eISSN: 2377-4304


Standard surgical treatment for early-stage cervical cancer includes radical total hysterectomy. However, there is firm evidence that in selected cases surgery can be limited to removal of the cervix (trachelectomy), while maintaining the uterine body, in order to preserve fertility. When performed abdominally, both uterine arteries are usually ligated to parametrial level, which theoretically alters the blood perfusion of the uterus, with the consequent compromise of the chances of pregnancy.
The objective is to present the abdominal radical trachelectomy technique, preserving the integrity of both uterine arteries (TRAPAU) and its initial results. The clinical case of a patient with cervical cancer in Stage IB1, from the CAMEC Institution, city of Rosario, Uruguay, is analyzed. The TRAPAU technique was performed for the conservative treatment of fertility. The technique could be performed satisfactorily without complications. The irrigation of the uterus was evaluated at 60 days and one year, by means of a Doppler ultrasound study, verifying adequate perfusion through the uterine arteries. Twelve months after surgery, she is disease-free. We conclude that the TRAPAU technique achieves optimal surgical radicality of the disease, maintaining the integrity of the uterine irrigation,
Keywords: Cervical cancer, Conservative surgery, Fertility preservation, Trachelectomy. Preservation of uterine arteries. Doppler uterine arteries post cervical cancer surgery
Cervical cancer continues to be one of the most frequent tumors among women; It ranks fourth in incidence worldwide, and is the second leading cause of death from gynecological cancer in women. It is one of the most common cancers in patients under 40 years of age.1
Surgical treatment is the approach of choice in the initial stages, and currently it can be adapted to patients who wish to preserve their fertility with the same results in terms of overall and disease-free survival as radical hysterectomy.
In 2018, the International Federation of Gynecology and Obstetrics (FIGO) modified the classification of cervical cancer, with changes in stages IA and IB, adapting them to the indication of fertility-conserving treatment. Fertility-sparing treatments are possible in stages IA and IB1 as long as the lymph nodes are reported histologically negative on freezing, and there is informed consent with the request of the patient to perform this type of procedure. Although cervical conization is a conservative treatment used, it is mainly limited to stages IA1 without invasion of the lymphovascular space.2
The radical trachelectomy strategy consists of removing the cervix together with the parametria and the upper third of the vagina, preserving the uterine body, with the subsequent possibility of pregnancy. The radical trachelectomy technique consists of resection of the cervix with or without preservation of the uterine artery.3 The approach routes can be abdominal (laparoscopic or laparoscopic) or vaginal with laparoscopic lymphadenectomy. The upper margin of the resection of the cervix should be examined microscopically by freezing during surgery, given that, if it is positive, conservative treatment is suspended and conventional radical surgery is performed. In the vaginal procedure, the ascending branch of the uterine artery is preserved, ligating only the lower cervical-vaginal branches,
Preservation of the uterine artery or its ascending branch is considered to be a factor that would play an important role in future obstetric outcomes.4 For this reason, this technical variant has been developed, which consists of preserving the uterine arteries during radical abdominal trachelectomy (TRAPAU).
The TRAPAU technique is feasible in women with a desire to conceive and cervical cancer in stages IA2 (invasion greater than 3mm and less than or equal to 5mm deep) and IB1 (tumor greater than 5mm and less than or equal to 2cm) of the FIGO 2018 classification, and who meet the following criteria: absence of lymphovascular invasion in the histopathological study, pelvic lymph nodes reported without invasion in the intraoperative pathology study, absence of tumor invasion in the upper margin of the resection of the cervix, also evaluated by intraoperative microscopic study, possibility of patient follow-up, and informed consent.5
The TRAPAU technique consists of performing a laparotomy with bilateral pelvic lymphadenectomy and anatomical-pathological study of the lymph nodes.6 In the case of positive lymphatic invasion, the conservative technique is suspended and radical surgery for neck cancer is performed, or surgery is suspended and subsequent treatment with radiotherapy. After confirming the negativity of the lymph nodes, we proceed with the radical trachelectomy, preserving the uterine arteries as was said.
Objective: Our objective is to present the first case of application of this technique in Uruguay with its initial results and to review the literature on the subject.
We present the clinical case of a 29-year-old patient, healthy, with no personal history to highlight, nulliparous. In the annual gynecological control, an exophytic macroscopic lesion of the cervix is visualized. A biopsy of the lesion was performed, obtaining fragments of 2 and 3mm in the colposcopy. The pathological anatomy reported in the microscopy an extensive carcinoma in situ, without invasion of the stroma by Hematoxylin Eosin staining. With this diagnosis, a surgical conization was performed. A 37 by 23 by 24mm piece was obtained, to which serial cuts were made every 2mm to its entirety. Microscopically, a non-keratinizing, infiltrating squamous cell carcinoma-like lesion with a surface extension of 12mm and stromal invasion of 7mm, without vascular emboli, was reported.
The FIGO 2018 classification was used to perform the staging of the clinical case. The patient was staged in Stage IB1. Due to her desire to preserve fertility, consultations with the reproductive team were made and therapeutic options were presented to her.
Given that it was an initial stage of cervical cancer, added to the desire to preserve fertility, performing a radical abdominal trachelectomy was considered, preserving the uterus and, if possible, the uterine arteries, and pelvic lymphadenectomy, which was understood and accepted by the patient, signing the corresponding consent.
The surgery was performed at the surgical center of the CAMEC Institution, FEPREMI, Rosario, Uruguay.
An abdominal approach was performed through a median infra-umbilical incision. Abdominal examination revealed no enlarged lymph nodes or elements of distant dissemination. A bilateral pelvic lymphadenectomy was started, sending the resected tissues to an extemporaneous study of pathological anatomy, confirming their indemnity.
Radical trachelectomy was then continued, for which the anterior peritoneum was opened and subsequent bladder descent. Skeletonization of the uterine artery was carried out in its entire extrauterine portion, visualization of the ureter in its pelvic path until it entered the bladder and its unroofing. In this way, the resection was achieved together with the piece of the lateral and anterior parametria. Section of the utero-sacral ligaments in their pararectal portion with preservation of the hypogastric plexus. Transverse section of the vagina 2 cm below the cervicovaginal junction. Section of the cervix at its junction with the isthmus and remission of the piece for its intraoperative anatomical-pathological evaluation, evaluating negative margins. Fixation of the vaginal vault to the lower portion of the uterus using absorbable stitches. A latex tube was left through the internal cervical orifice of the cervix, exteriorized towards the vagina, in order to avoid synechiae of said orifice (Figures 1–3).
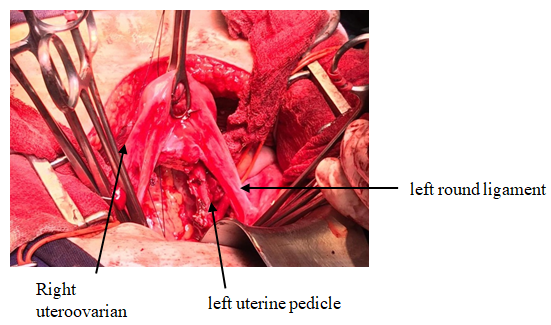
Figure 1 Trachelectomy already performed. The body is observed uterus elevated by forceps and its pedicles.

Figure 2 Point from anterior border of vagina to inferior border anterior aspect of the uterine body.

Figure 3 Central and lateral points of union of the upper border of the vagina to the lower border of the anterior aspect of the uterine body.
The TRAPAU technique was performed satisfactorily without complications. The patient did not require transfusions and intraoperative bleeding was 300cc. Intraoperative prophylactic antibiotics were indicated using Cefazolin 2g monodose. The duration of the surgical procedure was three hours. The bladder catheter was removed 48 hours postoperatively and the patient was discharged home on the fourth day. The vaginal tube was removed 30 days after the procedure.
The definitive pathological anatomy of the trachelectomy piece reported: absence of squamous lesions in the cervix, with free lateral borders, commissure and vertex, parametria without lesions. Thirteen reactive lymph nodes without metastatic replacement were examined. Clinical postoperative controls were performed at 7 and 30 days.
At 60 days after surgery, uterine irrigation was evaluated by transvaginal ultrasound and color Doppler study. It was found that the size of the uterine body was normal, with uterine pedicles present, whose flows were of medium resistance. Utero-ovarian pedicles with preserved blood flow were also identified (Figure 4) (Figure 5).
Oral contraception was started with ethinyl estradiol and drosperinone tablets. At 90 days, he was controlled by colposcopy, which ruled out pathology. The patient continued menstruating without dysmenorrhea and with characteristics similar to those prior to surgery. Remote controls, both clinical and through Oncological Colpocytology and Colposcopy at 6 months and one year after surgery, did not show elements of tumor persistence or recurrence.
One year after surgery, and in the absence of elements suggestive of neoplastic activity, a new Doppler ultrasound study was performed, which showed adequate perfusion through the uterine arteries, spiral arteries, and intramyometrial arteries (Figures 6–9).
Cervical cancer represents the third most frequent cancer in women in Uruguay, after breast and colorectal cancer. Approximately an average of 327 new cases are registered each year, corresponding to an incidence rate of 15.28 per 100,000, and a mortality rate of 5.47, which represents about 134 annual deaths.7 In the United States, the incidence of cervical cancer it is greater between 35 and 49 years of age, and decreases progressively from that age. In reproductive age (20 to 45 years) the reported incidence is 47.3 per 100,000 women.8
Given the notorious fertility delay in recent decades, a certain number of patients will require conservative treatments to preserve their fertility. Traditionally, options for the treatment of cervical cancer include total hysterectomy, radical hysterectomy with pelvic lymphadenectomy, or radiochemotherapy. As approximately 40% of these cases are diagnosed in patients under 45 years of age, definitive surgical management can cause the abolition of their reproductive capacity due to both surgical and functional causes.9
For this type of highly selected patients, in early stages (IA1–IB1), a fertility preservation treatment is recommended. Options for trachelectomy range from a cold cone, a cold cone with lymph node evaluation, or a radical trachelectomy with lymph node evaluation.
Cervical conization is one of the conservative treatments, but it is indicated in stages IA1, and it is an accepted option in cases of stages IA1 with invasion of the lymphovascular space and in stages IA2 eventually, and in these cases it must be accompanied by a lymphadenectomy. extraperitoneal laparoscopic.10
To be a candidate for radical trachelectomy, patients must have no history of infertility; and they must be early stages of the same, understanding as such cervical cancer stages IA1 with lymphovascular invasion, IA2 or IB1 with a lesion size ≤2cm; and absence of lymph node metastases. The histological type must be squamous cell carcinoma or adenocarcinoma. Neuroendocrine tumors, gastric-type adenocarcinomas and malignant adenoma are not candidates, nor are Stage IB2 tumors. In this sense, a prospective study of 88 patients who underwent laparoscopic radical trachelectomy for tumors larger than 2cm, has shown a higher incidence of recurrence greater than 20%.11
Regarding the pregnancy rate for the type of patients selected, it is increasingly encouraging, ranging between 40% and 74%.12
Radical trachelectomy consists of en bloc removal of the cervix, 2cm of the vaginal vault and the parametria, preserving the uterine body to which it joins the remaining vagina. Radical surgical methods include radical vaginal trachelectomy (VRT) with laparoscopic pelvic lymphadenectomy, abdominal radical trachelectomy (ART), laparoscopic radical trachelectomy, or robot-assisted radical trachelectomy.13
A systematic review from 2020 concludes that, although the literature is limited in terms of the number of cases and series, oncological results such as recurrence rate, mortality due to disease, injury-free interval and overall survival are favorable, with no differences differences between the different approaches to radical trachelectomy. However, the pregnancy rate and obstetric results appear to be higher using the vaginal approach.14
Vaginal trachelectomy has a recurrence rate of 4.1% and a survival rate of 2.5%, with no differences with radical surgery.15 In a case-control study comparing 137 women with tumors smaller than 2cm who underwent VRT versus controls who underwent radical hysterectomy, the 5-year recurrence-free survival rate was similar for both groups (95 and 100% respectively).16
The incidence of infertility after TRV varies widely from 14% to 41% according to different studies. After TRV, cervical factors account for 40-75% of fertility problems, with the remainder due to causes unrelated to surgery. The first-trimester miscarriage rate after radical trachelectomy is comparable to the rate in the general population (10% to 20%). The spontaneous abortion rate in the second trimester after TRV varies from 3 to 19%, which is higher than that of the general population (2%). Post-trachelectomy cervical factors may predispose the patient to the development of cervical insufficiency and/or chorioamnionitis and subsequent pregnancy loss. The rate of preterm delivery increases after a radical trachelectomy and is around 50%.17,18
Abdominal radical trachelectomy has a recurrence rate of 3.3% and death from disease of 1.5%. The infertility rate of the abdominal route is higher than the vaginal route. The abortion rate in the first trimester is similar to that of the general population.19
The greatest advantage of the abdominal route compared to the vaginal route is the shorter learning curve without the need to acquire vaginal and laparoscopic skills. Another advantage would be the possibility of obtaining more parametrial tissue, which would be a good option in those patients with larger lesions. Likewise, in patients with anatomical distortions and in those in which the vaginal approach is not possible, abdominal access is a real option. Disadvantages include greater blood loss, longer hospital stay, and bilateral sectioning of the uterine arteries, which could cause endometrial atrophy, cervical stenosis, as well as low birth weight in future pregnancies.20,21
In a study comparing the different approaches to radical trachelectomy, the vaginal approach had the highest pregnancy rate. There are several reasons that can explain these results. On the one hand, compared to ART, the vaginal route is considered a minimally invasive technique that can reduce intra-abdominal and pelvic adhesions, as well as mainly preserve the upper branches of the uterine artery, which would improve uterine irrigation.22
Nowadays, it is a matter of debate about the real benefit or not of the preservation of the uterine arteries during abdominal radical trachelectomy with a mainly reproductive purpose, with multiple studies both for and against it.
Wang in 2020 highlights the benefit of preserving the uterine arteries, which were followed up with tomography in evolution, highlighting their patency, concluding in favor of preserving them in abdominal radical trachelectomy.21
A review by Kim in 2019 concludes that uterine artery preservation supports the maintenance of uterine arterial blood flow and should be used by those performing minimally invasive radical trachelectomy, with promising obstetric and oncological results.23
To assess the contribution of uterine artery preservation as a contributing factor to fertility, Tang compared computed tomography angiograms of patients after radical abdominal trachelectomy with uterine artery preservation versus ligated artery preservation and found that 87.5% of Anatomically preserved uterine arteries were occluded after surgery. After abdominal radical trachelectomy, 65.4% of the patients had their uterus perfused from the collateral circulation of their ovarian arteries.24
Escobar et al. analyzed and measured uterine perfusion using laser angiography during uterine artery preservation and non-preservation during radical trachelectomy. Based on real-time angiography during surgery, the authors conclude that there is no need to preserve the uterine arteries during radical trachelectomy in order to maintain uterine viability.25
We controlled the preserved uterine arteries by color Doppler at 60 days and one year, demonstrating permeability and normal flow in them, not agreeing with the conclusions of Tang who found that most of the anatomically preserved uterine arteries were occluded after the surgery, nor with the conclusions of Escobar et al. who considered that there is no need to preserve the uterine arteries in order to preserve uterine viability, since the blood supply through the uterine arteries should, at least theoretically, preserve said viability.
Determination of uterine artery flows by Doppler study correlates with pregnancy rates, but diagnostic certainty is relatively low. Only large deviations from normal, such as shunts, absence of diastole, reverse flow, are easily detectable. To assess defects of reproductive importance, it is necessary to use modern, high resolution devices, equipped with Doppler and "Power Doppler", very sensitive, and to carry out individualized studies and serial follow-ups that correlate the results of the flows with the hormonal determinations and possibilities of pregnancy. . There are still no studies that correlate the results of the Doppler of the uterine arteries with the probability of pregnancy after the TRAPAU technique.
The clinical case of a patient with stage IB1 neck cancer according to the FIGO 2018 classification, with a desire to conceive, who was offered a conservative technique with preservation of the uterine arteries in order to improve her condition, was presented. reproductive prognosis. The technique was performed without complications, without tumor involvement a year after the procedure, and the existence of adequate blood flow in the uterine arteries was demonstrated by Doppler ultrasound at 60 daysand a year.
The future of the facts will determine the definitive success in terms of oncological safety and the real possibilities of conceiving a pregnancy, with good evolution of the same, and of obtaining a viable, healthy and term product as far as possible.
We believe that this is a successful treatment strategy from the oncological and reproductive point of view, which should be evaluated in the future for these particular cases, together with the possibility of validating this technique as a standard for these special clinical cases, with cancers of cervix in early stages and conceptional desire.
None.
None.
The authors declare having no conflict of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.