eISSN: 2572-8474


Research Article Volume 9 Issue 2
1Department of Nursing, Addis Ababa University, Ethiopia
2Department of health informatics, Debre Berhan Health Science College, Ethiopia
Correspondence: Teshome Habte, Department of Nursing, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia
Received: February 20, 2023 | Published: March 1, 2023
Citation: Habte T, Abebe E. Assessment of colostrum avoidance practice and associated factors among mothers of children under 2 years in Debre Berhan town North Shwoa Zone, Ethiopia: a community-based cross sectional study. Nurse Care Open Acces J. 2023;9(2):26-31. DOI: 10.15406/ncoaj.2023.09.00255
Background: A Scientific evidence has revealed early feeding of colostrum to the newborn is a key to tackle against harmful germs by coating his intestines, and helping to shield his immune system against germs.
Objective: To assess Colostrum avoidance and associated factors among mothers of children under 2 years of age in Debre Berhan town North Shewa Zone, Ethiopia.
Methods: A community-based cross-sectional study was conducted to assess colostrum avoidance practice in Debre Berhan town with total sample of 296 mother’s of children under two years of age from January 15to February 20, 2021. Data were collected by using structured-interview questionnaires from randly selected four kebeles after proportionaly allocated the study population for eah kebeles. Bivariate and Multivariate logistic regression analysis was done to examine the possible predictors and chi-square test was doneto check variables with the statistical association of P-value of < 0.05 and OR with 95% confidence interval were considered.
Result: All the study participants were enrolled in making a response rate of 100%.The mean age of the mother was 28.6 with 4.99 Standard deviation and the majority of them were orthodox 197 (66.6%) and 105(35.5%) of mothers were complete secondary education level. Out of 296, 122 (41.2%) of mothers were housewife, 262(88.5%) were married. The prevalence of colostrum avoidance was 17.9%, who did not feed colostrum for their child with different reasons. Out of this mothers who avoid their colostrum milk due to maternal illness 29(54.72%), dirty 4(7.55%) and Yellowish milk with 34(64.15%) of by their own decision and gave other feed 17 (25%).The reasons of colostrum avoidance with avoidance practice x2 =44 with p value <0.01 and COR =1.3(1.1-1.5, Prelacteal feedings were 3.16 higher to avoid their colostrum than those who had aware of colostrum feeding mothers (COR=4.2, AOR=3.16, 95% CI=1.6-6.19) were statistically associated with colostrum avoidance.
Conclusion and recommendation: To improve neonatal health and growth, maternal awareness is decisive factor through delivering health education and promoting immediate colostrum feeding practice therefore, attention is required by community health workers to work on it.
Keywords: colostrum avoidance, practice, associated factors, mothers of children under 2 years, Northshewa, Ethiopia
AOR, adjusted odds ratio; CI, confidence interval; COR, crude odds ratio; WHO, world health organization; UNICEF, united nations international children’s emergency fund; ANC, antenatal care; BCC, behavioral change communication; BF, breast feeding; EBF, exclusive breast feeding; EDHS, ethiopian demographic survey; PLF, pre lacteal feeding; PNC, post natal care; TIBF, timely initiation of breastfeeding
Colostrum is the first liquid that is produced in the first few hours after delivery. It is the perfect first food for your baby the transition from colostrum to mature milk is a gradual process. In the 2-3 weeks following delivery, you will notice your milk becoming thinner, less yellow and milky which is called “Foremilk”.Hind milk is the milk which follows foremilk during a feeding. It is richer in fat content and is high in calories. The high fat and calorie content of this milk is important for your baby’s health and continuing growth. Make sure to let your baby drain one breast before moving on to the other.1,2 Globally, child death is higher as compared to other age groups and more than 75% occurs in developing countries. Scientific evidence has reviled early feeding of colostrum to the newborn remained as the key to tackle infant nutrition and also the survival of infant.3,4 Colostrum is thick, sticky and clear to yellowish in color and also contains proteins, vitamin A and maternal antibodies important to the new born nutrition until lactation is fully established.5–7 The World Health Organization and United Nations International Children’s Emergency Fund recommended that after delivery, optimal early breast feeding practices should be encouraged. These optimal practices include initiating breastfeeding within 30 minutes to an hour of birth, giving colostrum, not giving pre-lacteal or post-lacteals and exclusive breastfeeding of infants.8,9 Avoiding colostrum in the first three crucial days after birth increases the risk of infection and death among neonates and child mortality in developing countries is more associated with malnutrition as well as colostrum avoiding deprives the newborns of nutrients and immunoglobulin and causing a reduction in the priming of the gastrointestinal tract, and increases the risk of infant morbidity and mortality.10–12 More than 4 million babies die in the neonatal period every year, and most of these deaths occur in poorer countries due to longer delay in breastfeeding initiation and discard colostrum, the greater chances of neonatal mortality caused by infections. Breastfeeding include colostrum within the first hour of life has been shown to reduce high neonatal mortality by 22%. According to EDHS, 2016, Seventy-three percent of children began breastfeeding within 1 hour of birth, and 92% within 1day of birth, which are 22 and 12 percentage points higher than in 2011, respectively. The practice of pre lacteal feeding, likewise, decreased from 29% in 2005 to 27% in 2011, and dropped further to 8% in 2016.13,14
Some mothers in developing countries avoid colostrum feeding on the basis of traditional or cultural beliefs that range from viewing it as having no nutritional value, seeing it as harmful to the infant’s health (making the baby sick or even causing death), or seeing it as ‘bad luck’ for the family.5–7 Some women may specify no reason for avoiding colostrum other than tradition.7 As a study conducted in Egypt, 42.2% and 57.8% of newborns received colostrum and pre-lacteal feeds in the first feed, respectively. The commonest Pre lacteal Feeding (PLF) were sugar/glucose water (39.6%), infant formula (28.6%), and herbs/decoction (21.7%).15 The findings from this study are used as a baseline information future researches and used to local manager, local planners, other health professionals, mothers of children and community leaders about the colostrum avoidance practices.16
Study setting, population and study design and period
The study was conducted at a randomly selected kebeles at Debre Berhan Town. Debre Berhan town is one of the 13 zones of Amhara regional state and the main city of North Shewa zone, which is located 130 km north of Addis Ababa and 682 km from capital city of Amhara regional state Bahir Dar. It is found on the altitude of 2,850m from sea level with the temperature ranging from 13oC to 28oC. As the information found from the city administration office. The city incampassess a total of nine kebeles’ with the total population of 108,825 of which 49,208 are males and 59,617 are females. Amongst female population, 9000 of them are women in the reproductive age group (15-49yr) and children less than two years of age, is 5,492. (report of the city administration office). A community based cross sectional study design was employed from January 15 to February 20, 2021.
Inclusion criteria
Mothers who have biological child under 2 years of age and residence at least six months in the study kebele’s.
Sample size determination
The sample size was calculated using single population proportion formula by considering the following assumptions: 13.5% prevalence of colostrum discarding in Raya Kobo district using Z = 95% Confidence level, d = 5%, design effect = 1.5 and 10% non-response rate Sample size was calculated.17
n= 179+18= 197*1.5= 296.
Sampling procedure and technique
Out of the nine kebeles in the city four of them were selected using simple random sampling method. As depicted in Figure 1 below the study participants from selected Kebele’s were determined by proportionally allocation with assuming that there could be no difference regarding colostrum avoidance between urban kebeles. Each eligible study participants were selected using systematic random sampling technique. The sampling frames were obtained from health post of each kebele’s. The first participant was selected using a lottery method and the next participants were selected at every 6th interval from the sampling of the selected kebeles.
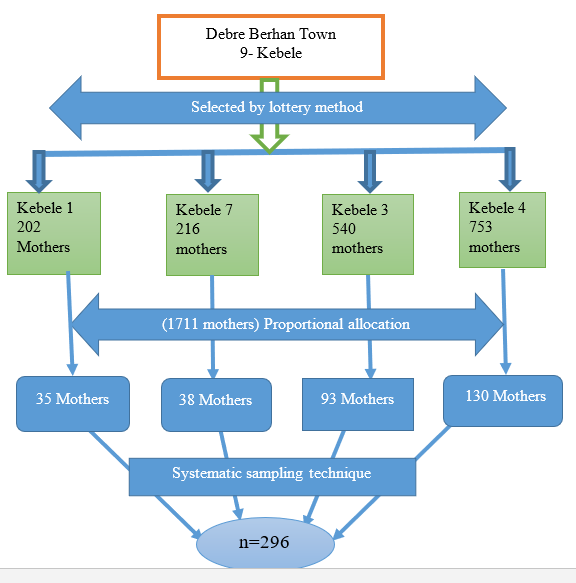
Figure 1 Schematic presentation of sampling technique to assess colostrum avoidance practice and associated factors among mothers of children under 2 years of age in Debre Berhan town, North Shewa zone, Ethiopia, 2021.
Study variables
Operational definition
Colostrum avoidance: is failure to feed infants with the first, thick and yellowish milk that is produced in the first three days after birth.
Poor knowledge: refers knowledge of colostrum feeding those mothers who was answers below three answers out of six knowledge of colostrum feeding questions.
Good knowledge: refers knowledge of colostrum feeding those mothers who were answered greater than three out of six knowledge of colostrum feeding questions.
Source of information: Source of information about breast feeding or colostrum feeding practices from health professionals, mass media, and friends.
Biological mother: Refers to mother who gave birth.
Data collection procedure
Interview questionnaires were conducted from different related studies and necessary modifications were done4,5,16. A translated in to Amharic version questionnaire was used to collect data. It covers socio-demographic factors of families, the occurrence of colostrum avoidance practice and associated factors that influence to remove the colostrum.
Data processing and Analysis
Data was sorted, coded, entered, categorize and analyzed using SPSS version 22 statistical software. Then, collected data was summarized and describe by descriptive statistics (percentages, frequency, mean values and standard deviations) as well as presented in tables, graph, pie charts. Appropriate tables were used to present findings and Chi- square test was done to check presence of significance associations. The Bivariate and logistic Multivariate analysis were used to test significance association of dependent and independent variables using OR with 95% of CI. Statistical significance p value (<0.05) and the level of confidence is 95% was used to describe there is significant association between dependent and independent variables.
Data quality control
Training was given for data collectors and supervisors for one day and questionnaires were pre tested. Prior to the actual data collection, pre-testing was done in non-sampling area 5% 16 of the total sample size to check clarity, completeness, consistency and setting of time required to conduct.
Socio-demographic characteristics
A total of 296 mothers were enrolled in the study with 100% response rate. In this study, the majority (61.8%) of the study participants were within 24-34yrs of age group with the mean age of participants was 28.6 and Standard deviation 4.99 and about 197 (66.6%) were orthodox religion followers, maternal history of the participants were having two children was 197 (66.6%) this indicates that majority of the study participants were gave birth two times. Their level of education about 90 (30.4%) of the mothers were complete secondary school and 122 (41.2%) house wife the remaining government employe, farmer, trader, daily laborer, and 10%, 31%,15% and 2% respectively.
Colostrum/breast feeding practice at Debre Berhan town
From the total of 296 mothers 243(82.1%) of them had colostrum feeding practice for their child and only 53(17.9%) did not feed colostrum for their child with different reasons. As depicted in Table 1 below, out of 53 mothers who avoid their colostrum milk were responded 29(54.72%) due to maternal medical illness and 4(7.55%) due to dirty and Yellowish milk with 34(64.15%) of mothers avoid colostrum feeding by their own decision. From the total mothers, majority of them 229(77.4%) were did not given pre-lacteal feeding practice but 22.6 % only gave to their children with different reasons such as maternal illness was 18 (27%).
Variables |
Response |
Number |
Percentage |
Colostrum feeding practice with in five days |
Yes |
243 |
82.1 |
No |
53 |
17.9 |
|
Initiation time of breast feeding |
Before 1 hour |
224 |
92.2 |
After 1 hour |
19 |
7.8 |
|
Reasons of colostrum avoidance |
Maternal medical illness |
29 |
54.72 |
have no milk |
14 |
26.42 |
|
cause of abdominal pain |
6 |
11.32 |
|
Dirty and yellowish |
4 |
7.55 |
|
Influence person |
Own decision |
34 |
64.15 |
Traditional birth attendant |
11 |
20.75 |
|
Grandparents |
2 |
3.77 |
|
Friends |
5 |
9.4 |
|
Others |
1 |
1.9 |
|
Prelacteal feeding practice |
Yes |
67 |
22.6 |
No |
229 |
77.4 |
|
Reasons of mothers who gave other feeding within five days |
BF not satisfy |
13 |
19.40% |
Cleanse infant bowel |
15 |
22.39% |
|
Due to maternal illness |
18 |
26.87% |
|
Culture |
6 |
8.96% |
|
|
to calm it |
15 |
22.39% |
Table 1 Colostrum feeding practice of mothers at Debreberhan town (n=296)
Factors influencing colostrum avoidance
According to the knowledge of the mothers in regarding colostrum feeding was 243(82.1%) know about colostrum meaning, of which 178(60.1%), 51(17.2%), 53(17.9%) were Yellow milk, thick milk and unknown response of its meaning respectively and only 91(30.7%) mothers listed more >=3 about colostrum milk knowledge that were considered to be good knowledge based on our study but 69.3% response <3 classified as poor knowledge about colostrum.
Health care service utilization
From the total of mother respondents 98% had ANC visit in the last pregnancy, 214(72.3) had got more than four ANC visiting among of this 199 (67.2%) mothers were knowing appropriate time about colostrum feeding time and 191(64.5%) mothers feed immediately their children but 30.8% and 2% of mothers were attending below 4 ANC visit and had no any visiting respectively.
Associated Factors affecting colostrum avoidance practice
Based on the cross tabulation analysis , mothers occupation, family type, as depicted in Table 2 below, knowledge of the mothers about colostrum ,mothers source of information about colostrum, ANC visit, Breast feeding counseling, mode of delivery were statistically significance with colostrum avoidance practice whereas age of the mother ,mother educational level, husband educational status, monthly income, marital status of the mothers, gestational age of children were not significantly associated. In the binary logistic regression at P< 0.05 (with 95% of CI), mother occupation, daily labor, family type, source of information of the mothers, knowledge of mothers about colostrum, breast feeding counseling ,mode of delivery were statistically associated with colostrum avoidance practice . In multivariate analysis, mother occupation (merchant), 64% of the mothers more practice to avoid colostrum than other mothers occupation, AOR=0.36 ,95%CI =(0.14-0.939), and daily labor ,85% of mothers were more practice than housewives, AOR=0.15,95%CI=(0.3-0.78), as shown in Table 3 below, mothers who did not get source of information about colostrum, 55% of them who were more practiced than who got information about colostrum, AOR=0.45,95% CI= (0.209-0.99), and mother who did not get breast feeding counseling ,72% of them were more practiced than those who got breast feeding counseling during ANC follow up, AOR=0.28,95%CI=0.12-0.635).
Variable |
Categories |
Colostrum avoidance practice |
p-value |
|
Yes |
No |
|||
Age group of mother |
18-24 yrs |
8(15.5%) |
60(24.7%) |
0.317 |
25-34 yrs |
34(64.2%) |
149(61.3%) |
||
34-44 yrs |
11(20.8%) |
33(13.6%) |
||
>45 yrs |
0 |
1(0.4%) |
||
Mothers’ education level |
Unable to read and write |
11(20.8%) |
28(11.5%) |
0.379 |
Able to read and write |
16(30.2%) |
68(28.0%) |
||
Primary education |
9(17.0%) |
59(24.3%) |
||
Secondary education |
15(28.3%) |
75(30.9%) |
||
College and above |
2(3.8%) |
13(5.3%) |
||
Husband educational level |
Unable to read and write |
6(12.2%) |
17(7.4%) |
0.331 |
Able to read and write |
11(22.4%) |
42(18.2%) |
||
Primary education |
12(24.5%) |
73(31.6%) |
||
Secondary education |
19(38.8%) |
80(34.6%) |
||
College and above |
1(2.0%) |
19(8.2%) |
||
Monthly income |
Below1000 birr |
9(17.0%) |
28(11.5%) |
0.137 |
1001-2000 birr |
16(30.2%) |
47(19.3%) |
||
2001-4000birr |
10(18.9%) |
50(20.6%) |
||
>4000 birr |
18(34.0%) |
118(48.6%) |
||
Mothers occupation |
Housewife |
19(35.8%) |
103(42.4%) |
0.002 |
Merchant |
13(24.5%) |
32(13.2%) |
||
Government employee |
5(9.4%) |
25(10.3%) |
||
Farmer |
11(20.8%) |
80(32.9%) |
||
Daily labor |
5(9.4%) |
3(1.2%) |
||
Variable |
Catagories |
Colostrum avoidance practice |
p-value |
|
Yes |
No |
|||
Family type |
Nuclear family |
36(67.9%) |
198(81.5%) |
0.008* |
Extended family |
13(24.5%) |
42(17.3%) |
||
Other |
4(7.5%) |
3(1.2%) |
||
Marital status |
Single |
5(9.4%) |
14(5.8%) |
0.132 |
Married |
44(83.0%) |
218(89.7%) |
||
Widowed |
1(1.9%) |
8(3.3%) |
||
Separation |
3(5.7%) |
3(1.2%) |
||
Child gestational age |
Term |
41(77.4%) |
185(76.1%) |
0.201 |
Pre term |
10(18.9%) |
32(13.2%) |
||
Post term |
2(3.8%) |
26(10.7%) |
||
Knowledge of mother about colostrum |
Yes |
34(64.2%) |
209(86.0%) |
0.001* |
No |
19(35.8%) |
34(14.0%) |
||
Got Source of information about colostrum |
Yes |
34(64.2%) |
209(86.0%) |
0.001* |
No |
19(35.8%) |
34(14.0%) |
||
ANC visit |
Yes |
50(94.3%) |
240(98.8%) |
0.038* |
No |
3(5.7%) |
3(1.2%) |
||
BF counseling |
Yes |
30(56.6%) |
194(79.8%) |
0.001* |
No |
23(43.4%) |
49(20.2%) |
||
Place of delivery |
Health institution |
48(90.6%) |
231(95.1%) |
0.202 |
Home |
5(9.4.%) |
12(4..9%) |
||
Mode of delivery |
CS |
14(26.4%) |
33(13.6%) |
0.026* |
SVD |
39(73.6%) |
199(81.9%) |
||
Instrumental |
0 |
11(4.5%) |
||
PNC visit |
Yes |
18(34%) |
102(42.0%) |
0.28 |
no |
35(66.0%) |
141(58.0%) |
||
|
||||
Table 2 Factors associated with colostrum avoidance among respondent mothers using cross tabulation and Chi's square test at Debre berhan town (n=296)
This study revealed that the prevalence of colostrum avoidance was 17.9% which is higher than the study conducted Aksum town (6.3%) 5, in Kombolcha was (11. 4%) 10, in Raya kobo was 13.5% 17 and prevalence of result was lower than in Mezan Tepi was 19.3%)18 and also it was lower than study in India (76.0%),the mothers response report indicated that 51.5% considered as colostrum was not important.1 This result revealed that mother occupation (merchant), 64% of the mothers more practice to avoid colostrum than other mothers occupation, AOR=0.36 ,95%CI =(0.14-0.939), and other than daily labor ,85% of mothers who were more practice than housewives, AOR=0.15,95%CI=(0.3-0.78) but the other literatures were not including occupation of the mother . So that the mothers with merchant occupation and daily laborer were avoid colostrum than other mother’s occupations. This finding reveal that, mothers who did not get source of information about colostrum, 55% of them who were more practiced than who got information about colostrum, AOR=0.45, 95% CI= (0.209-0.99) which was lower than a study was conducted in Aksum, mother information on colostrum feeding [AOR=4.8 (95% CI=1.83, 12.69)] were statistically associated with colostrum avoidance (at P value of < 0.05,)(4).The difference could be difference maternal knowledge, mother educational level, difference settings, and communities location difference. This study revealed that the mothers who had colostrum feeding practice 243(82.1%) feed colostrum for their child, of 224(75.7%) and 67(22.6%) mothers were having breast feeding initiation with in l hour and Prelacteal feeding below five days respectively. The study conducted in Aksum, regarding the breastfeeding initiation, 271(56.8%) mothers have initiated breastfeeding within 1 hr. and 48 (10.1%) were providing pre-lacteal feeding within three days before giving breast feeding to their child5 and in Addis Ababa, 102 (20.6%) were reported giving Prelacteal feeds to their infants within the first three days before giving breast milk.11 Our finding had higher in breast feeding practice, initiation time and Prelacteal feeding. Debre Berhan Town were due to socio cultural difference between two communities.
Regarding to the Prelacteal feeding in our finding 67 (22.6%), As the study conducted in wolaita-zone, southern Ethiopia the prevalence of pre-lacteal feeding practice was 20.6%.19,20 in these case our finding was intermediate change between to communities might be due to difference in culture, the difference in infant feeding style, settings and study period. As this study result knowledge of the mothers in regarding colostrum feeding was 243(82.1%) knew about colostrum meaning, of which 178(60.1%), said Yellow milk and only 91(30.7%) of mothers had good knowledge and the remaining have poor knowledge, some of them heard about colostrum meaning from health professional, 140(57.6). Whereas similar study conducted in Debre Marko town21 majority of mothers 290(76.72%) of mothers responded good knowledge about colostrum breast milk and majority of mothers heard about colostrum and its importance from health institutions by health profession 299(79.10 %).
Limitations
Due to cross sectional study design establishing a temporal relationship between dependent and independent variable is impossible.
Recent international initiatives have drawn the attention of Ethiopian mothers to not to give Prelacteal feeding and avoid colostrum in the first six months of life. To encourage neonatal health and growth through breast milk feeding, we recommend culturally tailored education delivered by community health advocators, BF counseling’s and traditional health practitioners that promotes immediate colostrum feeding and discourages Prelacteal feeding and colostrum avoidance practice habit. The most common prenatal food was; sugar water and water followed by plan water.
Recommendation
Debre Berhan town administration health office: should work on encouraging Behavioral change communication (BCC) tasks on the disadvantages of colostrum avoidance and Health Education activities should be aimed at not only mothers of child, but also include their family’s members and local cultural practice and should be implemented at facilities and communities level to decrease the colostrum avoidance practice.
For health extension workers: need to increase awareness about early initiation of Breast feeding and its importance for optimal growth of children in the community. Need to give health education on colostrum feeding for the mother in the community.
Ethics approval and consent to participate
Ethical approval was obtained and allowed by the Research and Ethical approval Committee at the Department of Nursing and Midwifery, College of Health Sciences in Addis Ababa University. Furthermore, official letters were written to the respective health institutions. Verbal and written consent was obtained from each participant and anonymity and confidentiality were kept. Respondents were having the right not to participate in or withdraw from the study at any stage. This study was conducted in accordance with the principles of the Declaration of Helsinki.Each study participants were informed about the purpose and procedure of the study and their right to refuse was respected and written consent was obtained from all study participants before the interview. The respondents were also told that the information obtained from them be treated with complete confidentiality and do not cause any harm to them.
Availability of data and materials
Data supporting the conclusions of this article are available by request to, Endegena abebe. The relevant raw data will be made available to researchers wishing to use them for non-commercial purposes.The authors acknowledge to Debreberhan town administrative office, community leaders, Community health post workers and study participants for their valuable support.
The authors declare that they have no conflicts of interest.
None.
HT and AE wrote the research, developed the questionnaire, analyzed the data and wrote the paper and interpreted the findings as well as participated in the preparation of the manuscript. Both authors supervised the data collection, contributed to the interpretation of the findings, and participated in the preparation of the manuscript. All authors read and approved the final manuscript.

©2023 Habte, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.