conditions (463.31±18vs 651.17±70.81 pg·mL-¹, F(1,65) = 33.45, p = 0.01 and 463.31±64.18vs 727.14±81.3 pg·mL-¹, F(1,65) = 38.06, p = 0.01 respectively). S-Klotho concentration immediate-post was significantly higher while non-sleep deprived compared to the same measurement while partially sleep deprived (651.17±70.81 vs 727.14±80.3 pg·mL-¹, respectively, F(1,65) = 14.648, p = 0.02). Significant differences were found between conditions regarding baseline and post-recovery S-Klotho concentration and PSD (463.31±64.18 vs 522.68±51.98 pg·mL-¹, respectively, F(1,65) = 12.96, p = 0.03).Significant differences were found between immediate-post S-Klotho values and post-recovery (PSD: 651.17±70.81 vs 522.68±51.98 pg·mL-¹, F(1,65) = 31.2, p = 0.03) and (NPSD: 727.14±80.3 vs 513.41±55.24 pg·mL-¹, F(1,65) = 34.2, p = 0.02).
Dynamics of S-Klotho concentration are presented in Table 2 and Figure 1 below.
|
Condition |
Variable |
Baseline |
Immediate-Post |
Post Dynamic Recovery |
|
NPSD |
Average |
463.31 |
727.14αβ |
513.41β |
|
SD |
64.18 |
81.3 |
55.24 |
|
|
PSD |
Average |
N/A |
651.17β |
522.68†β |
|
SD |
N/A |
70.81 |
51.98 |
Table 2 S-Klotho (pg·mL-¹) concentrations according to condition and stage of exercise testing (mean±SD)
NPSD, non-sleep deprived; PSD, partially sleep deprived; SD, standard deviation; α, significant difference between conditions; β, significant difference from the measurement of a stage prior in the same condition; †, significant difference between post recovery to baseline.
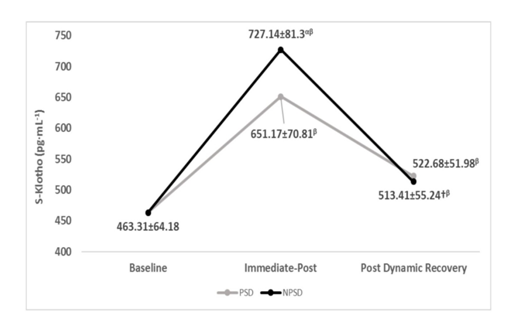
Figure 1 S-klotho (pg·mL-¹) concentrations according to condition (mean±SD).
NPSD, non-sleep deprived; PSD, partially sleep deprived; SD, standard deviation; α, significant difference between conditions; β, significant difference from the measurement of a stage prior in the same condition; †, significant difference between post recovery to baseline.
Heart rate: Significant differences (p≤05) were found between conditions for the heart rate at the start of the exercise test (test start and stages 1-4). All other comparisons were non-significant (p>0.05). Presented in Figure 2 are changes in heart rate according to the stage of the NDKS sub-maximal test.

Figure 2 Changes in heart rate (bpm) according to condition, during the maximal NDKS exercise test (mean).
Bpm, beats per minute; NPSD, non-sleep deprived; PSD, partially sleep deprived; α, significant difference between conditions; β, significant difference from the measurement of a stage prior in the same condition; n, number of subjects contributing to the average.
Systolic blood pressure: Systolic blood pressure was non-significantly higher (p>0.05) while partially sleep deprived for the majority of the tests. For both conditions, all comparisons were significantly different (p≤05) between stages within the condition. Changes in systolic blood pressure according to the stage of the NDKS sub-maximal test are presented in Figure 3.
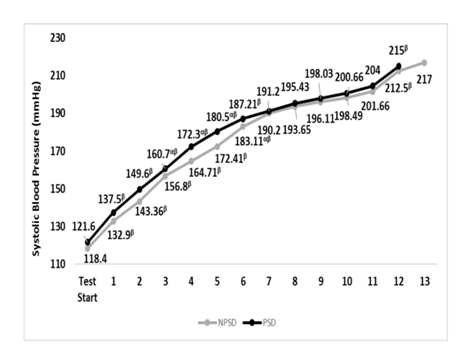
Figure 3 Changes in systolic blood pressure (mmHg) according to condition, during the sub-maximal NDKS exercise test (mean).
SBP, systolic blood pressure; RSBP, resting systolic blood pressure; mmHg, millimeters of Mercury; NPSD, non-sleep deprived; PSD, partially sleep deprived; blood pressure not measured while running; α, significant difference between conditions; β, significant difference from the measurement of a stage prior in the same condition.
Diastolic blood pressure: Diastolic blood pressure was within a very narrow range of five mmHg for both conditions and during all stages. None of the comparisons between conditions was significant (p>0.05).Changes in diastolic blood pressure according to the stage of the NDKS sub-maximal test are presented in Figure 4.

Figure 4 Changes in diastolic blood pressure (mmHg) according to condition, during the sub-maximal NDKS exercise test (mean).
DBP, diastolic blood pressure; RDBP, resting diastolic blood pressure; mmHg, millimeters of Mercury; NPSD, non-sleep deprived; PSD, partially sleep deprived; blood pressure not measured while running; α, significant difference between conditions; β, significant difference from the measurement of a stage prior in the same condition.
Maximal and peak oxygen uptake: None of the subjects reached maximal oxygen uptake while partially sleep deprived. While non-sleep deprived, seven subjects reached maximal oxygen uptake, while the rest peaked. Oxygen uptake was significantly higher for NPSD compared to PSD (57.45±18 vs 52.31±2.67 mL∙Kg-1∙min-1; F(1,65) = 23.54; p = 0.031). Comparisons between maximal oxygen uptake, and the comparison of subjects that have peaked vs maxed between conditions are presented in Table 3.
|
Condition |
Variable |
Maximal/Peak |
No. of subjects that have Peaked |
No. of subjects that have Maxed |
|
NPSD |
Average |
57.45α |
26 |
7α |
|
SD |
4.18 |
|||
|
PSD |
Average |
52.31 |
33 |
0 |
|
SD |
2.67 |
Table 3 Maximal oxygen uptake (mL∙Kg-1∙min-1)according to condition (mean±SD)
NPSD, non-sleep deprived; PSD, partially sleep deprived; blood pressure not measured while running; α, significant difference between conditions; mL, milliliter; Kg, Kilogram; min, minute; SD, standard deviation.
Test termination: The absolute number of exercise terminations was significantly lower (p≤05) while none partially sleep deprived for termination in stage 9 (11 vs 21 terminations; F (1,31) = 43.57; p = 0.036), while significantly higher for stage 10 (16 vs 10 terminations; F(1,25) = 25.11; p = 0.042). Non-significantly (p>0.05), more subjects were able to reach more advanced stages while none partially sleep deprived. Comparisons between conditions for the number of terminated test are presented in Table 4.
|
Condition |
Stage 9 |
Stage 10 |
Stage 11 |
Stage 12 |
Stage 13 |
|
NPSD |
11α |
16α |
3 |
2 |
1 |
|
PSD |
21 |
10 |
1 |
1 |
0 |
Table 4 Number of subjects according to exercise termination stage
NPSD, non-sleep deprived; PSD, partially sleep deprived; blood pressure not measured while running; α, significant difference between conditions.
The researchers are unaware of published data pertain to this specific topic and design. With that said, S-Klotho is a biomarker of aging and anti-aging alike, dependent on the extent of gene expression.34,35 Thus, this study starts to shade light on the connection between partial sleep deprivation and aging/anti-aging represented via S-Klotho concentration under certain conditions. Sleep deprivation (acute and/or chronic) is well documented as an influencer of function and performance in both healthy and clinical populations, across sex, gender, and age to different extents.3–19 Proper sleep has been indicated as an anti-oxidative factor.36,37 The present study demonstrates a clear and significant influence of partial sleep deprivation on S-Klotho’s response to the maximal NDKS aerobic exercise test in young, healthy, and trained men, while compared to being non-partially sleep deprived. The data of this study suggest that partial sleep deprivation of 20hours, is a strong enough stressor, resulting in lower levels of S-Klotho immediate-post, and post-dynamic recovery, while compared to those of the non-partially sleep deprived state.
The S-Klotho protein has been identified as part of the response of the creation of ROSs.36–38 Aerobic exercise is well documented as the inducer of oxidative stress.38–40 As a result of endoplasmic reticulum stress and mitochondrial oxidative stress, a greater extent of ROSs is created.41 It is estimated, yet not proven, that about 2% of oxygen uptake during exercise, results in ROSs.42 Logically, an increase in oxygen uptake and oxidative stress will increase the production of ROSs and the need for S-Klotho to battle it. ROSs are associated with the ageing process and cell dysfunction, hence one of the possible mechanisms in which S-Klotho can contribute to anti-aging.43 The non-statistically significant differences for S-Klotho concentrations post-dynamic recovery indicated that though while partially sleep deprived, the subjects did not achieve as high an oxygen uptake as while non-partially sleep deprived, S-Klotho levels were similar for both conditions. This may indicate an impaired ability to recover while partially sleep deprived. Since while non-partially sleep deprived, subjects lowered their S-Klotho levels more at the absolute aspect within the same time given for recovery, compared to while partially sleep deprived, one can assume that the recovery and contradiction of ROSs was faster while non-partially sleep deprived. Very few data exist regarding the influence of partial sleep deprivation on performance and oxygen uptake in particular, especially maximal oxygen uptake. A decrease in maximal oxygen uptake measured in an incremental maximal exercise test due to a shorter duration of sleep as well as lower quality of sleep was previously reported.44 The researchers reported oxygen uptakes of 44-59mL∙Kg-1∙min-1, which are comparable with the results of this study.44 The result of this study show that for the most part, subjects were able to achieve slightly higher HRmax values, which could be explained by the fact that they were somewhat younger in age.44
In a study from 2017, recovery was influenced for the worse by one night of partial sleep deprivation. Although subjects were cyclists and older in age, as well as the exercise test being a HIIT session, recovery was impaired twenty-four hour post (Appendix A). The 2017 study and its findings raise the possibility that recovery was impaired for this study’s subjects immediately post and within 15minutes of recovery.45 Researchers also reported subjects in their study were sleepier and less motivated within the 24hours that followed. It is possible that the subjects of this study experienced the same, though the design of this study did not address these topics.45 The loss of sleep is documented as an influencer of blood pressure, with a greater negative affect as age increases.46 Our results stand in contradiction to the findings of past studies as non-significant differences were found for blood pressure between the two conditions.
Minutes |
Workload |
Comments |
Warm-up |
2.3mph × 0% grade |
Measurements taken |
1 |
3.1mph × 5% |
Measurements taken |
2 |
3.7mph × 5% |
|
3 |
3.7mph × 6% |
Measurements taken |
4 |
4.3mph × 6% |
|
5 |
4.3mph × 7% |
Measurements taken |
6 |
5.0mph × 7% |
|
7 |
5.0mph × 8% |
Measurements taken |
8 |
5.6mph × 8% |
|
9 |
5.6mph × 9% |
Measurements taken |
10 |
6.2mph × 9% |
|
11 |
6.2mph × 10% |
Measurements taken |
12 |
6.8mph × 10% |
|
13 |
6.8mph × 11% |
Measurements taken |
14 |
7.4mph × 11% |
|
15 |
7.4mph × 12% |
Measurements taken |
16 |
8.0mph × 12% |
|
17 |
8.0mph × 13% |
Measurements taken |
18 |
8.6mph × 13% |
|
19 |
8.6mph × 14% |
Measurements taken |
20 |
9.2mph × 14% |
|
21 |
9.2mph × 15% |
Measurements taken |
22 |
9.8mph × 15% |
|
23 |
9.8mph × 16% |
Measurements taken |
24 |
10.4mph × 16% |
|
Appendix A The NDKS Aerobic Exercise test
The data of this study suggest that twenty hours of partial sleep deprivation is a strong enough stimulus affecting S-Klotho concentration in response to the maximal NDKS aerobic exercise testing protocol. Our results support the possibility of an impaired ability to elevate S-Klotho as a result of maximal exercise and partial sleep deprivation, a lesser need to battle ROSs since oxygen uptake was lower, and/or and impaired ability to return to baseline levels post-dynamic recovery. The results of this study fairly align with the majority of existing data pertaining to the influences of partial sleep deprivation on hemodynamic variables and oxygen uptake, though data is limited. As many people exercise and are required to perform under less than optimal sleep condition, the researchers find value in the further investigation of these influences.
None.
The authors declare that there is no conflict of interest.

©2019 Saghiv, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.