eISSN: 2572-8474


Research Article Volume 6 Issue 5
1Department of Cardiac Intensive Care B2143, The Heart Centre, Copenhagen University Hospital Rigshospitalet, Denmark
2Department of Cardiac Intensive Care B2143, The Heart Centre, Copenhagen University Hospital Rigshospitalet, Denmark
3Department of Cardiology, Copenhagen University Hospital Rigshospitalet, Denmark
Correspondence: Jesper Kjaergaard, Department of Cardiac Intensive Care B2143, Copenhagen University Hospital, Rigshospitalet Blegdamsvej 9, 2100 Copenhagen, Denmark, Tel +4535453545
Received: November 11, 2019 | Published: November 20, 2019
Citation: Glud H, Grand J, Kjaergaard J, et al. Critical heart disease - the relatives’ perspective. Nurse Care Open Acces J. 2019;6(6):194-200. DOI: 10.15406/ncoaj.2019.06.00207
Background: Being a relative of a critically ill patient is associated with acute stress and the risk of neuropsychiatric late effects.
Objective: To investigate the relatives' experiences in a cardiac medical intensive care unit with a view to identifying areas in which the relatives need support and promoting cooperation between relatives and staff.
Method: Prospective, observational, questionnaire survey of 100 relatives of a semi-structured questionnaire. Relatives are included in the study on the patient's 3rd day of admission. Analysis of the open-ended questions was inspired by the thematic analysis.
Results: Of 139 invited, 100 responded (71%). The relatives were mainly cohabiting / spouse (70%). The majority (78%) responded that it was great or very important to be involved in the care. A minor group (8%) reported that they received too little information. The thematic analysis revealed three themes in where the relatives favored honest and specific information about the patient's condition and prognosis, how they struggled in an unfamiliar setting and were depending on staffs help to cope with the situation.
Conclusion: This study gives important insights into the relatives' feelings and needs when a patient is admitted to the intensive care unit. It is important that relatives are involved in the care and the relatives expect specific information about the patient's disease and prognosis. Future studies should investigate measures that can reduce stress and potential harmful effects in relatives.
Keywords: Nursing, relative’s experience, intensive care, cardiology, patient's family, post-intensive care syndrome, post-traumatic stress disorder, family
Intensive cardiac care is one of the most advanced and resource-intensive treatment areas in the healthcare system and involves advanced equipment, costly treatment modalities and high staff training requirements.1 In line with improvements in medical and surgical fields, more patients can be offered advanced curative or life-prolonging treatment. This development, along with the changing demographic trends in populations, is putting increasing pressure on the intensive care units.2 Intensive treatment is often indicated for serious illnesses which are with risk of death or serious complications. Emotional, existential and ethical dilemmas are a part of everyday life for patients, staff and relatives. Some critically ill patients can be treated and survive with good quality of life while others can have extended their life for a while. But when the treatment is futile, it should be terminated to avoid pulling the patient and relatives through unnecessary physical and psychological suffering.3 The patients' close relatives have a decisive influence on several aspects of the disease course. Relatives often act as the patient's representative in the intensive care unit and can assist with simpler care and provide emotional support to the patient.4 The relatives are often heavily burdened in the situation and in the long term they may develop psychological reactions and diseases,5,6 which can be particularly stressful as the relatives need help and support when the patient is discharged. It is estimated that 1 in 3 relatives of a deceased intensive care patient fulfills the criteria for depression or anxiety7 and relatives are also at risk of developing post-traumatic stress syndrome. Internationally, these reactions of the relatives have been given the name "post-intensive care syndrome-family".5,6 Managing this risk during disease therefore poses a particular challenge to the staff, who, in addition to their professional expertise in treatment and care, must try to address the relatives' concerns and needs and potentially reduce the risk of adverse long-term reactions.
The relatives' psychological condition during and after the patient's hospitalization remains to be poorly described. Our knowledge about involvement and support for relatives in cardiac medical intensive care units is sparse. There is a need for increased focus on this element of nursing, to improve our understanding of the relatives needs and potentially prevent stress and adverse long-term reactions. In addition, there is potential to exploit the relatives' knowledge and support in treatment and care. The purpose of the present study was to elucidate the relatives' experiences at a cardiac medical intensive care unit to identify areas where there is a need for support for the relatives and to promote cooperation between staff and relatives about the critically ill intensive patient.
The study was conducted as a prospective, observational survey of 100 consecutive respondents to a semi-structured questionnaire for relatives on a cardiac medical intensive care unit in a tertiary care hospital in Copenhagen, Denmark. The questionnaire consisted of 25 questions (23 closed questions with answer options and 2 open questions allowing for free text responses). Relatives were included in the study on the patient's third day of admission. It was voluntary to respond, and the answers were anonymous.
Adult (age ≥18 years) relatives of hospitalized patients with severe heart disease fulfilled the inclusion criteria. The only exclusion criterion was language barriers that made it impossible to understand the questionnaire, which was only available in Danish. The questionnaire was designed by a group of experienced intensive nurses, with a focus on clarifying following areas:
The open-ended questions were exploring information and the experience of being a relative in a cardiac intensive care unit.
Quantitative results were presented descriptively with numbers, percentages and differences. Analysis of the open-ended questions were inspired by the thematic analysis as described by Braun and Clarke,1,2 a method that offers a way of identifying and providing a detailed analysis of patterns across a set of data.
Thematic analysis is an iterative and progressive process and consists of six phases. First, the data are read numerous times to ensure immersion and notes regarding potentially interesting aspects of the data are made at this stage. Following familiarization, the entire set of data was coded thoroughly by HG and SN.
Codes were derived from the data in a bottom-up process; codes captured descriptive elements of being a relative in a cardiac medical intensive care unit. After review with PP, which involved a close review of the coding of a segment of the data set and assessing the overall coding of the data set, the data set was read again and recoded, and codes were added or modified, as necessary, to ensure a consistently coding of the entire data set. Keeping our research focus in mind, potential categories were then identified from the codes, based on patterned responses and clusters of meaning within the set of data. Relevant data were united under each category. Finally, three themes were identified, and the data read again to affirm that the themes formed by the authors captured the participants' views and experiences of being a relative in a cardiac medical intensive care unit.
Over a period of 12 months from the summer of 2016 to the summer of 2017, 137 relatives of hospitalized patients were asked whether they would participate in the study. Patients during the period had mainly cardiogenic shock, were unconscious resuscitated from out-of-hospital cardiac arrest or had life-threatening cardiological disease, e.g. severe endocarditis.
The participants were informed verbally and in writing about the study before they consented. Participation was voluntary, anonymous and without consequences for patients’ care and treatment. The questionnaires were given a consecutive number, relation to the patients' identity or illness was not registered according to current legislation.
Categorical data was given as number and percentage and differences between groups were calculated using chi-square test. All statistical analyzes were calculated in Microsoft Excel version 2013 (Microsoft, Washington, USA).
Of 139 invited, 100 responded (71%). The relatives mainly consisted of close family (98%), of which cohabiting/spouse was the most frequent relation (70%) followed by children (20%) and parents (5%) (Figure 1). The reception at the department was assessed as "very satisfactory" by 86 (86%) and information on the arrival of the relatives at the intensive care unit was predominantly "appropriate" without any difference between doctors and nurses (doctor: 88 (88%), nurse 89 (89%))=0.82)) (Figure 2 a and b), but 5 and 8%, respectively, felt they were given 'too little' information. Upon arrival at the department, 95 (95%) of the relatives knew who to turn to and 95 (95%) experienced "no" or "short wait". A large part of the relatives stated that it has "great" or "very large" importance to be involved in the care (78%). The most frequent activities the relatives participated in were:
There was no significant difference between cohabiting and other relatives' experience of being involved in care. Of the cohabitants 55/70 (79%) responded their involvement in the care was of ‘great’ or ‘very great’ importance; other relatives: 17/25 (68%), p=0.19).
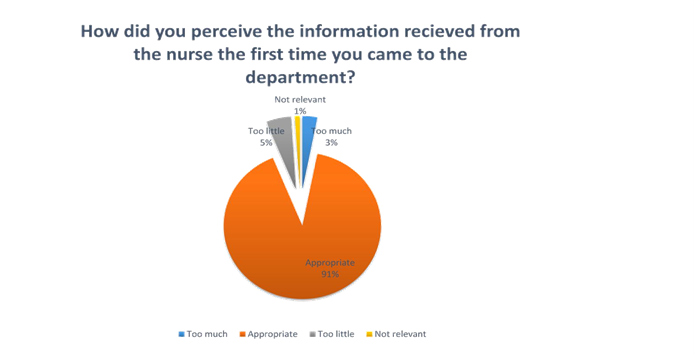
Figure 2 (A) Fraction of responses describing amount of information from nurses or doctors when relatives first arrived in the department.
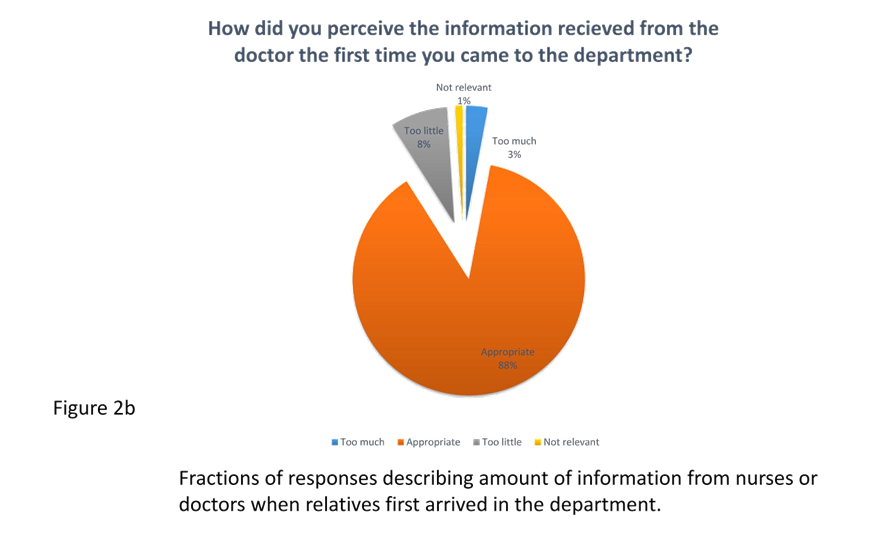
Figure 2 (B) Fraction of responses describing amount of information from nurses or doctors when relatives first arrived in the department.
Thirty-seven (37%) relatives brought children to the department. Of these, 36 (97%) estimated that having children was "good" or "really good" and all 37 experienced that the staff informed the children "well" or "really good".
Thirteen (13%) assessed the department's facilities as "bad" or "really bad" and the most frequent criticism stated in the open questions were small patient suites, limited opportunities for relatives to stay alone in the waiting period and occupied parking lots. However, 71 (71%) responded "well" to the overall impression of the department's premises. Overall, 93 (93%) responded "well" or "very well" to the extent, wishes and needs have been taken into account during your relatives' admission.
The qualitative thematic analysis revealed three themes (see table 1. for an example of the thematic analysis): The first theme, “Thorough and honest information secures quality and hope” in where relatives stated the importance of receiving a thorough information and continuous honest and realistic updates to keep up hope and secure a good quality in the care. One relative state it like this: “It is important to get realistic assessments about the relative's condition, both positive and negative. It is nice that we feel greeted in all the questions we ask about the treatment, even if it is not necessarily current issues - so the feeling of being met in our needs is important”. Or as another relative describes: “it is very important to be able to get explanations. Important with honest information. Total resumes of the hospital stay and are able to follow development in the main data”.
Quotes |
Codes |
Categories |
Themes |
Statements on information from the staff |
What – since last |
Importance of thorough information and |
Thorough and honest information secures |
What has happened since I last visited? |
Status of my relative |
||
Status of my father's health and how the current situation is. |
Update every time |
||
[I would like an] update every time I visits. Whether my relative is |
What happens and why |
||
What happens and why. What does treatment mean, what data is shown |
|||
Statements about the way to inform |
|||
Tell the truth, don’t hold anything back |
Tell the truth |
||
Very important to be able to get explanations. Important with honest information. |
Get explanations |
||
It is important to get realistic assessments about the relative's condition, both positive |
Get realistic assessment |
||
The truth about the patient’s condition. |
The truth |
||
It is important for me that you answer my questions openly and honestly. |
Openly and honestly answers |
||
A realistic assessment of patient’s prognosis. Focus on positive news. |
Focus on positive news |
||
Table 1 Example of the analytical process
Secondly, the theme “Depending on professional help” illustrates the dependence on help from the staff regarding how to cope with the situation and how to act on the ward. Expressed like this: “Help with handling the children, should they come visit? What should I talk to them about? Also guidance on taking care of myself”. And also: “What should I do in the future? What should I do in the patient’s room when I visit, for example”
The third theme “Struggling in unfamiliar and unfriendly setting” reveals how the relatives experience that the physical conditions on the ward causes more stress and almost tend to forget relatives. This is illustrated as follows: “You as a staff member have done the extra things for us to be here and we appreciate that. But the fact that the relatives of a whole department have so small rooms to stay in, is scary. Or that you sit out between the other patients who are going to echocardiography It is as if the relatives are forgotten - we put our trust in the best care that our family member - but the desire to be here also roar when you see the conditions” or “It is disturbing that the ward do not have single rooms. Nursing activity around co-patient cannot be overlooked/heard”.
In this study of 100 relatives of patients in a cardiac medical intensive care unit, we found.
There is a marked knowledge gap about the relatives' psychological condition during an intensive patient's admission and the extent of neuropsychiatric symptoms subsequently. Furthermore, there is currently little evidence of measures that can limit the psychological consequences of relatives of intensive care patients. Smaller international studies have reported that using diaries can reduce post-traumatic stress symptoms in relatives8 and thorough information about the patient's condition9 and support from staff10 has been shown to protect relatives from neuropsychiatric late effects. Furthermore, meetings between staff and relatives with a focus on the difficult conversation11 and the delivery of material about the grief process12 have proved to have a positive impact on the relatives' coping with crisis. This study highlights the influence of the physical conditions and the setting the care is taking place in, in order to prevent negative stress.
Involving relatives in the patient's care and treatment is potentially beneficial to both patient, staff and relatives themselves. The relative has special knowledge of the patient and a special interest in the patient's well-being. These aspects can be utilized in the care so that patients’ needs are met. By involving the next of kin in the care, restlessness, helplessness and frustration of the relative can be prevented for potential benefit to both the staff and the relatives themselves.13 The situation can be further exploited to offer the next of kin conversations with a psychologist or priest who may contribute further to mitigating mental trauma. However, since the relative is not formally a patient in the ward, this type of support may not be offered.5 It is not certain that all relatives are ready to participate in the care and the optimal time to involve the relatives is not known.14
Based on this present study and the available literature in the field, we would recommend involving caregivers in the care of the critically ill heart-intensive patient. The relative should be informed on how best to assist the patient during hospitalization and information on the patient's health status and expected prognosis should be provided openly and honestly. However, when asking relatives to join in on patient care the importance of potentially caregiver burden should be considered. Caregiving burden has been related to a decreased quality of life with mental deterioration, such as depression and anxiety, and increased morbidity as a consequence.15,16 If the patient has children under the age of 18, it seems reasonable for them to visit the patient in the intensive care unit, however there is need for more knowledge in this area in general.
Knowledge exists about children experiencing a parent living through cancer, and both age and illness severity seems to play a role.17 No knowledge exists internationally about children’s experiences with parent’s heart diseases or the caregiver burden of the children.
Future studies should investigate specific actions that can be taken to help relatives, both adults and children of critically ill patients, as well as studies that clarify the extent of neuropsychiatric late sequelae of relatives. The present study is limited by the anonymous, observational design and states only semi-quantitatively how the relatives are affected by the patient's course. The study has been carried out at a specialized cardiological intensive care unit, comprises only Danish-speaking relatives and is not linked to actual intervention, why extrapolation to other disease groups, not Danish-speaking, as well as conclusions on the effect of nursing initiatives that potentially reduce the influence on relatives during the course should be made with caution. The thematic analysis part also contains limitations. Experiences and statements from relatives are written and thereby not open for deeper exploration as would be in for example a face to face interview. To ensure dependability, we sought to be as traceable and documentable in the research process as possible. To secure conformability that is related to the integrity of the findings that are rooted in the data, we presented the process of analysis, quotes, codes, categories and theme that support the findings in an example.
The data material has certain limitations which have to consider when interpreting the data. First, the data collection was so no identification of relatives or patients was possible. Therefore we are unable to link the answers the diagnoses, event or course of the patients’ treatment in the department. As the data collection was anonymized, no approval from the ethics committee or data protection agency was needed
This study provides insight into the relatives' feelings and needs when a patient is admitted to the intensive care unit. It is important for relatives to be involved in the care, and this applies to both partners and related relatives. The relatives felt their wishes and needs were met and there was satisfaction with both the reception at the department and information from both the doctor and the nurse. Future studies should clarify the potential benefits of involving caregivers in the care of the intensive care patient as well as the extent of neuropsychiatric late sequelae in relatives after a patient's intensive hospitalization.
Implications of Clinical practice
HG conceived the idea for the study, constructed the survey, participated in analysis and drafted and approved the final manuscript.
JG participated in analysis and drafted and approved the final manuscript.
JK participated in analysis and drafted and approved the final manuscript.
SN participated in construction of the survey and approved the final manuscript.
PP participated in analysis and drafted and approved the final manuscript.
Danish law waives the use of anonymized survey data from relatives. The ethical committee waives consent for anonymized questionnaire data.
The research was carried out without funding.
The nursing colleagues at Cardiology Intensive Care Unit 2143, Rigshospitalet are acknowledged for support and practical help with the completion of this study.
The authors have no conflicts of interest to declare.

©2019 Glud, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.