eISSN: 2572-8474


Research Article Volume 8 Issue 2
Health Sciences Department of Nursing, Salale University, Ethiopia
Correspondence: Mengistu Benayew, Health Sciences Department of Nursing, Salale University
Received: October 01, 2022 | Published: October 12, 2022
Citation: Benayew M. Barriers and factors associated with pressure injury prevention practice among nurses working in northern oromia government hospitals in Ethiopia: a cross sectional study design, 2019. Nurse Care Open Acces J. 2022;8(2):65-70. DOI: 10.15406/ncoaj.2022.08.00240
Objective: This study assessed nurses’ pressure injury prevention practices, barriers and associated Factors at Northern Oromia Hospitals in Ethiopia 2019.
Background: Pressure injuries occur in patients both in acute and chronic care settings and place a considerable burden on patients, caregivers, and the health-care system. Pressure injuries are one of the most costly and physically incapacitating problems, contributing to disability and death by prolonging the time of illness, recovery, and hospitalization.
Methods: Hospital based cross-sectional study was done among 215 nurses in North Shewa Zone Hospitals in Oromia Region, Ethiopia from January 1, 2019 to February 30, 2019. Epi data version 3.1 was used to enter data, which was then exported to SPSS version 25 for analysis. Significant determinants for nurses' pressure injury prevention practice were identified using bivariable and multivariable logistic regression.
Results: 215 nurses, out of 230 study participants were responded to the questionnaires making 93.5% response rate. The magnitude of nurses’ pressure injury prevention practice was found to be 43.7% and level of education, AOR 2.075 (95% CI, 1.143-3.765), knowledge, AOR 2.484 (95% CI, 1.303-4.737), training, AOR 2.498 (95% CI, 1.342-4.648), Nurses to patients ratio, AOR 2.306 (95% CI, 1.242-4.281), work experience AOR 1.842 (1.00-3.394) and satisfaction with nursing leadership, AOR 2.395 (95% CL, 1.259-4.554) were determinants of pressure injury prevention practice. Lack of institutional policy and presences of other priorities other than pressure injury were the common barriers for implementing pressure injury prevention practice.
Conclusions: In this study the majority of nurses had poor practice towards pressure injury prevention. Education, knowledge, training, Nurses to patients ratio, work experience and satisfaction with nursing leadership were factors affecting pressure injury prevention practice of nurses.
Recommendations: Implementing strategies that improve pressure injury knowledge, providing on job training, increased educational levels, allocating appropriate nurse-to-patient ratios and encouraging nursing leadership help to improve nurses’ pressure injury prevention practice.
Keywords: pressure injury, prevention, practice, nurses, factors
PI, pressure injury; PIP, pressure injury prevention; NPIAP, national pressure injury advisory panel
Pressure injuries are lesion or injury to the skin or underlying tissues resulting from unrelieved pressure, shear, friction, or a combination of all these. These lesions usually occurred over a bony prominence and may result in tissue death.1 The consequences of pressure-induced skin damage range from non- blanchable erythema on intact skin to open ulcers extended to bone tissues.2 Pressure injures occur in all healthcare settings, with the highest incidence in hospitals and varying by area such as intensive care units, medical wards, and surgical wards.3,4 Pressure injuries are a largely preventable patient safety problem if appropriate interventions are implemented early and are considered indicators of quality of care and patient safety in healthcare. However, pressure injuries remain a serious and potentially life-threatening problem in all healthcare facilities worldwide that continue to cause discomfort, reduces quality of life, increases risk of infection, prolongs illness and hospitalization, increases workload and consumption of hospital resources, and can even lead to disability and death.5–7 According to the 2017 NPUAP report, showed that nearly 2.5 million patients developed pressure related skin injury and 60,000 deaths were occurred each year. Pressure ulcers are a common and devastating complication in hospitalized patients in Africa. It affects 13.84% of his patients in Nigeria and 16.8% in Ethiopia.8,9 Healthcare costs for patients with pressure ulcers ranges from $750 million to greater than $1 billion.10 A pressure injury risk assessment can help identify patients at increased risk of developing a pressure ulcer and guide the best actions to prevent pressure ulcer formation.11 Treatment and prevention of pressure injuries require a multidisciplinary team with a holistic therapeutic approach. Nursing staff, in particular, play a key role in maintaining skin integrity and avoiding complications of pressure injuries, using a variety of preventive methods.12 People with prolonged immobility, limited ability to change positions, sedation from trauma or surgery, peripheral vascular diseases, diabetic mellitus, under nutritional, incontinency, impaired sensation are mainly at risk of developing pressure injury.13–15 Various support surfaces, repositioning, mobilization, skin care, and nutritional supplementation are among the interventional treatments meant to avoid the development of pressure injuries.16 Studies in Ethiopia revealed inadequate pressure injury prevention practice ranging from 17.2%-67.3%17 and heavy work load, training, patient’s condition, lack of pressure ulcer related knowledge, clinical experience, education, availability of equipment and guidelines, and level of satisfaction with nursing leadership style were factors affecting nurses’ pressure injury prevention practice.17–19 Therefore, this study was conducted to assess nurses’ pressure injuries prevention practice and related factors in the study area.
Study design and setting
Hospital based cross-sectional study was conducted from January 1 to February 30, 2020 at North Shewa Zone government hospitals. North Shewa Zone is one of the zones of Oromia regional states in Ethiopia, located at 112 kilometers from the capital city, Addis Ababa. Five government hospitals are there in this Zone with a total of 547 health care professionals. Of which, 230 were nurses.
Study participants
The source and study population were all nurses working in the five government hospitals of North Shewa Zone in Oromia Region, Ethiopia, 2020. All of these nurses were included in the study.
Study variables
The dependent variable was nurses’ pressure injuries prevention practice. The independent variables were socio-demographic factors (age, sex, educational level, and working experience); Institutional related factors (presence of guide line, equipment, training, clinical practice area/ward, work load, nursing leadership,) and Nurse related factors (knowledge).
Data collection tools
Data regarding Socio-demographic factors, institutional, and nurse related factors were collected with self-administered structured questionnaire adopted from different kinds of literatures (10.16.21.22). The outcome variable was measured with 11 practices item questions on three point Likert scale (always, sometimes, never). Knowledge was assessed by 12 yes or no item questions.
Data collectors and procedures
The investigator nominated four BSC nurses working in health centers and trained them about the objective of the study and way of data collection. After a written informed consent was taken, data were collected with self-administered questionnaires and supervised by the investigator.
Sample size determination
Due to the small numbers of source population, the study included all of the nurses working in the five government hospitals in North Showa Zone.
Operational definition
Pressure injury prevention practice: is the expressed practice of nurses towards all preventive activities for pressure injury prevention among hospitalized patients and measured with 11 practices questions and based on the mean of the practice questions it was classified as good if participants scored the mean and above and poor practice if scored less than the mean score.
Pressure injury prevention Knowledge: is the awareness of nurses towards pressure injury prevention. It was assessed by 12 yes/no item questions and classified in to two as good and poor knowledge based on the mean score of knowledge questions.
Nurses, who scored the mean score of the knowledge and above were considered as having good knowledge of pressure injury prevention and those who scored below the mean were considered as having poor knowledge of pressure injury prevention.
Data quality control
Four BSc degree nurses for data collectors were recruited and one day training was given for data collectors. Pretest was conducted in 5% of sample size in Chancho hospital before the actual data collection to clear any ambiguity, confusions, difficult words and differences in understanding.
Data analysis
The data were checked for completeness, coded and entered into Epi Data Version 3.1 then exported into SPSS version 25 for analysis. Descriptive statistics such as text, graphs and tables were used to present data. Model fitness and multicollinearity were checked using Hosmer-Lemeshow goodness of fit test and variance inflation factor (VIF). Those independent variables which had a p-value of ≤ 0.25 during binary logistic regression analysis were entered into multivariable logistic regression analysis. Then AOR with 95% CI and p-value < 0.05 were used to identify factors significantly associated with nurses' pressure ulcer prevention practice.
Ethical approval statement
Ethical approval letter was taken from the Institutional Review Board (IRB) of Salale University after approval of the proposal. Then permission letter from Salale University research and publication directorate was written to each study hospital. Data collection was performed after written voluntary consent is taken from the study participants. Any potential identifiers were eliminated to ascertain confidentiality.
Socio-demographic characteristics
A total of 215 nurses participated in the study with a response rate of 93.5%. The age of the participants was from 20-43years with a median age of 27 years and more than two-thirds (75.8%) were in the age group of 20-29 years. More than half of the study participants (55.3%) were unmarried and (60.5%) were male. Similarly, more than half of the study participants (54.9%) had less than two years of work experience. Almost half of the study participants were (51.2%) were BSc and above graduate professionals (Table 1).
Variables |
Category |
Number |
% |
Age of respondents |
20-29 |
163 |
75.8 |
≥30 |
52 |
24.2 |
|
Sex of respondents |
Male |
130 |
60.5 |
Female |
85 |
39.5 |
|
Marital status of respondents |
Not married |
119 |
55.3 |
Married |
96 |
44.7 |
|
Ethnicity of respondents |
Oromo |
135 |
62.8 |
Amhara |
75 |
34.9 |
|
Others |
5 |
2.3 |
|
Level of education |
Diploma |
105 |
48.8 |
Degree & above |
110 |
51.2 |
|
Current working area |
IPD |
77 |
35.8 |
OPD |
138 |
64.2 |
|
Year of work experience |
>2 years |
97 |
45.1 |
|
<=2 years |
118 |
54.9 |
Table 1 Sociodemographic characteristics of nurses in north shewa zone hospitals, oromia region, Ethiopia, 2020 (N = 215)
Organizational related factors
More than half of the nurses (52.6%) and (67.9%) said their working unit lacked pressure injury prevention guidelines and equipment, respectively. Less than half of the study participants, (47%) had received formal training in the prevention of pressure injuries. Similarly, almost half of nurses, 50.7% reported a high workload, and more than half of nurses 52.6% were dissatisfied with their organization's nursing leadership style (Table 2).
Variables |
Category |
No |
% |
Got training on pressure injury prevention |
Yes |
101 |
47 |
No |
114 |
53 |
|
Availability of pressure injury prevention guidelines |
Yes |
102 |
47.4 |
No |
113 |
52.6 |
|
Availability of pressure injury prevention equipment |
Yes |
69 |
32.1 |
No |
146 |
67.9 |
|
Satisfied by the nursing leadership style |
Yes |
102 |
47.4 |
No |
113 |
52.6 |
|
Nurse-patient ratio (work load) |
<=1:10 |
106 |
49.3 |
>1:10 |
109 |
50.7 |
|
Knowledge on PI prevention |
Good |
120 |
55.8 |
|
Poor |
95 |
44.2 |
Table 2 Organizational and nurses’ related factors towards expressed pressure injury prevention practice in north shewa zone hospitals, oromia region, ethiopia, 2020 (N = 215)
Pressure injury prevention practice
The study revealed that nurses’ good practice of pressure injury prevention was 44 % (Figure 1). As the nurses’ pressure injury prevention practice scores revealed, 35.8% of the nurses always make the bed linens clean and dry all the times; 36.7% placed pillow under the patient’s calf, and (28.8%) give advice to patient and caregiver on pressure injury prevention practice (Table 3).
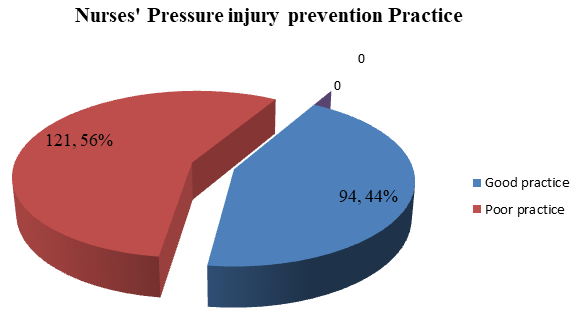
Figure 1 Pie chart shows nurses pressure injury prevention practice in north shewa zone government hospitals, oromia region, Ethiopia, 2020 (N = 215).
Variables |
Frequency of Practice score |
|
|
Always (%) |
Sometimes (%) |
Never (%) |
|
Identify common contributing factors for PI |
42(19.5) |
50(23.3) |
123(57.2) |
Used Braden scale for PI assessment |
34(15.8) |
62(28.8) |
119(55.4) |
Document all data related to PI assessment |
31(14.4) |
70(32.5) |
114(53.1) |
Do skin care routinely for admitted patients |
43(20) |
40(18.6) |
132(61.4) |
Placed pillow under the patients calf to prevent PI |
79(36.7) |
40(18.6) |
96(44.7) |
Gave advice for care giver to use cream on patient’ skin |
62(28.8) |
34(15.8) |
119(55.4) |
Make the bed linens clean and dry all the times |
77(35.8) |
36(16.7) |
102(47.5) |
Provide vitamins & food for malnourished patients |
29(13.5) |
54(25.1) |
132(61.4) |
Turn patients every two hours |
55(25.6) |
40(18.6) |
120(55.8) |
Advised patient and care giver regarding PIP care |
68(31.6) |
35(16.3) |
112(52.1) |
Provide perineal care for incontinency patients |
56(26.04) |
73(34.0) |
86(40.0) |
Table 3 Frequency distribution of the nurses’ practice score on expressed pressure injury in north shewa zone hospitals, oromia region, ethiopia, 2020 (N = 215)
PI, pressure injury PIP; pressure injury prevention.
Pressure injury prevention knowledge
In this study only, 55.8% of the study participants had a good knowledge of pressure injury prevention. All most, half of the study participants, 50.7% had no knowledge on the first sign of pressure injury development, 46.5 % on pressure injury risk assessment tools, 48.4% on the importance of change patients position, and 46.5% on the importance of the educational program in reducing the incidence of pressure injury (Table 4).
Variables |
Yes (%) |
No (%) |
The first sign of pressure injury development is open sore |
106(49.3) |
109(50.7) |
Immobility and altered consciousness are risk factors for PI |
91(42.3) |
124(57.7) |
Hot water and soap may dry the skin & increase the risk for PI |
89(41.4) |
126(58.6) |
It is important to massage bony prominences |
114(53) |
101(47) |
All individual should be assessed on admission for risk PI |
109(50.7) |
106(49.3) |
Braden scale is a risk assessment tool used for assessing PI |
115(53.5) |
100(46.5) |
Heel ulcer is prevented by putting pillow under the patients calf |
94(43.7) |
121(56.3) |
Skin cleaning should occurred at routine intervals for bed ridden patients having incontinence |
100(46.5) |
115(53.5) |
Malnourished patient are at higher risk of developing pressure injury |
115(53.5) |
100(46.5) |
Turn position for every 2 hours is significant activity for protecting skin damage |
111(51.6) |
104(48.4) |
Lift up the patient by dragging is correct practice for maintain skin integrity |
114(53) |
101(47) |
Educational program may reduce the incidence of pressure injuries |
115(53.5) |
100(46.5) |
Table 4 Frequency distribution of the nurses knowledge score towards expressed pressure injury prevention in north shewa zone hospitals, oromia region, ethiopia, 2020 (N = 215)
Perceived barriers for pressure injury prevention practice
Nurses were asked about the existence of specific barriers in their work environment and reported that lack of institutional policy 140(65.1%) and presences of other priorities other than pressure injury 137(63.7%) were the common barriers for implementing pressure injury prevention practice (Table 5).
Perceived barriers for expressed PU Prevention |
Response |
No |
(%) |
Poor access to literature affects nurses pressure injury prevention practice |
Yes |
118 |
54.9 |
No |
97 |
45.1 |
|
Lack of institutional policy about pressure injury prevention affects nurses pressure injury prevention practice |
Yes |
140 |
65.1 |
No |
75 |
34.9 |
|
Lack of cooperation among staff nurses affects nurses pressure injury prevention practice |
Yes |
105 |
48.8 |
No |
110 |
51.2 |
|
Uncooperative patients affects nurses pressure injury prevention practice |
Yes |
129 |
60 |
No |
86 |
40 |
|
Shortage of pressure relieving device affects nurses pressure injury prevention practice |
Yes |
103 |
47.9 |
No |
112 |
52.1 |
|
Presence of other priority than PI affects nurses pressure injury prevention practice |
Yes |
137 |
63.7 |
|
No |
78 |
36.3 |
Table 5 Percentage distribution of Nurses’ perceived barriers for pressure injury prevention practices working in north shewa zone hospitals, oromia region, ethiopia, 2020 (N = 215)
PI, pressure injury.
Factors associated with pressure injury prevention practice
A binary logistic regression analysis was carried out to identify candidate variables for multivariable logistic regression analysis model. In the multivariable logistic regression, education, knowledge, training, nurse to patient ratio, satisfied by the nursing leadership, and work experience were significantly associated factors. Compared with diploma nurses, BSc degree and above were 2 times (AOR: 2.075; 95% CI: 1.143, 3.765) more likely to have good expressed pressure injury prevention practice. Nurses who had good knowledge on pressure injury prevention were almost 2 times (AOR: 1.904; 95% CI: 1.038, 3.490) more likely to have good expressed pressure injury prevention practice as compared to their counterparts. Nurses who had got formal training on pressure injury prevention were 2.5 times (AOR: 2.498; 95% CI: 1.342, 4.648) more likely to have good expressed pressure ulcer prevention practice as compared to those nurses who had not got formal training on pressure injury prevention. Nurses who reported appropriate nurse to patient ratio were 2.3 times (AOR: 2.306; 95% CI: 1.242, 4.281) more likely to have good expressed pressure injury prevention practice than those nurses who reported inappropriate nurse to patient ratio. Similarly, nurses who were satisfied by the nursing leadership were 2.3 times (AOR: 2.347; 95% CI: 1.279, 4.304) more likely to have good expressed pressure injury prevention practice as compared to those nurses who were unsatisfied by the nursing leadership. Nurses with greater than two years of work experience were 1.84 times more 1.842(1.00-3.394) to practice pressure injury prevention than those nurses with two and less years’ work experience (Table 6).
Variables |
PUP Practice |
COR(95% CI) |
AOR(95% CI) |
|||
|
Adequate |
Inadequate |
||||
Educational status |
Degree & above |
60(54.5%) |
50(45.5%) |
2.506(1.439-4.365) |
2.075(1.143-3.765)* |
|
Diploma |
34(32.4%) |
71(67.6%) |
1 |
1 |
||
Knowledge on PI prevention |
Good |
62(51.7%) |
58(48.3%) |
2.105(1.207-3.670) |
1.904(1.038-3.490) * |
|
Poor |
32(33.7%) |
63(66.3%) |
1 |
1 |
||
Year of work experience |
>2 years |
50(51.5%) |
47(48.5%) |
1.789(1.037-3.088) |
1.842(1.00-3.394)* |
|
≤2 years |
44(37.3%) |
74(62.7%) |
1 |
1 |
||
Get training on PI prevention |
Yes |
54(53.5%) |
47(46.5%) |
2.126(1.228-3.678) |
2.498(1.342-4.648)* |
|
No |
40(35.1%) |
74(64.9%) |
1 |
1 |
||
presence of PIP guideline |
Yes |
52(51%) |
50(49%) |
1.758(1.02-3.03) |
1.376(0.733-2.583) |
|
No |
42(37.2%) |
71(62.8%) |
1 |
1 |
||
Nurse to patient ratio |
=<1:10 |
54(50.9%) |
52(49.1%) |
1.791(1.039-3.089) |
2.306(1.242-4.281)* |
|
>1:10 |
40(36.7%) |
69(63.3%) |
1 |
1 |
||
Satisfied by the nursing leadership |
Yes |
53(52%) |
49(48%) |
1.899(1.1-3.279) |
2.347(1.279-4.304)* |
|
|
No |
41(36.3%) |
72(63.7%) |
1 |
1 |
|
Table 2 Bivariate and multivariate analysis of factors associated with nurses’ expressed pressure ulcer prevention practice in north shewa zone hospitals, oromia region, ethiopia, 2020 (N = 215)
Prevention of pressure ulcers is an indicator of quality of care and nursing care has a major effect on pressure ulcer development and prevention. So this study was aimed to assess nurses’ pressure injury prevention practice, the perceived barriers and associated factors in Northern Oromia Government hospitals of Ethiopia.
In this study, 44 % (95% CI: 37.1%-50.3%) of the participants had good practice of pressure injury prevention, which is consistent with Ethiopians study’s finding in Wolaita Sodo University Teaching and Referral Hospital(37,9%)20 in Harare and Dire Dawa town public hospitals (51.9%)21 and in Gonder University Hospital (48.4 %).22 This consistency could be explained by similarity of the study settings and study population. However, it is lower than the study finding conducted in Addis Ababa Public Hospitals (67.3%) and in Gurage Zone Public Hospitals (58.5%) in Ethiopia.23 But higher than a study finding in Tigray public hospitals, Ethiopia (17.2%)This discrepancy might be due to different assessment tools and scoring system. As the study result revealed lack of institutional policy was the main listed barrier for the implementation of pressure injury prevention practice, which accounts for 65.1% of the study respondents. The presence of other priorities other than pressure injury prevention (63.7%) was the second most reported barrier for nurses’ pressure injury prevention practice followed by uncooperative patient (60%). Poor access to literature was listed as barrier for nurses’ pressure injury prevention practice by more than half of the nurses’ (54.9%).
The study identified significant factors of nurses’ pressure injuries prevention practice. Nurses’ pressure injuries prevention practice showed an association with some socio-demographic variables. Holding of bachelor and above degree was significantly associated with nurses ’pressure injuries prevention practice. Studies conducted in Ethiopia at Wolaita Sodo University Teaching and Referral Hospital in Gurage Zone hospitals and in Harare and Dire Dawa town public hospitals supported this association. Th is might be explained by nurses at higher level of education will have good knowledge that eatable them to practice pressure injuries prevention activities accurately. Work experience in nursing was another socio-demographic related factor showed significant association with nurses’ pressure injuries prevention practice, which is also supported by a study finding in Wolaita Sodo University Teaching and Referral Hospital. The possible justification for this association will be nurses who spent longer time in the clinical area will develop better experience by observing other skilled staffs, by updating themselves. Among nurse’s related factors, knowledge of pressure injury prevention was significantly associated with their pressure injury prevention practice. This relationship is supported by three studies in Ethiopia conducted in Harare and Dire Dawa town public hospitals, in Wolaita Sodo University Teaching and Referral Hospital, and in Gurage Zone hospitals respectively and in a study result in Jeddah city. This might be because of knowledge is a prerequisite for practice.
A higher level of nurse’s satisfaction with the nursing leadership was significantly correlated with pressure injuries prevention practice, which is supported with a study result in Gonder University Hospital. The study showed that nurses who reported appropriate nurse-patient ratio were experiencing good pressure injuries prevention practice, which is supported by the finding of a study in Gurage Zone hospitals and in Gonder University Hospital and in South Eastern Nigeria. Training on pressure injuries prevention was another significant factors of nurses’ pressure injuries prevention practice in the current study, which supported by a study findings in South Eastern Nigeria24 and Iran.25
Study limitation
Since the data were collected by self-administered questionnaire, this approach might affect the accuracy of responses and as the study was cross-sectional, it did not indicate the precedence of outcome or exposure.
The practice of nurses’ pressure injuries prevention was 44 %, which is inadequate to prevent the occurrences of pressure-induced skin injuries. Work experience in nursing, educational status, Knowledge, training on pressure injury prevention, inappropriate nurse to patient ratio, and satisfaction with the nursing leadership style were predictor of nurses’ expressed pressure injury prevention practice.
I would like to express my deepest gratitude to Salale University, North Showa zone health Bureau, and to study hospitals administrative bodies. I acknowledged all data collectors and study participants for their cooperation to participate in the study.
Salale University funded this research work. The funder had no role in study design, data collection, analysis, decision to publish, or manuscript preparation.
The author declare that he have no competing interests regarding the publication of this paper.
Recommendations
improving nurses’ Knowledge towards pressure injury prevention, provide training on pressure injury prevention, educate nurses to a higher level of education, allocate appropriate nurse to patient ratio, and makes the nursing leadership style conducive will help to increase nurses pressure injury prevention practice.
Declarations of ethical approval
Ethical approval letter was taken from the Institutional Review Board (IRB) of Salale University after approval of the proposal. Before data was collected, permission letters were obtained from the study hospitals, and each study participant gave their written agreement voluntarily.
Consent to publication
Not applicable.
Data availability
The data supporting this study are made available within the manuscript.
Author contributions
All the activities in this paper including ideal conception, study design, data collection, analysis and interpretation were performed by author.
Generalizability
Because the study included all of the source population, the study result is more generalizable to the study area.

©2022 Benayew. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.