eISSN: 2572-8474


Research Article Volume 8 Issue 1
1MSc, Cardiovascular Thoracic Nursing, GGSIPU/ National Heart Institute, India
2Principal, GGSIPU/ National Heart Institute, India
Correspondence: Bhanupriya, MSc, Cardiovascular Thoracic Nursing, GGSIPU/ National Heart Institute, East of Kailash, New Delhi, India
Received: June 11, 2022 | Published: June 25, 2022
Citation: Bhanupriya, Chugh D. COVID impact on pattern of ischemic heart disease in comparable period. Nurse Care Open Acces J. 2022;8(1):37-46. DOI: 10.15406/ncoaj.2022.08.00236
Aim: To compare the impact of COVID-19 on pattern of Ischemic Heart Disease in comparable period by assessing the incidence, severity of symptoms and in-hospital mortality of Ischemic Heart Disease patients before and during COVID-19.
Background: COVID-19 directly or indirectly, affects the cardiovascular system it not only causes myocardial injury but also reduces the incidence and increasing the severity and mortality of Ischemic Heart Disease patients and it was seen that pneumonia and influenza infections increases the risk of acute MI by six folds.
Methods: Data collected from health records of patients admitted in National Heart Institute from Ischemic Heart Disease in comparable four months period of before (Oct 2019-Jan 2020) and during (Oct 2020-Jan 2021)COVID-19 by using a self-structured bio physiological tool. The total samples taken were 421 out of which 237 were before COVID-19 and 184 were during COVID-19. STARD checklist used to report the study.
Results: The major findings of the study reveals that incidence of ischemic heart disease indicates that before COVID-19 incidence was 13.32% whereas the incidence of ischemic heart disease during COVID-19 was 12.69%. This means incidence decreases during COVID-19 as compared to before COVID-19. Severity scores measured before COVID-19 showed the majority of the patient (61.2%) having no severity as compared to during COVID-19 whereas the majority of patients having mild (41.8%) and moderate (1.1%) severity as compared to before COVID-19. Mortality of ischemic heart disease indicates that before COVID-19 in-hospital mortality was 1.28% whereas in-hospital mortality of ischemic heart disease during COVID-19 was 0.54%.
Conclusion: From findings the study interprets that incidence and in-hospital mortality of Ischemic Heart Disease patients decreases during COVID-19 as compared to before COVID-19, whereas the severity of Ischemic Heart Disease symptoms increases during COVID-19 as compared to before COVID-19.
Implication: Patients are staying away from the hospital due to fear of contracting the infection which in return act as a major issue of increasing Ischemic Heart Disease severity so, the nurses should involve in a proactive campaign to alleviate patient concern and encourage them to seek timely medical attention despite the COVID-19 pandemic.
Keywords: COVID-19, pattern of ischemic heart disease, comparable period
COVID-19, corona virus disease 2019; ACS, acute coronary syndrome; IHD, ischemic heart disease; CAD, coronary artery disease; STEMI, ST segment elevation myocardial infarction; NSTEMI, non ST segment elevation myocardial infarction; MI, myocardial infarction
The main text must be clearly paragraphed. State the objectives of the work and provide an adequate background, comprehensive insight on the purpose of the study and its significance, avoiding a detailed literature survey or a summary of the results.
The COVID-19 pandemic is the greatest crisis of our time, claiming more than 2 million lives and causing the biggest shock to the global economy since World War II.1 COVID-19 is a highly contagious new virus caused by SARS-CoV-2. The disease was first identified in December 2019 in Wuhan, Hubei, China.2 The outbreak was declared a Public Health Emergency of International Concern by the World Health Organization (WHO) in January 2020 and was recognized as a pandemic in March 2020.3
COVID-19 primarily affecting the respiratory system but it can also cause acute myocardial injury and chronic damage to the heart.4 some clinical studies reported an association between cardiovascular diseases and COVID-19. The Patients with pre-existing cardiovascular comorbidities increasing the risk of death in patients with COVID-19, whereas COVID-19 can also induce myocardial injury, arrhythmia, acute coronary syndrome, and venous thromboembolism.5
As COVID-19 pandemic has had a huge impact on the global health care system. Across the world, the Government has appealed to people to stay at home and observe social distancing to slow down the pandemic, but this leads to “pseudo-reduction” i.e. the incidence of ACS/STEMI is actually the same, but these patients are staying away from hospitals due to fear of contracting the infection in the hospital setting.6 Some reports also showed that due to COVID-19 pandemic there is significant decline in total acute coronary syndrome, this decrease in hospital admissions and late presentations can be a worrisome sign for an increase in future complications of myocardial infarctions.7
Similarly, according to the American college of emergency physicians, nationwide hospitals are seeing up to 60% reduction in admission for heart attack due to fear in the medical community of the dangerous and potentially fatal effect of COVID-19. These fears are also backed up by a recent study showing a 38% drop in the patient being treated with a life-threatening ST elevated myocardial infarction (STEMI) heart attack.8 And increase in deaths caused by IHD during the initial phase of COVID-19 which raising concern due to the indirect toll on the patient.9
Aim of study
The present study was conducted as an attempt to assess the pattern of Ischemic Heart Diseases in a comparable period of pre and during COVID-19 pandemic in a patient admitted to National Heart Institute, Delhi. With following objectives:
Background
Among patients with Corona virus disease 2019 (COVID-19), coronary artery disease (CAD) has been identified as a high-risk condition. Coronary artery disease (CAD) is the leading cause of death and the most common cardiovascular disease worldwide.10 Similarly; CAD is a prevalent condition among patients with COVID-19, varying between 2.5% and 10% of cases.11 According to the china report CAD has been identified as a risk factor for severe COVID-19 and the case-fatality rate increased from 2.3% to 10.5% in patients with pre-existing cardiovascular disease.12
It is presumable that COVID-19, directly and indirectly, affects the cardiovascular system and the heart in particular. Potential mechanisms of cardiovascular injury have been identified and include direct myocardial injury from hemodynamic derangement or hypoxemia, inflammatory myocarditis, stress cardiomyopathy, micro vascular dysfunction or thrombosis due to hypercoagulability, or systemic inflammation (cytokine storm), which may also destabilize coronary artery plaques. Pneumonia and influenza infections have been associated with a six-fold increased risk of acute MI. Patients with severe COVID-19, such as those with high fever or hypoxia due to lung disease may need a significant increase in cardiac output. Type II myocardial ischemia; therefore, may result in patients with obstructive CAD.13
According to a study conducted to analyse the death rates from ischemic heart disease before and after the onset of the pandemic in the United States and its comparison with those to the same periods the year before and they found a substantial increase in deaths from ischemic heart diseases and hypertensive diseases over that period. Specifically, there was an 11 percent spike in deaths due to ischemic heart diseases, or those related to the narrowing of the arteries, over that time compared with the previous year.14
Another study was conducted in Italy to evaluate the impact of the COVID-19 pandemic on patient admissions to Italian cardiac care units (CCUs). In which they compared admissions for acute MI to coronary care units from March 12th to 19th in 2020 with those during the equivalent week in 2019 and they found that there was a 49.4 percent reduction for both STEMI and NSTEMI. The STEMI case fatality rate was higher, comparing 2020 with 2019.15 A large database study was also conducted in England comparing hospital admissions for acute coronary syndromes (ACS) between mid-February and the end of March 2020 and with the weekly average in 2019 (3017 per week). It shows a substantial reduction in the weekly numbers of patients with ACS admitted to hospitals in England by the end of March 2020 (1813 per week; 40 percent reduction) compared with the 2019 weekly average. The trend was partially reversed by the end of May 2020 (2522 per week; 16 percent reduction). Although the decline in hospital admissions was seen in all types of ACS (e.g. STEMI, NSTEMI, unstable angina, and MI of unknown type), but it was most pronounced for those with NSTEMI.16
There are some reports which show an increased coronary artery thrombus burden in patients with STEMI along with an increased frequency of thrombotic strokes, especially in young people during the COVID-19 pandemic.17 Similarly; according to National Centre for Health Statistics data the death rates from ischemic heart disease and hypertensive disease in the U.S increased after the onset of the pandemic in 2020, compared with changes over the same period in 2019. And there was an increase in deaths due to ischemic heart disease (139%) and hypertensive diseases (164%) during the pandemic.18
Research design: Descriptive-Comparative Research design.
Sample and setting: All the patients of IHD admitted to the National Heart Institute within 4 months period before (Oct 2019-Jan 2020) and during COVID-19(Oct 2020-Jan 2021) were taken as a sample. There were total 421 samples out of which 237 samples were before COVID-19 and 184 samples were during COVID-19.
Inclusion criteria: All the patients who were admitted diagnosed and treated as IHD in the hospital within 4 months of period before and during COVID-19.
Exclusion criteria: Less than 15 years and more than 90 years of age; Patients admitted with non-cardiac conditions; Patients with valvular heart diseases, a congenital heart defect and peripheral arterial diseases
Data collection: Data was collected from the health records of the patients admitted in National Heart Institute from Ischemic Heart Disease in comparable four months period of before (Oct 2019-Jan 2020) and during (Oct 2020-Jan 2021) COVID-19 by using a self-structured bio physiological tool.
Data analysis: The data was analysed by applying descriptive and inferential statistics, data was analyzed in terms of frequencies and percentages. Mean, mean percentage, standard deviation, mean difference and Mann Whitney U test were computed to find the comparison of pre-COVID-19 and during COVID-19 impact on the pattern of Ischemic Heart Disease.
Baseline characteristics such as demographic variables and clinical variables of ihd patients before and during covid-19
This section describes the characteristics of ischemic heart disease patients the samples were drawn from the national heart institute. A total of 421 samples were selected for the study. In Table 1 information on the demographic variables includes age, gender and diagnosis and length of stay in hospital. In Table 2 information on clinical variables of the sample such as heart rate, systolic and diastolic blood pressure Spo2 with or without oxygen and chest pain on admission.The data collected were tabulated and analyzed to obtain the frequency and distribution of ischemic heart disease.
S. No |
Demographic variables |
Before COVID-19 (n=237) |
During COVID-19 (n=184) |
||
f |
% |
f |
% |
||
1 |
Age (in years) |
2 |
0.8 |
2 |
1.1 |
34-43 |
11 |
4.6 |
12 |
6.5 |
|
44-53 |
48 |
20.3 |
24 |
13.1 |
|
54-63 |
88 |
37.1 |
66 |
35.8 |
|
64-73 |
61 |
25.7 |
55 |
29.9 |
|
74-83 |
17 |
7.2 |
20 |
10.9 |
|
Above 84 |
10 |
4.2 |
05 |
2.7 |
|
2 |
Gender |
194 |
81.9 |
138 |
75 |
Female |
43 |
18.1 |
46 |
25 |
|
Table 1 The frequency and percentage distribution of patients according to demographic variables (N=421)
S. No |
Clinical manifestations |
Before COVID-19 (n=237) |
During COVID-19 (n=184) |
||
f |
% |
f |
% |
||
1 |
HR |
03 |
1.3 |
00 |
00 |
51-100 |
205 |
86.5 |
160 |
86.9 |
|
101-150 |
29 |
12.2 |
24 |
13.1 |
|
2 |
SBP |
27 |
11.4 |
12 |
6.5 |
101-150 |
174 |
73.4 |
135 |
73.4 |
|
151-200 |
35 |
14.8 |
35 |
19.1 |
|
More than 200 |
00 |
00 |
01 |
0.5 |
|
Non recordable |
01 |
0.4 |
01 |
0.5 |
|
3 |
DBP |
28 |
11.8 |
13 |
7.1 |
61-80 |
145 |
61.2 |
109 |
59.2 |
|
81-100 |
57 |
24.1 |
57 |
30.9 |
|
101-120 |
06 |
2.5 |
03 |
1.7 |
|
More than 120 |
00 |
00 |
01 |
0.5 |
|
Non recordable |
01 |
0.4 |
01 |
0.5 |
|
4 |
SPO2 With O2 |
|
|
|
|
Less than 90 |
04 |
1.7 |
00 |
00 |
|
Above 90 |
36 |
15.2 |
11 |
5.9 |
|
Not applicable |
197 |
83.1 |
173 |
94.1 |
|
5 |
SPO2 with Room air |
|
|
|
|
Less than 80 |
05 |
2.1 |
01 |
0.5 |
|
81-90 |
13 |
5.5 |
05 |
2.7 |
|
Above 90 |
198 |
83.5 |
172 |
93.5 |
|
Not applicable |
21 |
8.9 |
06 |
3.3 |
|
Table 2 The frequency and percentage distribution of IHD patients according to clinical variables (N=421)
Percentage-wise distribution of ischemic heart disease according to their age depicts that the highest percentage of them (37.1%) before COVID-19 and (35.8%) during COVID-19 were in the age group of 54-63 years and lowest percentage (0.8%) before COVID-19 and (1.1%) during COVID-19 were in the age group of 24-33 years. Hence it can be interpreted that ischemic heart disease mostly affected people with 54-63 years of age group irrespective of COVID-19.
Percentage-wise distribution of ischemic heart disease according to their gender shows that the highest percentage (81.9%) of them before COVID-19 was male and less than half of this percentage (18.1%) was female. Similarly during COVID-19 male shows the highest percentage (75%) and females was less in percentage (25%). Hence it can be interpreted that ischemic heart disease is more prominent in males as compared to females irrespective of COVID-19.
Figure 1 showed the frequency-wise distribution of patients according to their diagnosis indicates that the highest number of patients 96 (40.5%) before COVID-19 and 83 (45.1%) during COVID-19 were diagnosed with CAD. The patient diagnosed with ACS were 39 (21.2%) during COVID-19 and 21(8.9%) before COVID-19, whereas the patient with stable angina were 8(4.3%) during COVID-19 and 21(8.9%) before COVID-19. The patient diagnosed with unstable angina were 38(16.0%) before COVID-19 and 13(7.1%) during COVID-19, patients with NSTEMI were 29(12.2%) before COVID-19 and 17(9.2%) and with STEMI were 31(13.1%) before COVID-19 and 22(12.0%) during COVID-19. Hence it can be interpreted that most of the patients were diagnosed with CAD and ACS during COVID-19 and with CAD and unstable angina before COVID-19. CAD was more prominent both during and before the COVID-19 pandemic.
Figure 2 showed that patients were hospitalized for less than 7 days (92.4%) and more than 16 days (0.5%) during COVID-19 whereas patients were hospitalized for 8-16 days (8%) before COVID-19. Hence it was interpreted that some patients were hospitalized for more than 16 days during COVID-19.
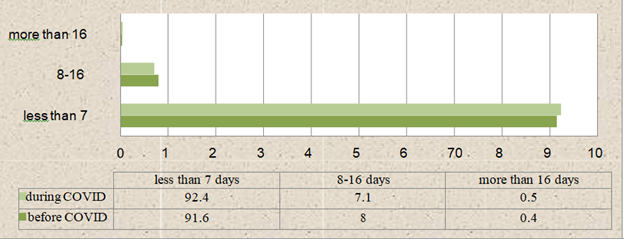
Figure 2 A bar diagram shows the percentage distribution of IHD patients with regards to the duration of hospitalization.
Percentage-wise distribution of ischemic heart disease according to clinical manifestations on admission shows that the highest number of patients in both during COVID-19 (86.5%) and before COVID-19 (86.9%) was having heart rate between 51- 100 beats /min and very less number of patients were having heart rate less than 50 beats/min before COVID-19 (1.3%) but during COVID-19 not a single patient was having heart rate less than 50 beats/min and (12.2%) patient before COVID-19, (13.1%) were having heart between 101-150 beats/min. Hence it was interpreted that most of the patients were having a heart rate of 51-100 beats/min both before and during COVID-19.
Percentage-wise distribution of systolic blood pressure ranges between 101-150 was in more number of patient irrespective of COVID-19 but systolic blood pressure ranges between 151-200 and more than 200 is more during the time of COVID-19 was (19.1%) (0.5%) respectively and that of before COVID-19 was (14.8%) (0.0%) respectively and it was shown that (11.4%) before COVID-19 and (6.5%) during COVID-19 were having systolic BP ≤100. Hence it was interpreted that number patients were having systolic BP range between 101-150 irrespective of COVID-19.
Similarly, diastolic blood pressure ranges between 61-80 was in more number patients irrespective of COVID-19, diastolic blood pressure ranges between 81-100 was (24.1%) before COVID-19 and (30.9%) during COVID-19. Diastolic blood pressure between 101-120 was (2.5%) before COVID-19 and (1.7%) during COVID-19 and (11.8%) before COVID-19 and (7.1%) during COVID-19 were having diastolic blood pressure <60 and it was shown that during COVID-19 (0.5%) were having diastolic blood pressure more than 120 and none of the patients was having diastolic blood pressure more than 120 before COVID-19. Hence it was interpreted that more patients were having diastolic blood pressure between 61-80 irrespective of COVID-19.
Percentage-wise distribution of SpO2 with O2 showed that less than 90 it was (1.7%) before COVID-19 and none of the patients having SpO2 less than 90 during COVID-19 and (15.2%) before COVID-19 and (5.9%) during COVID-19 were having SpO2 above 90. Similarly, (2.1%) before COVID-19 and (0.5%) during COVID-19 were having SpO2 with room air less than 80, (5.5%) before COVID-19 and (2.7%) during COVID-19 were having SpO2 with room air between 81-90 and (83.5%) before COVID-19 and (93.5%) during COVID-19 were having SpO2 with room air above 90. Hence it was interpreted that more patients were having SpO2 with oxygen and with room air above 90 irrespective of COVID-19.
Figure 3 showed the frequency distribution of patients according to chest pain indicates that the highest number of patients were having chest pain 205 (86.5%) before COVID-19 and 167 (90.8%) during COVID-19 and very less number of patients were not having chest pain before 32(13.5%) and during COVID-19 17(9.2%).
Comparison of incidence of ihd patients before and during covid-19
This section describes the incidence of ischemic heart disease before and during COVID-19. The samples were drawn from the national heart institute. It was analyzed by using a formula: Incidence = IHD admission/total hospital admission *100 H1- There will be a significant difference in the mean incidence of Ischemic Heart Disease before and during COVID-19.
Table 3 showed the month-wise incidence of ischemic heart disease indicates that there was the highest incidence of cases admitted in Jan before COVID-19 60(14.88%) and during COVID-19 52(15.90%). The lowest incidence of cases before COVID-19 was in Dec 52 (11.65%) whereas it was in Nov 40 (9.59%) during COVID-19.
Month |
Before COVID-19 |
During COVID-19 |
||||
Total admission in hospital |
Admission with ischemic heart disease |
Incidence |
Total admission in hospital |
Admission with ischemic heart disease |
Incidence |
|
Oct |
452 |
67 |
14.82% |
372 |
41 |
11.02% |
Nov |
478 |
58 |
12.13% |
417 |
40 |
9.59% |
Dec |
446 |
52 |
11.65% |
383 |
51 |
13.31% |
Jan |
403 |
60 |
14.88% |
327 |
52 |
15.90% |
Table 3 The month-wise distribution and incidence of ischemic heart disease patients before and during COVID-19 (N=421)
Figure 4 showed the Overall incidence of ischemic heart disease indicates that before COVID-19 incidence was 13.32% whereas the incidence of ischemic heart disease during COVID-19 was 12.69%. Hence it was interpreted that the overall in-hospital incidence of ischemic heart disease decreases during COVID-19 as compared to before COVID-19.
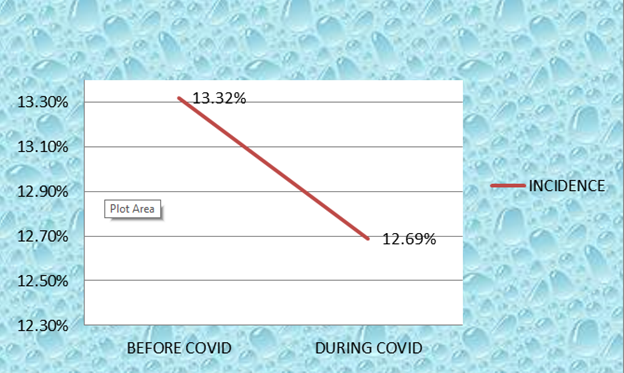
Figure 4 A line diagram shows the overall incidence of ischemic heart disease before and during COVID-19.
Table 4 The data presented in the table shows that the mean rank of incidence of IHD before COVID-19 was higher at 6.375 than the mean rank of incidence during COVID-19 2.625, the obtained Mann Whitney U value was 0.5 with a p-value of 0.015. Hence, null hypothesis HO1 is rejected and research hypothesis H1 is accepted indicating that there was a significant difference in the incidence of ischemic heart disease before and during COVID-19. This shows that more cases were seen before COVID-19 as compared to during COVID-19.
Group |
N |
Mean Rank |
Sum of Ranks |
Mann-Whitney U |
“p’ Value |
Before COVID-19 |
237 |
6.375 |
25.5 |
0.5 |
0.015* |
During COVID-19 |
184 |
2.625 |
10.5 |
Table 4 Comparison of incidence of ischemic heart disease before and during COVID-19 using Mann Whitney U test
Level of significance 0.05 *significant **non-significant
Assessment of severity of symptoms before and during covid-19
This section describes the frequency and percentage of clinical parameters showing the severity of ischemic heart disease before and during COVID-19.
Table 5 represents the severity of cardiac and inflammatory biomarkers which shows that troponin was positive in more patients before COVID-19 (29.1%) as compared to during COVID- 19 (27.2%). CK-MB >24 IU/L was also more before COVID-19 (28.3%) as compared to during COVID-19 (24.5%). Pro-BNP < 300Pg/ml and > 300Pg/ml was more during time of COVID-19 (2.7%) (14.7%) as compared to before COVID-19 (2.1%) (11.8%) respectively. CRP <6mg/l and >6mg/l was also more during COVID-19 pandemic (1.6%) (1.1%) as compared to before COVID-19. D-dimer <0.5µg/ml and >0.5µg/ml were also more during the COVID-19 pandemic (2.2%) (4.9%) respectively whereas none of the patients had undergone D-dimer before COVID-19.
S. No |
Cardiac and inflammatory biomarkers |
Before COVID-19 |
During COVID-19 |
||
f |
% |
f |
% |
||
1 |
Troponin |
69 |
29.1 |
50 |
27.2 |
Negative |
48 |
20.3 |
49 |
26.6 |
|
Not done |
120 |
50.6 |
85 |
46.2 |
|
2 |
CK-MB |
48 |
20.2 |
37 |
20.1 |
>24 IU/L |
67 |
28.3 |
45 |
24.5 |
|
Not done |
122 |
51.5 |
102 |
55.4 |
|
3 |
Pro-BNP |
05 |
2.1 |
05 |
2.7 |
>300 pg/ml |
28 |
11.8 |
27 |
14.7 |
|
Not done |
204 |
86.1 |
152 |
82.6 |
|
4 |
CRP |
01 |
0.4 |
03 |
1.6 |
|
>6 mg/l |
00 |
00 |
02 |
1.1 |
|
Not done |
236 |
99.6 |
179 |
97.3 |
5 |
D-DIMER |
00 |
00 |
04 |
2.2 |
|
>0.5 µg/ml |
00 |
00 |
09 |
4.9 |
|
Not done |
237 |
100.0 |
171 |
92.9 |
Table 5 The frequency and percentage distribution of cardiac and inflammatory biomarkers of IHD patients (N=421)
Hence it was interpreted that most of the patients having deranged values during COVID-19 as compared to before COVID-19 except troponin and CK-MB.
Table 6 represents the frequency and percentage of ECG severity which shows that ST Wave changes were seen more during the time of COVID-19 (56.5%) as compared to before COVID-19 (48.5%) whereas T wave changes were seen more before COVID-19 (65%) as compared to during COVID-19 (54.9%) and Arrhythmias more frequently COVID-19 (22.8%) as compared to before COVID-19 (21.1%). Hence it was interpreted that ST wave changes and arrhythmias are more commonly seen in patients during COVID-19.
S. No |
Clinical variables |
Before COVID-19 (n=237) |
During COVID-19 (n=184) |
||
f |
% |
f |
% |
||
1
|
ST Wave |
|
|
|
|
No change |
121 |
51.1 |
80 |
43.5 |
|
Elevation/depression |
115 |
48.5 |
104 |
56.5 |
|
Not done |
01 |
0.4 |
00 |
00 |
|
2 |
T Wave |
|
|
|
|
|
No change |
82 |
34.6 |
83 |
45.1 |
|
Elevation/ Depression |
154 |
65.0 |
101 |
54.9 |
|
Not done |
01 |
0.4 |
00 |
00 |
3 |
Arrhythmias |
|
|
|
|
|
Yes |
50 |
21.1 |
42 |
22.8 |
|
No |
186 |
78.5 |
142 |
77.2 |
|
Not done |
01 |
0.4 |
00 |
00 |
Table 6 The frequency and percentage distribution of IHD patients according to ECG (N=421)
Figure 5 showed the frequency of ECHO Severity which shows that RWMA presents more before COVID-19 (27.4%). EF between 55-70%(37%) and 35-39%(10.3%) was more during COVID-19 whereas EF between 40-54%(39.7%) and <35%(5.5%) was more before COVID-19. MR in the trace (65.2%) and severe (1.1%) category was more during COVID-19 whereas it was more in mild (17.7%) and moderate (4.6%) category before COVID-19. PAH was present in more patients during COVID-19 (77.2%) as compared to before COVID-19 (11.8%). Hence it was interpreted that severity of ECHO increases during COVID-19 as compared to before COVID-19.
Figure 6 showed the percentage-wise distribution of CAG indicates that CAG was performed in the highest percentage of the patient during COVID-19 (90.8%) as well as before COVID-19 (83.5%). Hence it was interpreted that CAG was more often done in patients with ischemic heart disease.

Figure 5 A line diagram shows the frequency distribution of IHD patients before and during COVID-19 with regards to ECHO.
Table 7 represents the frequency and percentage of other investigations severity which shows that CAG was done in more patients during COVID-19 (90.8%). Hb <13 or >17 gm/dl was more before COVID-19 (44.7%). ESR >22 mm/1hr was more during COVID-19 (13.6%). HbA1c >5.7 was more during COVID-19 (13.6%). PT/INR >14.9/>1.8 was more during COVID-19 (10.3%). SGOT <17 U/L was more before COVID-19 (1.7%) whereas >59U/L was more during COVID-19 (17.9%). SGPT <21U/L was more during COVID-19 (17.9%) whereas >72U/L was more before COVID-19 (8.1%). Sr. Creatinine>1.3mg/dl was more during COVID-19 (75.5%). Sr. Urea <19 mg/dl (15.8%) and >43mg/dl (15.2%) was more during COVID-19. Sr. Sodium <135 or >145 mmol/l was more before COVID-19 (34.2%). Sr. Potassium <3.5 or >5.1 mmol/l was more during COVID-19 (12.5%). Sr. Calcium <8.6 or >10.3mg/dl was more during COVID- 19 (10.3%). random blood sugar <80 or>140mg/dl was more during COVID-19 (49.5%). Hence it can be interpreted that ESR, HbA1c, PT/INR, SGOT, SGPT, Sr. Creatinine, Sr. Urea, Sr. Potassium, Sr. Calcium and random blood sugar were more severe during COVID-19 as compared to before COVID-19.
S. No |
Blood Investigations |
Before COVID-19 (n=237) |
During COVID-19 (n=184) |
||
f |
% |
f |
% |
||
1 |
HB |
|
|
|
|
13-17 gm/dl |
130 |
54.9 |
104 |
56.5 |
|
<13 or >17 gm/dl |
106 |
44.7 |
78 |
42.4 |
|
Not done |
01 |
0.4 |
02 |
1.1 |
|
2 |
ESR |
|
|
|
|
0-22 mm/1hr |
127 |
53.6 |
76 |
41.3 |
|
>22 mm/1hr |
26 |
11.0 |
25 |
13.6 |
|
Not done |
84 |
35.4 |
83 |
45.1 |
|
3 |
HbA1C |
|
|
|
|
|
4.5-5.7 |
10 |
4.2 |
07 |
3.8 |
|
>5.7 |
72 |
30.4 |
63 |
34.2 |
|
Not done |
155 |
65.4 |
114 |
61.9 |
4 |
PT/INR |
|
|
|
|
|
9.8-14.9sec/0.8-1.8 |
193 |
81.4 |
157 |
85.3 |
|
>14.9/>1.8 |
23 |
9.7 |
19 |
10.3 |
|
Not done |
21 |
8.9 |
08 |
4.3 |
5 |
SGOT |
|
|
|
|
|
<17 U/L |
04 |
1.7 |
01 |
0.5 |
|
17-59 U/L |
120 |
50.6 |
96 |
52.3 |
|
>59 U/L |
39 |
16.5 |
33 |
17.9 |
|
Not done |
74 |
31.2 |
54 |
29.3 |
6 |
SGPT |
|
|
|
|
|
<21 |
28 |
11.8 |
33 |
17.9 |
|
21-72 U/L |
116 |
48.9 |
87 |
47.3 |
|
>72 U/L |
19 |
8.1 |
10 |
5.5 |
|
Not done |
74 |
31.2 |
54 |
29.3 |
7 |
Sr. Creatinine |
|
|
|
|
|
0.7-1.3 mg/dl |
212 |
89.5 |
21 |
11.4 |
|
>1.3 mg/dl |
20 |
8.4 |
139 |
75.5 |
|
Not done |
05 |
2.1 |
22 |
11.9 |
8 |
Sr.Urea |
|
|
|
|
|
<19 |
24 |
10.1 |
29 |
15.8 |
|
19-43 mg/dl |
186 |
78.5 |
125 |
67.9 |
|
>43 mg/dl |
22 |
9.3 |
28 |
15.2 |
|
Not done |
05 |
2.1 |
02 |
1.1 |
9 |
Sr.Sodium |
|
|
|
|
|
135-145 mmol/l |
153 |
64.6 |
143 |
77.7 |
|
<135 or >145mmol/l |
81 |
34.2 |
38 |
20.7 |
|
Not done |
03 |
1.3 |
03 |
1.6 |
10 |
Sr.Pottasium |
|
|
|
|
|
3.5-5.1 mmol/l |
219 |
92.4 |
158 |
85.9 |
|
<3.5 or >5.1mmol/l |
15 |
6.3 |
23 |
12.5 |
|
Not done |
03 |
1.3 |
03 |
1.6 |
11 |
Sr.Calcium |
|
|
|
|
|
8.6-10.3 mg/dl |
17 |
7.2 |
03 |
1.6 |
|
<8.6 or >10.3 mg/dl |
05 |
2.1 |
19 |
10.3 |
|
Not done |
215 |
90.7 |
162 |
88.1 |
12 |
Random Blood sugar(RBS) |
|
|
|
|
|
80-140 mg/dl |
119 |
50.2 |
88 |
47.8 |
|
<80 or >140 mg/dl |
113 |
47.7 |
91 |
49.5 |
|
Not done |
05 |
2.1 |
05 |
2.7 |
Table 7 The frequency and percentage distribution of IHD patients according to blood investigations (N=421)
Table 8 represents that Deaths due to IHD in the hospital were present in 1.3% of patients before COVID-19 and 0.5% patients during COVID-19.23.6% of patients were intubated before COVID-19 whereas 28.8% patients were intubated during COVID-19. NIV was used in 2.5% of patients before COVID-19 and 2.2% patients during COVID-19. It was also showed that 8.9% of patients were readmitted before COVID-19 and 8.2% of patients were readmitted during COVID- 19.
S. No |
Other parameters |
Before COVID-19 (n=237) |
During COVID-19 (n=184) |
||
f |
% |
f |
% |
||
1 |
Death |
|
|
|
|
Yes |
03 |
1.3 |
1 |
0.5 |
|
No |
234 |
98.7 |
183 |
99.5 |
|
2 |
Intubation |
|
|
|
|
Yes |
56 |
23.6 |
53 |
28.8 |
|
No |
181 |
76.4 |
131 |
71.2 |
|
3 |
Non-invasive ventilation |
|
|
|
|
Yes |
06 |
2.5 |
04 |
2.2 |
|
No |
231 |
97.5 |
180 |
97.8 |
|
4 |
Readmission |
|
|
|
|
Yes |
21 |
8.9 |
15 |
8.2 |
|
No |
216 |
91.1 |
169 |
91.8 |
|
Table 8 The frequency and percentage distribution of IHD patients according to other severity parameters (N=421)
Figure 7 showed the percentage-wise distribution of patients according to therapeutic management indicates that 21.9% of patients were undergone CABG before COVID-19 whereas 27.2% of patients had undergone CABG during COVID-19. PTCA was done in 27.4% of patients before COVID-19 and 36.4% patients during COVID-19 whereas thrombolysis was done in 2.5% patients before COVID-19 and in 5.4% patients during COVID-19. Medical optimization was done in 38.8% of patients before COVID-19 and in 24.5% of patients during COVID-19. Hence it was interpreted that CABG, PTCA and thrombolysis was done more often during COVID-19 whereas most of the patients were treated with medical optimization before COVID-19.
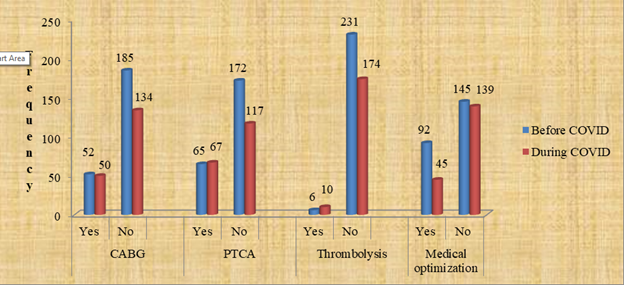
Figure 7 A bar diagram shows the percentage distribution of IHD patients with regards to therapeutic management.
Comparison of severity of symptoms before and during covid-19
This section describes the comparison of the severity of symptoms of ischemic heart disease scores before and during COVID-19. The score was obtained from the bio physiological tool on Ischemic heart disease having a maximum score of 39. Severity was interpreted in terms of severe with the scores of more than 30 moderate with the scores of 20-29 mild with the scores of 10-19 and no severity with a score less than 9 and this section also shows the comparison of severity before and during COVID-19. The data were analyzed to obtain the mean, standard deviation, mean percentage, and Mann-Whitney U test. H2: There will be a significant difference in the mean severity of ischemic heart disease patients before and during COVID-19.
Table 9 Severity scores measured before COVID-19 showed the majority of the patient (61.2%) having no severity as compared to during COVID-19 whereas the majority of patients having mild (41.8%) and moderate (1.1%) severity as compared to before COVID-19. Hence it was interpreted that severity increases during COVID-19 as compared to before COVID-19.
S.No |
Severity of IHD |
SCORE |
Before COVID-19 (n=237) |
During COVID-19 (n=184) |
||
f |
% |
f |
% |
|||
1 |
No severity |
0-9 |
145 |
61.2 |
105 |
57.1 |
2 |
Mild |
10-19 |
91 |
38.4 |
77 |
41.8 |
3 |
Moderate |
20-29 |
01 |
0.4 |
02 |
1.1 |
4 |
Severe |
30-39 |
00 |
00 |
00 |
00 |
Table 9 Comparison of severity scores among IHD patients before and during COVID-19 (N=421)
Table 10 Mean, standard deviation, and mean percentage of before and during COVID-19 severity scores of patients with ischemic heart disease reveals that overall severity during COVID-19 mean score was 9.5163±3.9 which is 24.40% whereas in severity before COVID-19 mean score was 8.5527±3.7 which is 21.93% of the total score. However, the median of severity during COVID-19 was 9 with the range of 2-30 and the median of severity during COVID-19 was 8 with the range of 2-20 of the total score.
Severity |
N |
Range |
Mean |
Median |
Mode |
SEM |
Std. deviation |
Mean % |
During COVID- 19 |
184 |
2-30 |
9.5163 |
9.0 |
8.0 |
0.294 |
3.9 |
24.40% |
Before COVID- 19 |
237 |
2-20 |
8.5527 |
8.0 |
5.0 |
0.242 |
3.7 |
21.93% |
Table 10 Mean, standard deviation, mean percentage of the severity of IHD symptoms before and during COVID-19
Table 11 the data presented in the table shows that the mean rank of the severity of IHD during COVID-19 227.39 was higher than the mean rank of severity before COVID-198.27 with the sum of ranks 41840.00 and 46991.00 respectively. The obtained Mann Whitney U value was 1.879 with a p value 0.015 significant at 0.05 levels in between before and during COVID-19. Hence, null hypothesis HO2 is rejected and research hypothesis H2 is accepted indicating that there was a significant difference in the severity of ischemic heart disease before and during COVID-19. This shows that severity increases during COVID-19 as compared to before COVID-19.
Severity |
N |
Mean Rank |
Sum of Ranks |
Mann Whitney U |
“p’ Value |
Before COVID-19 |
237 |
198.27 |
46991.00 |
1.879 |
0.015* |
During COVID-19 |
184 |
227.39 |
41840.00 |
Table 11 Comparison of before COVID-19 and during COVID-19 severity of ischemic heart disease patient using Mann Whitney U test
Level of significance 0.05 *significant **non-significant
Comparison of in-hospital mortality of ihd patients before and during covid-19
This section describes the in-hospital mortality of ischemic heart disease before and during COVID-19. The samples were drawn from the national heart institute. It was analyzed by using a formula:
Mortality = total no. of deaths due to IHD*100 /total discharge of IHD patients
H3- There will be a significant difference in mean mortality of Ischemic Heart Disease before and during COVID-19.
Table 12 & 13 showed the month-wise mortality of ischemic heart disease indicates that there were more number patients were died only in Oct before (5%) and during COVID-19 (3.03%). And it was more before COVID-19 as compared to during COVID-19.
Month |
Before COVID-19 |
During COVID-19 |
||||
Total no. Of deaths |
Total discharge |
In-hospital Mortality |
Total no. Of deaths |
Total discharge |
In-hospital Mortality |
|
Oct |
3 |
60 |
5% |
1 |
33 |
3.03% |
Nov |
0 |
55 |
0% |
0 |
42 |
0% |
Dec |
0 |
55 |
0% |
0 |
54 |
0% |
Jan |
0 |
64 |
0% |
0 |
54 |
0% |
Table 12 Month-wise distribution and in-hospital mortality of IHD patients before and during COVID-19 (N=421)
Group |
N |
Mean Rank |
Sum of Ranks |
Mann-Whitney U |
‘p’ Value |
Before COVID-19 |
237 |
4.625 |
18.5 |
7.5 |
0.14** |
During COVID-19 |
184 |
4.375 |
17.5 |
Table 13 Comparison of in-hospital mortality of ischemic heart disease before and during COVID-19 using Mann Whitney U test
Level of significance 0.05 *significant **non-significant
Figure 8 showed the Overall mortality of ischemic heart disease indicates that before COVID-19 in-hospital mortality was 1.28% whereas in-hospital mortality of ischemic heart disease during COVID-19 was 0.54%. Hence it was interpreted that the overall in-hospital mortality of ischemic heart disease decreases during COVID-19 as compared to before COVID- 19.

Figure 8 A line diagram shows the overall mortality of ischemic heart disease before and during COVID-19.
The data presented in the table shows that the mean rank of mortality of IHD before COVID-19 was higher at 4.625 than the mean rank of mortality during COVID-19 4.375, the obtained Mann Whitney U value was 7.5 with a p-value of 0.14. Hence, null hypothesis H03 is accepted and research hypothesis H3 is rejected indicating that there was a non-significant difference in mortality of ischemic heart disease before and during COVID-19. This shows that in- hospital mortality decreases during COVID-19 as compared to before COVID-19.
Currently, COVID-19 is a threat to global health. Various researches show that COVID-19 can cause cardiovascular disorders, including myocardial injury, arrhythmias, acute coronary syndrome and venous thromboembolism. Hence it is important to know the impact of COVID-19 on the pattern of ischemic heart disease like the incidence of IHD, severity, and duration of hospitalization of IHD patients during COVID-19, and mortality of IHD patients during COVID19 so that measures can be taken to reduce the impact of COVID-19 on the pattern of ischemic heart diseases.
Study limitations
The limitations of the study were:
Comparison with similar studies
The findings of the present study reveal that the in-hospital incidence of IHD patients during COVID-19 (in 2020) decreases as compared with before COVID-19 (the same period in 2019). It also reveals that there was a significant difference (p=0.015) in the mean incidence of IHD before and during COVID-19.
The finding is consistent with the previous study which shows that weekly rates of hospitalization decreased by 48% during COVID-19. 19 Yet another study shows a drop by 17.8% (p= 0.152) of total STEMI cases during the COVID-19 pandemic.7
The finding of the present study reveals that severity of IHD increases during COVID-19 with a mean score of 9.5163±3.9 as compared to before COVID-19 with a mean score of 8.5527±3.7. It also shows a significant difference (p=0.015) in the mean of severity before and during COVID-19.
This finding was supported by another study that suggests many patients with mild or anginal equivalent symptoms are likely staying at home and waiting longer before presenting to the hospital. Hence severity increases during COVID-19.
The findings of the present study reveal that the in-hospital mortality of IHD patients during COVID-19 decreases as compared to before COVID-19 in the comparable period. It also shows a non-significant difference (p=0.14) in the mean in-hospital mortality of IHD patients before and during COVID-19
These findings are in congruence with the previously conducted study that reveals that there was a concurrent reduction of in-hospital mortality of cardiovascular diseases during lockdown (during COVID-19) and there was a significant increase in out-of-hospital mortality, during the lockdown.20
The present study assessed the pattern of ischemic heart disease i.e. incidence, the severity of symptoms, duration of hospitalization, and in-hospital mortality during and before the COVID-19 pandemic. The finding shows that:
The results revealed that COVID-19 has an indirect impact on the pattern of ischemic heart disease as due to lockdown less or very few numbers of patients were going to hospital as they have fear of contracting with COVID-19 patients which will lead to a reduction in the incidence of IHD on the same side the patients ignoring their symptoms and stay at home for longer period which leads to increase in severity and they present clinical picture showing severe symptoms of IHD similarly, in-hospital mortality of IHD is also decreased during COVID-19 as all concern is shifted to the surge of COVID-19 but some researches indicated that out hospital mortality increases during COVID-19 as patients are not going to the hospital for proper treatment which makes their life in danger.
We are thankful to National Heart Institute for providing the facility to conduct research in the institute and Mrs. Divya Tomar (co-guide, NHI) for her continuous guidance throughout the study.
No conflict of interest has been declared by the author.

©2022 Bhanupriya,, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.