eISSN: 2572-8474


Research Article Volume 1 Issue 3
1Department of Surgery A, Odense University Hospital, Denmark
2Faculty of Health Sciences, University of Southern Denmark, Denmark
3Faculty of Health and Technology, Institute of Nursing, Denmark
4Department of Gynaecology and Obstetrics, Karolinska University Hospital, Sweden
Correspondence: Marianne K Thygesen, University of Southern Denmark, Department of Surgery A, Denmark, Tel +45 5045 9617
Received: October 31, 2016 | Published: December 8, 2016
Citation: Thygesen MK, Holt KA, Mogensen O. The significance of tailored, web-based information on experiences regarding perceived self-management in ovarian cancer patients in the diagnostic phase-an experimental study. Nurse Care Open Acces J. 2016;1(3):53-57. DOI: 10.15406/ncoaj.2016.01.00016
Cancer patients can experience a low self-management, which is associated with burn out and negatively associated with health-related quality of life. Patient-provider time at hospitals is often short and patients can lack knowledge, communication and support. We aimed to evaluate the influence of a healthcare-professional developed website, available to both patients and relatives, on patients’ experienced self-management before surgery for ovarian cancer. In an experimental study, Danish women with ovarian cancer were consecutively included if they would participate and had a relative, willing to offer attention to the cancer situation. The control group had standard care, the intervention group plus their relatives had additional access to a website with cancer-specific physical, psychical, and practical information. The validated questionnaires Cancer Behavior Inventory and Sense of Coherence provided data for statistical analysis. Patients’ difference in change in Sense of Coherence over time was statistically significant in favor of those who had used the website (mean difference 4.42, p<0.001).Patients’ and relatives’ access to our website prevented a decrease in self-management of Danish women in the diagnostic phase of ovarian cancer. Such support might be helpful to all patients approaching critical illness and who have a helpful relative, but this needs further investigation.
Keywords: website, perceivedself-management, ovarian cancer, diagnostic period, experimental study
CBI-B, cancer behaviour inventory; SOC, sense of coherence
A cancer trajectory is stressful for patients and lack of information, communication and support from healthcare professionals as well as socially contributes to this distress.1–5 Moreover, the patients’ in-hospital time is reduced,6–8 which decreases the direct contact with health care professionals. Therefore additional ways of communicating should be considered in order to increase support to the patients.9 Patients increasingly use the world-wide-web to gather information on health-related issues.10,11 Some prefer to access a large amount of information in an attempt to attain an overview or acquire extended knowledge, while others prefer receiving tailored information day-by-day.10 Internet information may improve empowerment12 but in other cases the www-based information is considered unqualified or incorrect.13 The positive and negative effects of web-based information can be addressed by establishing a website with healthcare professional-controlled information. A thorough search in Google Scholar and the databases PubMed, Ovid via EMBASE and PsycINFO, EBSCO via CINAHL and the Cochrane Library, using different terms of education, self-care with cancer, and computer, revealed that web-based information (with or without a possibility of e-contact to others) increases the patients’ knowledge, but the influence on self-management needs further investigation.9,14–16
People suffering from a disease, including cancer, can present a poor experienced self-management,17–19 but in cancer patients it has been possible to avoid a decrease, or regain a decrease in self-management after treatment.20 Moreover, support in specific from relatives might be important for cancer patient,21 and dialogues between patients and relatives about information relevant for the cancer situation might support a change in patients’ self-management.22 Avoiding a decrease or regaining a decrease in self-management was demonstrated with use of a multidisciplinary education programme focussing on promotion of health and self-care ability of patients after diagnosis.20 Such a program was led by healthcare professionals who provided and facilitated information and discussion regarding treatment, post treatment, and coping with cancer trajectories, as well as provided contact information to relevant healthcare professionals. However, such events were group-sessions, spend healthcare professional time, and started after surgery and definite diagnosis.20
The aim of this study was to evaluate the influence of a healthcare professional-developed website solely including information, made available to both patients and relatives, on patients’ own experienced self-management in the diagnostic phase before surgery for cancer.
Study design and setting
An experimental study was conducted with the inclusion of patients in both control and intervention groups within 13 months from the same gynecological hospital department. This department serves 1.2 million adults in Denmark. The control group was included within the first five months and had usual care. Control participants were tested alongside the development of a website. The intervention group was also included over five months, and they received usual care and had access to the website. The study is registered at the Danish Data Protection Agency.
Study participants
We consecutively included patients after a physician appointment where patients got a plan of ovarian cancer surgery, and still waited on surgery and a definite diagnosis. Participants should be able to read and understand Danish, and should have a relative willing to offer attention to the cancer situation.
Intervention
The web-site: A website for gynaecological cancer patients and their relatives was developed in a collaborative project involving multi-media design students from Lillebaelt Academy in Odense, healthcare professionals at Odense University Hospital, and the third author. To meet the challenges of delivering information relevant to the recipients, a qualitative descriptive study was performed, including semi-structured interviews with gynaecological cancer patients and their relatives. In the analysis and interpretation, the third author collaborated with a psychologist with experience in the rehabilitation of cancer patients, a physiotherapist, a social worker, a general practitioner (GP), a nurse from the outpatient clinic, and a ward nurse.23 Textual elements of the website were written by the third author and all relevant pamphlets were made electronically available. The LIX number of the website ranged from 31-56. This corresponds to a text with readability from easy to very difficult for ordinary trained readers, where the most difficult text was about diagnosis and treatment. Video clips were created in collaboration with a cancer patient and a relative. Further an interactive, electronic map of the ward was developed which included the facility to click for a view of photos showing specific places on the ward. The website was in Danish and consisted of three pathways: “Patients”, “Relatives” and “The department”. With videos, still images, and text, the website offered practical, physical, and psychological information. This included:
Patients’ and relatives access to the website: Right after study entrance, patients and relatives in the intervention group got the URL to the website and a pamphlet, which was designed to serve as a teaster. Patients and their relatives were urged to visit the website, at least until admission for the planed surgery. No formal requirements were set for interaction between patients and relatives.
Research tools
Participants were asked to fill out a questionnaire with socio-demographic characteristics in addition with the following questionnaires:
Cancer related self-efficacy: Patients experience of cancer-specific self-efficacy, were measured using a brief version of the Cancer Behaviour Inventory (CBI) developed by Merluzzi et al.24 The brief version (CBI-B) is a 14-item questionnaire with a Likert-type scale, ranging from 1 (not at all confident) to 9 (totally confident). A total score is calculated by summing the scores and a high score is associated with a high level of confidence in “maintaining activity and independence, coping with treatment-related side effects, seeking social support, and maintaining a positive attitude”25 p 659. Total obtainable scores range from 14 to 126. The scale has previously been used in a Danish context to measure change in self-efficacy of cancer patients over a short duration.25,26
Sense of coherence: Antonovsky’s sense of coherence (SOC) scale27 short version with 13 items was used to measure resources that provide a successful coping i.e. a general comprehension of one’s approach to life in regard to the ability to manage oneself.28 This presents a way of viewing health in contrast to sickness.27,28 The Likert-scale range from 1 to 7, and includes three subscales: comprehensibility, manageability and meaningfulness. The total score is calculated by summing the scores, resulting in a total score ranging from 13 to 91, where a high score reflects a strong SOC. The scale has been used in a wide range of studies, including studies concerning cancer patients and their relatives, and in a range of settings, including Denmark.27,29
Time of measures
Participants in both groups filled in the questionnaires twice. First, at study entrance: right after their appointment with the physician where they received time for ovarian cancer surgery (for the control group at time T1, and for the website group at time T3. Second, at study exit: the day before the cancer surgery (for the control group at time T2, and for the website group at time T4. The questionnaires took approximately fifteen minutes to complete. Questionnaires were either returned in prepaid envelopes or handed to a ward nurse at admission. One reminder was send by post if a questionnaire was not received one week after expected arrival.
Statistical analyses
The difference between intervention and control group was tested using linear regression adjusted for the baseline value at T1 (respectively T3), age, education, and presence of comorbidity. The paired t-test was used for within group comparisons. The normality assumption was verified by visual inspection of Q-Q plots. Missing data was handled by complete case analysis. All analyses were performed using Stata 11.2 (Stata Corp. College Station, (TX).
Ethical considerations
The study adheres to the Declaration of Helsinki30 and the Ethical Guidelines for Nursing Research in the Nordic Countries.31 Patients were offered written and verbal information about the study before they agreed to involve a relative, and all participants received study information before they signed content. The study has a registered number at the Danish Regional Scientific Ethical Committee.
Sample
Between April 2010 and April 2011, a total of 239 patients were eligible for participation of whom 83 patients were included: 30 without and 53 with access to the website Figure 1. Data from non-participants was not obtainable. Baseline characteristics are summarized in Table 1 and between-group differences were not statistically significant (p=0.320). All participants had 8 to 14 days between T1 and T2, and T3 and T4, respectively. For those, who had access to the prepared website, the response rate for fully completed questionnaires at both T3 and T4 and combined with self-reported visit to the website, was between 51,0% and 62,3% Figure 1. On the contrary, drop-out rates, as those participants not compliant with our set-up, e.g. not visiting the website when access was given and/or not filling in both the questionnaires, was higher in the intervention group (from 49,0% to 37,7%) than in the control group (from 3,4% to 16,7%) Figure 1.
Characteristics |
Patients |
Relatives |
||
Control |
Intervention |
Control |
Intervention |
|
(n = 30) n (%) |
(n = 53) n (%) |
(n = 30) n (%) |
(n = 53) n (%) |
|
Other sickness |
15 (50) |
16 (30) |
||
Internet user |
20 (67) |
38 (72) |
22 (73) |
45 (85) |
Education <13 years |
22 (73) |
22 (42) |
13 (43) |
18 (34) |
Education > 13 years |
7 (23) |
22 (42) |
11 (37) |
30 (57) |
Age 17-60 |
13 (43) |
31 (58) |
20 (67) |
40 (76) |
Age 61+ |
17 (57) |
22 (42) |
9 (30) |
12 (30) |
Age mean (min-max) |
62.6 (40–82) |
56.2 (28–79) |
54.9 (28–74) |
52.4 (17–75) |
Table 1 Socio-demography of control and intervention group.
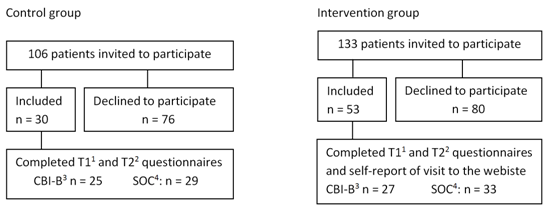
Figure 1 Flow chart of patients.
1T1: At study entrance: After accept of a plan of ovarian cancer surgery, 2T2: At study exit: The day before surgery for ovarian cancer, 3CBI-B: Cancer Behaviour Inventory questionnaire, 4SOC: Sense of Coherence questionnaire.
Patients’ self-efficacy for coping with cancer (CBI-B)
At baseline, the mean score of CBI-B in the control and intervention groups was 89.64(T1) and 91.3(T3), and at follow-up 87.0(T2) and 94.5(T4), respectively. The self-efficacy for coping with cancer decreased in the control group (mean-2.64, 95% CI: -8.10 to 2.82 (p=0.3285)) and increased for those who visited the website (mean 3.41, 95% CI: -0.50 to 7.31 (p 0.0847)). A difference in change between the two groups was observed, but this difference was not statistically significant (mean change 5.63, 95% CI: -0.73 to 12.00 (p=0.082)).
Patients’ Sense of Coherence (SOC)
The mean score of SOC for patients in the control group at baseline was 66.10(T1) and at follow-up 63.27(T2), and for the intervention group at baseline 70.72(T3) and at follow-up 70.83(T4). Within-group comparisons revealed a statistical significant decrease over time in the control group (mean-0.22, 95% CI: -0.38 to-0.06 (p=0.0086)) and a small not significant change in the group with self-reported visit on the website (mean 0.01, 95% CI -0.16 to 0.13(p 0.8413)). A statistically significant difference in change was observed between control and intervention group: mean change 4.42, 95% CI: 1.83 to 7.02 (p<0.001).
The aim of this study was to evaluate the influence of access for patients and relatives to a healthcare professional-developed website on patients’ own experienced self-management before surgery for cancer, and we tested a website solely including information tailored to women and their relatives in the diagnostic phase of ovarian cancer. Patients with access to the website were compared with patients without access to the website and both groups filled in the same questionnaires twice. The patient group without access to the website had a statistically significant decrease in their Sense of Coherence (SOC) in the period awaiting cancer surgery. This means, that their experienced resources available to cope with upcoming important situations decreased.28
The intervention group sustained their level of SOC and the difference to the control group was statistically significant. SOC in adulthood is regarded nearly stable over time28 and a temporary poor SOC is expected to increase after surviving the cancer. However, the time perspective of the increase is unknown. Moreover, a poor SOC is associated with low self-reported health and quality of life29,32,33 and up to 60% of female cancer patients suffer from post treatment psychological problems.34–37 Therefore, it is important to address self-management issues and accordingly to our study, specific web-based information regarding cancer-specific physical, psychical, and practical issues are of value already in the late diagnostic phase before surgery.
Our developed website for gynaecological cancer patients and their relatives include solely information and is as such a simple website. Websites for breast cancer patients can include interactive services as support opportunities with e-contact possibilities to both support groups, healthcare professionals and live chats, as well as services designed to train the users, but notably, only services with information and support were in specific useful to such patients.38 Our intervention was designed to inform both the patient and the relative and to ease a dialogue between them, thus we draw on relatives as supporters. This might be a useful strategy in western females waiting for gynecological cancer surgery, as such people seams to seek more support from their family than do their fellow patients scheduled for benign surgery.21 Moreover, it has been demonstrated that communication around information services can improve the patients’ self-management.22,39 However, we did not reach significant results in both our measures. Access to the website did not statistically significant change the self-efficacy in females awaiting ovarian surgery. We facilitated a dialogue between the patient and the relative regarding the accessible information, the cancer trajectory and challenges in this regard. Former studies facilitating such dialogues have proved able to statistical significant change the self-efficacy among the patients.22,40 Emotional and psychological support can be challenging for relatives to give,41,42 and this might be one explanation. Another explanation could be that our study may be underpowered since the difference in change between groups was in favour of our intervention and sense of coherence and self-efficacy are found to be positive correlated in the Danish background population.43
Our study design had an inherent risk of change of context over time. To meet this challenge, we decreased the time between usual care group and the intervention group and the entire research was done at the same department, with the same healthcare professionals, and included only female patients with a plan of primary surgery for ovarian cancer. The drop-out rate was higher in the intervention group, possibly because the tasks in the intervention group was time consuming, minor text parts could be difficult to read, and some patients might lack a computer capable to run the video sequences. However, in Denmark everybody have access to a computer with video processors for free at public libraries, which may negate some of the possible difficulties. Compared to the control group, the intervention group had a slightly higher SOC at study start. This reflects another inherent risk in all comparative non-randomized research, which we met in the study design by focusing on changes in scores. The relatives were expected to support the patients, but how and how much was not measured. The ward nurses routinely registered outpatient calls and the nurses could not report any changes in workload from before to after introduction of the website. Further research in relatives’ ways of supporting cancer patients might be helpful to the clinic. Our results are found among Danish ovarian cancer patients. These results are transferable to ovarian cancer patients in Denmark and might be transferable to other patients approaching critical illness in western cultures, but in such cases test in own setting is highly recommended.
Access to our informational website for both patients and relatives support the self-management of ovarian cancer patients before surgery. The access is associated with a sustained level of sense of coherence meaning that patients sustain their experienced available resources to cope with upcoming important situations until definite diagnosis, contrary to those without access to the website. Such support might prevent a decrease in perceived self-management in all patients who approach critical illness and have a helpful relative, but this needs further investigation.
The Danish Cancer Society and the Department of Gynecology and Obstetrics and The Department of Surgery, Odense University Hospital, Denmark funded this study. We thank the patients who participated in this study and the relatives who supported them, and we acknowledge the important collaboration with nurses Inger Juhl, Jette Johansen and Helle Frandsen from the Department of Gynaecology and Obstetrics at Odense University Hospital, who helped to adjust the study to clinical practice and supported the data collection. Further, we thank the statistician, PhD, René DePont Christensen for undertaking the statistical work.
The author declares no conflict of interest.

©2016 Thygesen, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.