MOJ
eISSN: 2475-5494


Research Article Volume 8 Issue 2
1Arba Minch College of Health Sciences, Ethiopia
2Arba Minch General Hospital, Ethiopia
Correspondence: Mende Mensa, Arba Minch College of Health Sciences, Ethiopia, Tel +2510937170976
Received: July 15, 2017 | Published: April 3, 2019
Citation: Mensa M, Belijo MN. Status of skilled birth attendance utilization and determinants among women of child bearing age in Chencha Woreda, Gamo Gofa zone, Southern Ethiopia, December 2016. MOJ Womens Health. 2019;8(2):178-190. DOI: 10.15406/mojwh.2019.08.00233
Background: Approximately 99% of maternal deaths are occurring in developing countries and most of these deaths could have been prevented if mothers had access antenatal care (ANC) during pregnancy, were attended by a skilled birth attendant. However the prevalence of skilled birth attendance and institutional delivery were still low in developing countries like Ethiopia. Therefore this study was aimed at exploring the reasons for low skilled birth attendance in rural communities of Chencha District Gamo Gofa Zone, Southern Ethiopia.
Objective: To assess the status of skilled birth attendance and its determinants among mothers in rural communities of Chencha district, southern Ethiopia, December 2016.
Methods: A community based cross sectional study that employed quantitative data collection method was conducted. Multi stage sampling technique was used for selection of study participants. A pre tested semi-structured questionnaires via interview was used to collect data on different variables.
Results: There are 500 women who had children less than 5 years old were participated in this study. Majority of participants 356(71.2%) were in the age group of 26-30 years with Mean age of 27.44±(3.076) years. Age of the mother 21-25 years [AOR=1.56 (1.204-3.516), Government employed husband [AOR= 1.669 (1.475-81.642), Mothers with monthly income above 5000 ETB [AOR=2.196 (1.051-4.590), No ANC follow-up[AOR=0.915 (0.375-0.953), Mothers who reported health professionals are not well skilled [AOR= 0.227 (0.085-0.607) and Health facility in less than 5km distance [AOR=3.116 (1.916-5.068) were independent predictors of skilled birth attendance utilization.
Conclusion: Our study revealed that prevalence of skilled birth attendance below one third. Age of the mother 21-25 years, Mothers with government employed husband, mothers with monthly income above 5000 ETB, ANC follow-up, Health professionals skilled and Health facility in less than 5km distance were predictors of skilled birth attendance utilization. Designing strategies to address these variables by responsible bodies is critical.
Keywords: skilled birth attendance, knowledge, attitude, antenatal care, southern, ethiopia
ANC, antenatal care; BEmONC, basic emergency obstetrics and neonatal care; C/S, cesarean section; CemON, comprehensive and emergency obstetrics and neonatal care; CI, confidence interval; DHS, demographic and health survey; EDHS, ethiopian demographic and health survey; EmOC, emergency obstetric care; ETB, ethiopian birr; HEW, health extension worker; HF, health facility; HSDP, health sector development program; MDG, millennium development goal; MMR, maternal mortality ratio; MOH, ministry of health; PAD, professionally assisted delivery; PI, principal investigator; RH, reproductive health; SBA, skilled birth attendants; SNNPR, southern nation, nationalities and peoples region; SPSS, statistical package for social studies; SSA, sub sahara africa; SVD, spontaneous vaginal delivery; WCBA, women of child bearing age; WHO, world health organization.
Addressing maternal health encompasses social, cultural, health systems and health policy factors globally. Among these factors complications of pregnancy and childbirth are a leading cause of maternal morbidities and mortalities for women of reproductive age (15–49 years) in developing countries. The WHO estimates that over 500,000 women and girls die from complications of pregnancy and childbirth each year, worldwide, with approximately 99% of these deaths occurring in developing countries. With a maternal mortality ratio of 545 deaths per 100,000 live births.1,2
As revealed in the UN MDGs, reducing maternal mortality as well as improving maternal and reproductive health, represent important areas of concern in the world today. Nearly 3.4 million of the 8 million infant deaths each year occur within the first week of life and are often due to a lack of or inappropriate care during pregnancy, delivery and the post-partum period.3
Hemorrhage, infection, eclampsia, obstructed labour and post abortion complications accounts for 80% of all direct causes maternal deaths, and the final 20 % are due to indirect obstetric causes like HIV/AIDS, anaemia, malaria and cardiovascular disease. Between 11% and 17% of maternal deaths occur during childbirth itself and between 50% and 71% in the postpartum period. About 45% of the postpartum maternal deaths occur during the first 24 hours, and more than two thirds during the first week.4
According to 2015 estimates, 303 000 maternal deaths occurred globally in 2015, yielding an overall MMR of 216 maternal deaths per 100 000 live births. The global lifetime risk of maternal mortality is approximately 1 in 180 for 2015. The overall MMR in developing regions is 239, which is roughly 20 times higher than that of developed regions, where it is just 12. Developing regions account for approximately 99% (302 000) of the estimated global maternal deaths in 2015, with sub-Saharan Africa alone accounting for roughly 66% (201 000), followed by Southern Asia (66000). The lifetime risk of maternal mortality is estimated at 1 in 36 in sub-Saharan Africa, contrasting sharply with approximately 1 in 4900 in developed countries. In Ethiopia, our country of interest, numbers from year 2016 estimate the level of maternal mortality (MMR) is high 412 per 100,000 live births.5,6
Global targets for ending preventable maternal mortality (EPMM) By 2030, every country should reduce its maternal mortality ratio (MMR) by at least two thirds from the 2010 baseline, and no country should have an MMR higher than 140 deaths per 1,00,000 live births (twice the global target).7 Most of these maternal deaths could have been prevented if mothers had access antenatal care (ANC) during pregnancy, were attended by a skilled birth attendant (SBA) who was able to deal with complications during delivery, and had appropriate care and support in the early postpartum period.8 In low and middle income countries, a significant proportion of women still deliver at home either without or with support from unskilled health providers.9
The Government of Ethiopia is succeeded in reducing MMR by three-quarters over the period 1990 to 2015 by applying multi-pronged approaches to reduce maternal and newborn morbidity and mortality through Federal ministry of Health (FMOH). It is striving to assure improved access to emergency obstetric services and to create home delivery free villages in each district and achieve Global targets for ending preventable maternal mortality (EPMM)By 2030, every country should reduce its maternal mortality ratio (MMR) by at least two thirds from the 2010 baseline, and no country should have an MMR higher than 140 deaths per 100 000 live births (twice the global target).6,7 More than 80% of maternal deaths worldwide are due to five direct causes, hemorrhage, sepsis, unsafe abortion, obstructed labor and hypertensive diseases. Most of these deaths can be prevented if women have access to essential obstetric care during pregnancy. Approximately 61% of births in developing countries take place with the help of SBAs although this number varies by regions.10
In most cases, the lower the percentage of SBAs at delivery for country or region, the higher the lifetime risk of maternal mortality in that region or country. A recent four-country (Benin, Ecuador, Jamaica and Rwanda) study has demonstrated that higher levels of skilled attendants during delivery lead to lower maternal mortality.17 It is estimated that, if there were SBAs at all deliveries, maternal mortality could be reduced by 13-33%.There are sound clinical reasons for a focus on skilled attendants.11
The effect of low utilization of quality maternal care services is known to be a contributory factor to the high incidence of avoidable deaths of pregnant women in mostly developing nations including Ethiopia. Despite these clear evidence Studies showed that Utilization of maternal health services in developing countries is low and hindered by factors like lack of infrastructure, quality of services provided and accessibility of the service.12 Access to Skilled Birth Attendance during childbirth and in the immediate post-natal period and access to Emergency obstetric care in case of obstetric complications are considered to be effective interventions to reduce the number of global maternal and newborn deaths.13 Study conducted in North West Ethiopia showed that only 38.2% of women gave birth in health facilities for their most recent birth while the most 223 (61.8%) delivered at home. Most women (87.4%) who did not deliver in health facilities were assisted by Lay birth attendants (families, friends or neighbors) followed by Health extension workers (7.2%), and traditional birth attendants (5.4%), respectively. The major reasons of institutional delivery were fear of complications (77.5 %), to get better service (56.5%) safe and clean delivery (46.4%) and they were communicated to deliver at health facilities during ANC attendance, 47(35.5%).14
There are many factors that affect the outcome of pregnancy from the onset of any obstetric complication. The outcome is most adversely affected by delayed treatment. Delay in treatment is the result of many factors; I) Lack of information and adequate knowledge about danger signals during pregnancy and labor; cultural/ traditional practices that restrict women from seeking health care; lack of money; II) Out of reach of health facilities; poor road, communication network, community support mechanisms and III) Inadequate skilled attendants; poorly motivated staff; inadequate equipment and supplies; weak referral system, procedural guides.15 Trends of skilled birth attendance are increasing from time to time. For example 80% of births to urban mothers were assisted by a skilled provider and 79% were delivered in a health facility, as compared with 21% and 20%, respectively, of births to rural women. Mothers’ educational status is highly correlated with whether their deliveries are assisted by a skilled provider and whether they are delivered in a health facility. 17% of births to mothers with no education were assisted by a skilled provider and 16 percent were delivered in a health facility, as compared with 93% and 92%, respectively, of births to mothers with more than a secondary education. A similar relationship is observed with household wealth.6
In addition, studies conducted in different regions of Ethiopia indicated that maternal education family size, husband occupation and education were all significantly associated with health facility delivery.16 Likewise, the study conducted in Indonesia, mother’s educational attainment was the strongest significant determinant for the use of a skilled attendant .The use facilities and/or trained providers for obstetric complications were positively associated with women’s and their husband’s education.17 Many studies conducted in north west Ethiopia indicated that mothers with lower age at first pregnancy, having more than one previous pregnancies, with in more than one birth order, received ANC service, birth complications in previous and immediate pregnancies and had every used professionally assisted delivery in preceding delivery were commonly found to be significantly associated with safe delivery service utilization.18
Studies have shown that antenatal care service utilization is independent predictor of utilization of institutional delivery. Mothers making one or more ANC visits were more likely to use delivery care service. This might be due to advice from healthcare workers during antenatal care increases a woman’s use of institutional delivery. The healthcare workers could provide good information regarding safe health care delivery and encourage women to deliver at health facility. A previous study in Ethiopia found that proper counseling and advice to deliver at health care facility increased institutional delivery.19
A study in Cambodia indicated that delivery with skilled attendant at the preceding delivery was a significant determinant for subsequent use of skilled attendant. Once a woman has delivered with the aid of an unskilled attendant, she is five to seven times less likely to seek skilled help than a primipara.20 Maternal parity is an independent predictor of utilization of delivery care services in rural Ethiopia, women with parity 1 were more likely to give birth at health care facility than multiparous women. The possible explanation for the low utilization of delivery care services among multiparous women could be because they feel more confident and perceive that there is no need for institutional delivery due to the experience and knowledge from previous pregnancies and births.21
Study conducted in southern Ethiopia showed that Mothers with the age range of 15-19 yrs were about five times more likely to give birth at health facility, Women had not attended the primary education were about 19% less likely to attend skilled delivery, women married to husbands those completed secondary school were about fifteen times more likely to give birth at heath facility than those uneducated, mother who had received less than four antenatal care were 43% less likely to utilize skilled birth attendances, mothers who had ever given birth at least once earlier in health facility tended to utilize skilled delivery services 6.70 times more likely than those who had not and Women those had known the risk of giving birth at home were seven times more likely to utilize skilled birth attendances than their counter parts.22
Study conducted in Bahir Dar, Ethiopia showed that Mothers who gave birth at home have different reasons 46% of them think giving birth at health facility has no necessity, 33% of mothers said the service at health facility is not customary, 21% of the mother said that the health facility was either too far or that they did not have transportation. Urban woman were more likely than rural women to report that health facility deliveries are not necessary (64% versus 45%). But rural women were more likely to report that facility deliveries are not customary (33% versus 21%), or that health facilities were too far or they had no transportation (22% versus 15%).23 Regardless of the government’s efforts to expand health service facilities and promote institutional delivery service in Ethiopia, about 85% of births still take place at home.24 Increased number of home deliveries was common in the rural community than urban births (63% versus 10%) and maternal mortality ratio is 676 per 100,000 live births in Ethiopia.25
Increasing institutional delivery is an important intervention to reduce maternal and children mortality and morbidity especially in lower income countries, however in Ethiopia most of the mother give birth at home. For example in Ethiopia the prevalence of live births delivered by a skilled provider was 28% and the prevalence of institutional delivery was 26% in the 2016 EDHS. This is much lower in the rural communities 21% of births were assisted by a skilled provider and 20% were delivered in a health facility.6, 26, 27
In Ethiopia, studies addressing determinants of maternity care services utilization were limited particularly in Gamo Gofa zone. Additionally, little is known about the determinants of utilization of skilled birth attendances services in the study area. Therefore this study was designed to fill these discrepancies by assessing the determinants of utilization of skilled birth attendances among women in childbearing age at rural villages in Chencha district Gamo Gofa Zone, Southern Ethiopia. The study findings will have input on maternal health improvement in the region as well as in the study area. The findings will also be used by responsible bodies who work on reproductive health services to address issues of reducing maternal morbidity and mortality (Figure 1).
Study area and period
The study was conducted in Chencha district from December 01 to 30, 2016. The district is one of the 15 districts in Gamo Gofa zone, Southern Nations and Nationalities Regional State. Based on projection from the 2007 E.C population and housing Census the woreda is estimated to be 142,063. The district has 48 kebeles; 3 town administration namely Chencha town, Ezzo town and dorze town which constitute about 14% of the woreda population and the remaining 86% of the population resides in the rural community.
Study design
A community based quantitative cross-sectional study design was employed.
Source& study population
Source population: All women in childbearing age who were permanent residents at least for one year in the study area.
Study population: All women in childbearing age that had given birth in the five years before the survey residing in randomly selected kebeles.
Study subjects: Women of childbearing age those had given birth in the past five years preceding the study period proportionally allocated in selected kebeles.
Sample size determination and sampling technique/sampling procedure:
Sample size determination and sampling technique: In the survey, multistage sampling technique was used. The following assumption and formula were considered in calculating the size of the sample. Proportion (p=26.8%) from study conducted in Sidama Zone”(22), at 95% confidence interval, 10% non-response rate and a design effect of 1.5 were considered. Finally, 500 sample women of childbearing age were drawn. The sample was calculated using single Population proportion formula.
N= 333; The Final sample size = 498.2 ≈ 500
Where N, sample size of women who gave birth at health institution by skilled attendants; Zα/2, is the corresponding Z value to 95% significance level = 1.96; P, Proportion of women who had given birth at health facilities by skilled attendants =26.8%; d, degree of freedom=5%.
Sampling procedure
Among forty five rural kebeles in the woreda five rural kebeles were selected randomly. From the selected kebeles, households with women who had given birth in last five years preceding the survey were identified by using the registration at health post. The total sample size had been then proportionally allocated from total women of childbearing age in each kebele. In cases where a woman had given birth more than once, the most recent pregnancy was considered for the present study. Based on this, a sampling frame that enlists all eligible mothers had been prepared and 500 women were included in the study using probability sampling technique (Figure 2).
Eligibility criteria
Inclusion criteria: Reproductive age women who are residing in the study area for at least one year and have given birth within five years preceding the survey.
Exclusion criteria: Women who were mentally and physically non-capable and unwilling to participate.
Variables of the study
Dependent variable: Utilization of skilled birth attendance (SBA) services.
Data collection procedure
Face-to-face interview with semi- structured questionnaire that was adapted from Ethiopian demographic and health survey and related thesis works. Women in the age range of childbearing had been interviewed by going house to house in the randomly selected kebeles. The English version of the questionnaire was translated in to a local language, Gamogna, by experts and translated back English for Consistency. Three health professionals holding diploma, who were fluent speakers of the language and who were working outside the health center of that catchment kebeles were recruited and oriented for one day by the principal investigator prior to data collection. One data collector was assigned per kebele. One supervisor with health background holding first degree was assigned per kebele in order to supervise and assist data collection process. Mothers who were not present during first visit had been revisited twice and the result of visiting was recorded on the tool.
Data quality management
The questionnaire was pre tested on 5% of the respondents in Doko shaye village that was randomly selected for this purpose. The kebele is similar with socio demographic characteristics with the people in the study areas. Findings had been discussed among data collectors and supervisors and tool was amended before actual data collection based on findings of pre-test. Data quality had been ensured during collection, coding, entry and analysis. During data collection, adequate orientation and follow up had been provided to data collectors and supervisors. Supervision of data collectors included observation of how the data collectors were going to administering questions. Supervisors checked the filled questionnaires on a daily basis for completeness, clarity. Then, the principal investigator had double-checked randomly the questionnaire for the completion each day.
Data processing and analysis
Finally, the data had first been checked manually for completeness then recoded, edited and entered into Epi data version 3.1 and exported to SPSS version 20.0 for further analysis. The data had further been cleaned by visualizing, calculating frequencies and sorting. After exploration, bivariate and multivariate analyses had been computed. The bivariate analysis using logistic regression was done to see the crude association between dependent and independent variable so that used to select the candidates for multivariate analysis if the “p” value is <0.05. The strength of association between dependent and independent variables (covariates) was expressed in odds ratio (OR). Finally, multivariate analysis using backward stepwise multiple logistic regression technique had been done to evaluate independent effect of each variable on skilled attendance service utilization by controlling the effect of other confounders.
Operational definitions
Ethical consideration
Ethical clearance was obtained from institutional Review Board of Arba Minch College of Health Sciences. Permission letters to conduct the study was obtained from south nation nationalities and people region health bureau, Gamo Gofa zone health department, Chencha woreda health office and respective kebele administrations. Aim of the study was explained, informed written consent had been obtained from each participant. Confidentiality was maintained by using codes that is only known by the respondent. Participants who were unwilling to participate in the study and those who wanted to abstain from their participation at any stage were informed to do so without any restriction.
Socio-demographic characteristics of the respondents
There are 500 women who had children less than 5 years old were participated in this study. Majority of participants 356(71.2%) were in the age group of 26-30 years with Mean age of 27.44±(3.076) years ranging from 20-37 years. Most of participants 454(90.8%), 464(92.8%) were Gamo by ethnicity and married respectively. Regarding religion more than one half 262(52.4%) was protestant followed by orthodox 190(38.0%). Concerning educational status one half 252(50.4%) of mothers were illiterate and less than one forth 116(23.2%) of fathers were illiterate. With regard to Majority 336(67.2%) of respondents have family size of 1-5 and Mean family size 4.87±(1.315) Years, ranging from 3-9. More than one quarter 142(28.4%) of respondents earn monthly income of less than 2000 ETB with Mean monthly income of 3121.04±(SD=1697.194) ETB, ranging from 1000-8600 (Table 1).
Socio-demographic characteristics |
Frequency |
Percent |
|
Age category |
15-20 years |
7 |
1.4 |
21-25 years |
69 |
13.8 |
|
26-30 years |
356 |
71.2 |
|
Above 30 years |
68 |
13.6 |
|
Religion |
Orthodox |
190 |
38 |
Protestant |
262 |
52.4 |
|
Muslim |
22 |
4.4 |
|
Catholic |
26 |
5.2 |
|
Ethnicity |
Gamo |
454 |
90.8 |
Gofa |
15 |
3 |
|
Amhara |
17 |
3.4 |
|
Wolayita |
8 |
1.6 |
|
Others |
6 |
1.2 |
|
Marital status |
Married |
464 |
92.8 |
Separated |
29 |
5.8 |
|
Divorced |
7 |
1.4 |
|
Educational status of mother |
Illiterate |
252 |
50.4 |
Completed primary school |
117 |
23.4 |
|
Completed secondary school |
78 |
15.6 |
|
College and University |
53 |
10.6 |
|
Educational status of the father |
Illiterate |
116 |
23.2 |
Completed primary school |
134 |
26.8 |
|
Completed secondary school |
124 |
24.8 |
|
College and University |
126 |
25.2 |
|
Occupational status of Mother |
Housewife |
160 |
32 |
Farmer |
122 |
24.4 |
|
Merchant |
112 |
22.4 |
|
Gov't employee |
61 |
12.2 |
|
Day laborer |
18 |
3.6 |
|
Private employee |
24 |
4.8 |
|
Others |
3 |
0.6 |
|
Occupational status of the husband |
Farmer |
196 |
39.2 |
Merchant |
151 |
30.2 |
|
Government employee |
74 |
14.8 |
|
Private employee |
48 |
9.6 |
|
Daily Laborer |
22 |
4.4 |
|
Retired |
9 |
1.8 |
|
Family size |
5-Jan |
336 |
67.2 |
Above 5 |
164 |
32.8 |
|
Monthly income in ETB |
Less than 2000 |
142 |
28.4 |
2001-3000 |
128 |
25.6 |
|
3001-4000 |
95 |
19 |
|
4001-5000 |
67 |
13.4 |
|
Above 5000 |
68 |
13.6 |
|
Table 1 Frequency distribution of Socio-demographic characteristics of Mothers having children less than 5 years in Chencha District, Southern Ethiopia, December 2016 (n=500)
Obstetric characteristics of the respondents
Majority 376(75.2%) of women had married at age of 20-24 years. mean age of first marriage was 21.3020 ± (2.18457) years, ranging from 17-32 years. Regarding Age at first pregnancy majority 390(78.0%) and mean age at pregnancy was 21.6±2.13192 Years, ranging from 17-32. With regard to outcomes of pregnancy most 469(93.8%) had live birth followed by 14(2.8%) abortion. Among mothers who were pregnant during study period majority 43(79.6%) started ANC follow-up. Most of mothers 470(94.0%) reported that their last pregnancy was planned and most of them reported that they had received ANC service for this pregnancy, however only about one third 147(33.7%) had received ANC service for times. Majority 348(69.6%) had delivered their last baby in home with most common mode of delivery being spontaneous vaginal delivery 457(91.4%). Regarding knowledge and attitude of the mother 291(58.2%) and 379(75.8%) had adequate knowledge about institutional delivery and positive attitude about it respectively (Table 2).
Obstetric characteristics of the respondents |
Frequency |
Percent |
|
Age at marriage |
14-19 years |
101 |
20.2 |
20-24 years |
376 |
75.2 |
|
25-30 years |
23 |
4.6 |
|
Age at first pregnancy |
14-19 years |
81 |
16.2 |
20-24 years |
390 |
78 |
|
25-34 years |
29 |
5.8 |
|
Outcomes of pregnancy |
Live birth |
469 |
93.8 |
Abortion |
14 |
2.8 |
|
Still birth |
8 |
1.6 |
|
Died within seven days |
6 |
1.2 |
|
Died b/n 7 days and birth |
3 |
0.6 |
|
Are you pregnant now |
Yes |
54 |
10.8 |
No |
446 |
89.2 |
|
How old is your pregnancy in months now (n=54) |
1-3 months |
16 |
29.6 |
4-6 months |
32 |
59.3 |
|
Above 6 months |
6 |
11.1 |
|
Have you started ANC follow-up (n=54) |
Yes |
43 |
79.6 |
No |
11 |
20.4 |
|
When was the last pregnancy in year |
Less than one year |
54 |
10.8 |
1 year |
338 |
67.6 |
|
2 years |
82 |
16.4 |
|
3 years |
20 |
4 |
|
4 years |
6 |
1.2 |
|
Was last pregnancy planned |
Yes |
470 |
94 |
No |
30 |
6 |
|
Did you receive ANC care |
Yes |
442 |
88.4 |
No |
58 |
11.6 |
|
Frequency of ANC visit (n=442) |
Once |
43 |
9.7 |
Twice |
56 |
12.7 |
|
Three times |
194 |
43.9 |
|
Four times |
149 |
33.7 |
|
Place of delivery of last baby |
Home |
348 |
69.6 |
Health Facility |
152 |
30.4 |
|
Mode of last delivery |
Spontaneous vaginal delivery |
457 |
91.4 |
Instrumental delivery |
8 |
1.6 |
|
Caesarean section |
35 |
7 |
|
Who assisted you in last delivery |
Physician |
26 |
5.2 |
Midwifery |
106 |
21.2 |
|
Nurse |
20 |
4 |
|
TBA |
348 |
69.6 |
|
Condition of last baby |
Live birth |
468 |
93.6 |
Live birth but died soon after birth |
23 |
4.6 |
|
Still birth |
9 |
1.8 |
|
Did you faced Health problem faced During Labor & delivery |
Yes |
26 |
5.2 |
No |
474 |
94.8 |
|
Table 2 Frequency distribution of Obstetric characteristics of the respondents of Mothers having children less than 5 years in Chencha District, Southern Ethiopia, December 2016
Regarding reported reasons of why mothers prefer home delivery majority 138(39.7%) reported previous home delivery was normal, 121(34.8%) reported labor was small and short, 36(10.3%) they were told that there pregnancy was normal and 21(6.0%) lack of transport and presence of traditional birth attendants (Figure 3).
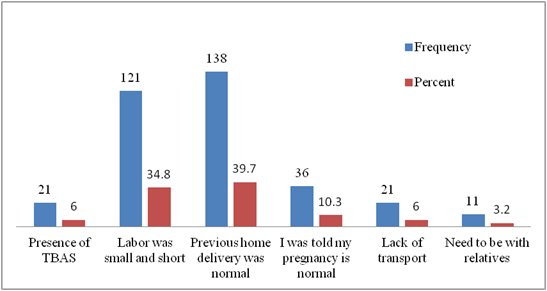
Figure 3 distribution of client related factors why mothers prefer home delivery in Chencha District, Southern Ethiopia, December 2016 (n=348).
Regarding health facility related factors why mothers prefer to give birth at home were 154(44.3%) health facility is too far, 146(42.0%) poor quality service, 32(9.2%) no female provider at health facility and 16(4.6%) unwelcoming approach of health care providers (Figure 4).
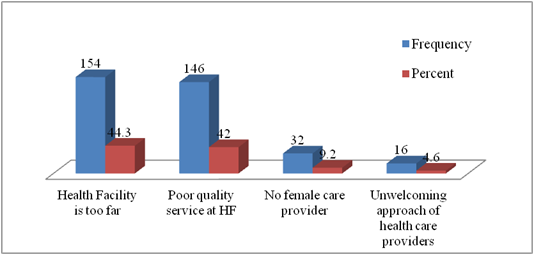
Figure 4 Distribution of health facility related factors why mothers prefer to give birth at home in Chencha District, Southern Ethiopia, December 2016 (n=348).
Concerning reasons why mothers give birth at health facility more than one third 37.0% reported need better service, 28% reported previous better outcome in health facility delivery, 14% difficult labor and 7.0% bad outcome with previous home delivery (Figure 5).
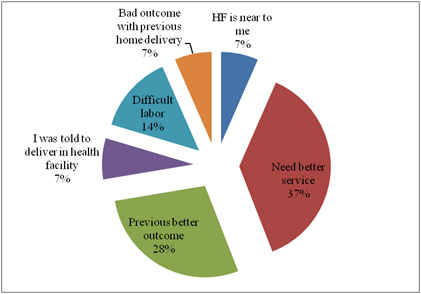
Figure 5 Distribution of Reasons why mothers prefer give birth at health facility in Chencha District, Southern Ethiopia, December 2016 (n=152).
Concerning Health problem faced During Labor & immediately after delivery the most common problem were 8(30.8%), 6(23.1%), 3(11.5%) and 3(11.5%) retained placenta, prolonged labor, mal-presentation and excessive vaginal bleeding respectively (Figure 6).
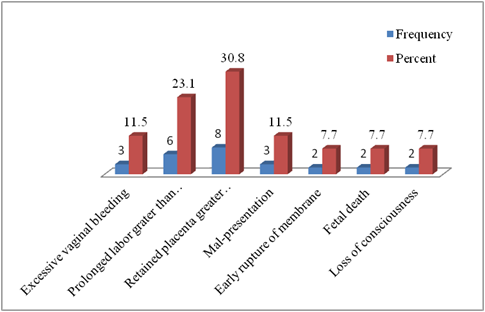
Figure 6 Health problem faced During Labor & immediately after delivery in Chencha District, Southern Ethiopia, December 2016 (n=26).
Regarding the birth order the last pregnancy of 193(39.0%), 170(34.0%), 118(23.0%) and 19 (4.0%) of mothers was third, fourth and above, second and first respectively (Figure 7).
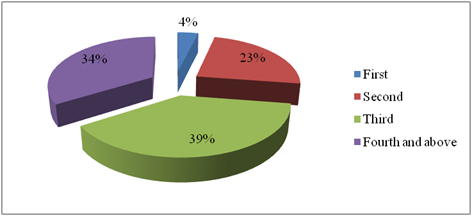
Figure 7 Birth order of the last baby in Chencha District, Southern Ethiopia, December 2016 (n=500).
Knowledge about pregnancy, labor and delivery service
Mothers were asked a series of questions regarding their knowledge about pregnancy, labor and delivery service and most of them 446(89.2%) reported that they know health risks associated with pregnancy, more than one half 291(58.2%) know danger signs of pregnancy, 295(59.0%) know danger signs of labor, 387(77.4%) reported having birth at home has associated risks and they also reported that having birth at health facility has associated benefit. Regarding risks associated with risks during pregnancy about one half 214(48.0%) reported pregnancy related disease, 157(35.2%) reported maternal death and 75(16.8%) fetal death. Concerning reported danger signs leakage of amniotic fluid without labor 57(19.6%), swelling of leg/face 46(15.8%) followed by increased BP 37(12.7%) and 34(11.7%) severe headache and excessive weight gain. With regard to reported danger signs of labor, prolonged labor greater than 12 hrs 70(23.7%), Increased BP 65(22.0%) followed by convulsion 35(11.9%) and Mal-presentation 35(11.9%). Among reported benefits of giving birth at Health facility early detection of problems 89(23.0%), low maternal mortality 69(17.8%) followed by low maternal exhaustion 64(16.5%). Overall knowledge of mother about pregnancy, labor and delivery service was adequate 291(58.2%) and poor for 209(41.8%) (Table 3).
Knowledge about pregnancy, labor and delivery service |
Frequency |
Percent |
|
Awareness of health risk during pregnancy |
Yes |
446 |
89.2 |
No |
54 |
10.8 |
|
If yes what are risks (n=446) |
Pregnancy related disease |
214 |
48 |
Maternal Death |
157 |
35.2 |
|
Fetal death |
75 |
16.8 |
|
Knowledge on danger signs of pregnancy |
Yes |
291 |
58.2 |
No |
209 |
41.8 |
|
If yes what are danger signs (n=291) |
Swelling of leg/face |
46 |
15.8 |
Vaginal bleeding |
26 |
8.9 |
|
Reduced fetal movement |
28 |
9.6 |
|
Severe headache |
34 |
11.7 |
|
Severe abdominal cramp |
29 |
10 |
|
Excessive weight gain |
34 |
11.7 |
|
Increased BP |
37 |
12.7 |
|
Leakage of amniotic fluid without labor |
57 |
19.6 |
|
Do you know danger signs of labor |
Yes |
295 |
59 |
No |
205 |
41 |
|
If yes what are danger signs of labor (n=295) |
Prolonged labor greater than 12hrs |
70 |
23.7 |
Early rupture of membrane |
25 |
8.5 |
|
Vaginal bleeding |
20 |
6.8 |
|
Placental retention greater than 1hr |
10 |
3.4 |
|
Mal-presentation |
35 |
11.9 |
|
Increased BP |
65 |
22 |
|
Convulsion |
35 |
11.9 |
|
Abdominal pain |
35 |
11.9 |
|
Giving birth at home has risks |
Yes |
387 |
77.4 |
No |
113 |
22.6 |
|
If yes what do you know (n=387) |
Maternal exhaustion |
64 |
16.5 |
Fetal distress |
113 |
29.2 |
|
Maternal death |
89 |
23 |
|
Fetal/neonatal death |
58 |
15 |
|
Postpartum morbidity |
41 |
10.6 |
|
Disease transmission from attendants |
22 |
5.7 |
|
Is there any benefit in giving birth at Health facility |
Yes |
387 |
77.4 |
No |
113 |
22.6 |
|
If yes what are they (n=387) |
Early detection of problems |
89 |
23 |
Early treatment of problems |
47 |
12.1 |
|
Lower maternal exhaustion |
64 |
16.5 |
|
Better newborn care |
43 |
11.1 |
|
Lower maternal mortality |
69 |
17.8 |
|
Low postpartum morbidity |
75 |
19.4 |
|
Overall Knowledge on pregnancy, labor and delivery service |
Adequate Knowledge |
291 |
58.2 |
Poor Knowledge |
209 |
41.8 |
|
Table 3 Frequency distribution of Mothers Knowledge about pregnancy, labor and delivery service in Chencha District, Southern Ethiopia, December 2016 (n=500)
Knowledge, Labelled to have adequate Knowledge if they correctly responded all questions designed to access knowledge about pregnancy, labor and delivery.
Attitude about pregnancy, labor and delivery service
Mothers were asked series of questions concerning their perception about pregnancy, labor and delivery complications and majority reported that complication of labor were preventable and treatable 380(76.0%) and 439(87.9%) respectively. most of respondents 400(80.0%) reported that every women were at risk of developing pregnancy complication. Over all attitude of mothers about pregnancy, labor and delivery was positive for 379(75.8%) and negative for 121(24.2%) (Table 4).
Attitude about pregnancy, labor and delivery service |
Attitude score |
|
Positive (1) |
Negative (0) |
|
Do you think most complications of labor were preventable |
380(76.0%) |
120(24.0%) |
Do you think most complications of labor where treatable |
439(87.8%) |
61(12.2%) |
Any pregnant women are at risk for developing delivery complications |
400(80.0%) |
100(20.0%) |
Delivery complications are hazardous to maternal health |
458(91.6%) |
42(8.4%) |
Delivery complications are risk for newborn |
412(82.4%) |
88(17.6%) |
Skilled birth attendance is important for my wellbeing |
434 (86.8%) |
66(13.2%) |
Skilled birth attendance is important for new born baby |
382 (76.4%) |
118(23.6%) |
Table 4 Frequency distribution of Mothers Attitude about pregnancy, labor and delivery service in Chencha District, Southern Ethiopia, December 2016 (n=500)
Note: Very agree and Agree were labeled as positive and assigned value “1” and Disagree and very disagree were labeled as negative attitude and assigned value “0”. The Overall Attitude was considered positive if all questions were assigned value “1” and respondents were labeled to negative attitude if any of questions is assigned “0.
Social and Health system factors and women decision-making
Most of mothers reported that they decide on utilization of health service and place of delivery 349(69.8%) and 312(62.4%) respectively. Concerning health system related factors majority of respondents 363(72.6%), 337(67.4%), 320(64.0%) and 180(36.0%) reported that Health professionals are skilled enough, The facility is well equipped to provide service, distance from health facility was greater than 5km and nearby health facility was health center respectively (Table 5).
Social factors |
Frequency |
Percent |
|
Who decides your health service utilization |
Self |
349 |
69.8 |
Husband |
137 |
27.4 |
|
Relatives |
14 |
2.8 |
|
Who decides your place of childbirth |
Self |
312 |
62.4 |
Husband |
132 |
26.4 |
|
Relatives |
43 |
8.6 |
|
Religious leader |
13 |
2.6 |
|
Health system factors |
|||
Health professionals are skilled enough |
Yes |
363 |
72.6 |
No |
137 |
27.4 |
|
The facility is well equipped to provide service |
Yes |
337 |
67.4 |
No |
163 |
32.6 |
|
Distance of nearby Health facility in Km |
Less than 5 km |
180 |
36 |
Greater than 5 km |
320 |
64 |
|
Types of nearby health facility |
Health post |
160 |
32 |
Hospital |
160 |
32 |
|
Health center |
180 |
36 |
|
Table 5 Frequency distribution of social and system factors associated with pregnancy, labor and delivery service in Chencha District, Southern Ethiopia, December 2016 (n=500)
Factors associated with skilled birth attendance
Binary logistic regression was done to identify association between skilled birth attendance utilization and independent variables and variables that have shown statistical significance at P-value less than 0.05 were entered into multinomial logistic regression to rule out confounders and identify independent predictors of skilled birth attendance utilization practice. Age of the mother 21-25 years were 1.5 times [AOR=1.56 (1.204-3.516) more likely to deliver their babies in health facility than those above 30 years of age, Mothers with government employed husband were 1.6 times [AOR=1.669 (1.475-81.642) more likely more likely to deliver their babies in health facility than farmers, mothers with monthly income above 5000 ETB were 2 times [AOR=2.196 (1.051-4.590) more likely to deliver their babies in health facility than those earing below 200 ETB per month, Mothers with no ANC follow-up were less [AOR=0.915 (0.375-0.953) likely to deliver in health facility than those who have ANC follow-up, Mothers with four times ANC visit were 5 times more [AOR=5.615 (1.851-17.040) likely to deliver in health facility than those with one time follow-up, Mothers who reported health professionals are not well skilled were less [AOR=0.227 (0.085-0.607) likely to deliver in health facility than those who reported professionals are well skilled, Mothers with nearest health facility in less than 5 km distance were 3 times more [AOR=3.116 (1.916-5.068) likely to deliver in health facility than those with more than 5km distance (Table 6).
Modern contraceptive use a |
Place of delivery of last baby in 5yrs |
COR |
95% CI for AOR |
AOR |
95% for AOR |
P value b |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Home (n=348 ) |
Health Facility (n=152) |
LB |
UB |
LB |
UB |
||||||||
Frequency |
Percent |
Frequency |
Percent |
||||||||||
Home |
Age of the respondent |
15-20 years |
5 |
1.4 |
2 |
1.3 |
1.3 |
0.23 |
7.354 |
0.6 |
0.083 |
4.322 |
0.767 |
21-25 years |
39 |
11.2 |
30 |
19.7 |
2.5 |
1.199 |
5.215 |
1.56 |
1.204 |
3.516 |
.015* |
||
26-30 years |
252 |
72.4 |
104 |
68.4 |
1.341 |
0.732 |
2.456 |
0.772 |
0.348 |
1.712 |
0.342 |
||
Above 30 years |
52 |
14.9 |
16 |
10.5 |
0.947 |
0.229 |
3.911 |
||||||
Occupation of the husband |
Farmer |
133 |
38.2 |
63 |
41.4 |
1 |
- |
- |
1 |
- |
- |
- |
|
Merchant |
101 |
29 |
50 |
32.9 |
1.364 |
0.316 |
5.881 |
0.719 |
0.07 |
7.361 |
0.989 |
||
Government employee |
44 |
12.6 |
30 |
19.7 |
0.133 |
0.022 |
0.817 |
1.669 |
1.475 |
81.642 |
.019* |
||
Private employee |
45 |
12.9 |
3 |
2 |
0.316 |
0.05 |
1.998 |
6.226 |
0.064 |
7.013 |
0.677 |
||
Daily Laborer |
19 |
5.5 |
3 |
2 |
0.947 |
0.229 |
3.911 |
1.76 |
0.133 |
23.339 |
0.221 |
||
Retired |
6 |
1.7 |
3 |
2 |
0.99 |
0.238 |
4.124 |
0.534 |
0.053 |
5.378 |
0.94 |
||
Monthly income |
Less 2000 ETB |
103 |
29.6 |
39 |
25.7 |
1 |
- |
- |
1 |
- |
- |
- |
|
1000-3000 birr |
86 |
24.7 |
42 |
27.6 |
0.657 |
0.358 |
1.204 |
1.448 |
0.689 |
3.042 |
0.174 |
||
3001-4000 birr |
74 |
21.3 |
21 |
13.8 |
0.382 |
0.193 |
0.755 |
1.846 |
0.833 |
4.088 |
0.006 |
||
4001-5000 birr |
46 |
13.2 |
21 |
13.8 |
0.614 |
0.303 |
1.243 |
1.196 |
0.515 |
2.779 |
0.175 |
||
Above 5000 birr |
39 |
11.2 |
29 |
19.1 |
0.509 |
0.278 |
0.933 |
2.196 |
1.051 |
4.59 |
.029* |
||
Did you receive ANC care |
Yes |
316 |
90.8 |
126 |
82.9 |
1 |
- |
- |
1 |
- |
- |
- |
|
No |
32 |
9.2 |
26 |
17.1 |
0.491 |
0.281 |
0.857 |
0.915 |
0.375 |
0.953 |
0.012 |
||
Frequency of ANC visit |
Once |
29 |
8.3 |
14 |
9.2 |
1 |
- |
- |
1 |
- |
- |
- |
|
Twice |
51 |
14.7 |
5 |
3.3 |
0.901 |
0.438 |
1.853 |
0.915 |
0.375 |
2.233 |
0.845 |
||
Three times |
139 |
39.9 |
55 |
36.2 |
0.738 |
0.466 |
1.168 |
1.34 |
0.762 |
2.356 |
0.309 |
||
Four times |
97 |
27.9 |
52 |
34.2 |
0.183 |
0.069 |
0.486 |
5.615 |
1.851 |
17.04 |
.002* |
||
Health professionals are skilled enough |
Yes |
238 |
68.4 |
125 |
82.2 |
1 |
- |
- |
1 |
- |
- |
- |
|
No |
110 |
31.6 |
27 |
17.8 |
0.16 |
0.039 |
0.651 |
0.227 |
0.085 |
0.607 |
.003* |
||
Distance from nearest health facility |
Less than 5 km |
145 |
41.7 |
35 |
23 |
0.419 |
0.271 |
0.646 |
3.116 |
1.916 |
5.068 |
0.000* |
|
Greater than 5 km |
203 |
58.3 |
117 |
77 |
1 |
- |
- |
1 |
- |
- |
- |
||
Table 6 Multivariable logistic regression of factors predicting the likelihood of modern family planning method utilization among reproductive age women at Arba Minch town, Southern Ethiopia, 2017, (n=500)
a 95% Confidence Interval for place delivery
b P-value between groups significant at the 0.05 level
This study revealed the status and independent predictors of skilled birth attendance by rural mothers in Chencha district, Gamo Gofa zone southern Ethiopia. The point prevalence of institutional delivery was 152(30.4%) and Majority 348(69.6%) had delivered their last baby in home with most common mode of delivery being spontaneous vaginal delivery 457(91.4%). This is higher than study conducted in southern Ethiopia showed that the prevalence of skilled birth attendance was 148(26.8%) (22) and findings from other rural communities Ethiopia For example 21% of births to rural mothers were assisted by a skilled provider and 20% were delivered in a health facility.6 However this is lower than study conducted in North West Ethiopia showed that 38.2 % of women gave birth in health facilities for their most recent birth while the most 223 (61.8%) delivered at home.14 The variation could be explained by difference in socio-demographic variables among study participants and difference in tools used by researchers.
This study showed that mothers knowledge about pregnancy, labour and delivery was adequate for the 291(58.2%) of them. However knowledge of mothers was not associated with skilled birth attendance. This could be due others factors deterring the use skilled birth attendance like maternal age, monthly income, occupation, skill of professionals and distance from health facility. This study revealed that the major reasons why mothers give birth at health facility include; 37.0% need better service, 28% previous better outcome in health facility delivery, 14% difficult labor and 7.0% bad outcome with previous home delivery. This is similar to findings from north west Ethiopia showed that major reasons of institutional delivery were fear of complications (77.5%), to get better service (56.5%) safe and clean delivery (46.4%) and they were communicated to deliver at health facilities during ANC attendance, 47(35.5%).14
Age of the mother 21-25 years were 1.5 times [AOR=1.56 (1.204-3.516) more likely to deliver their babies in health facility than those above 30 years of age. This in line with findings from different studies conducted in north west Ethiopia indicated that mothers with lower age at first pregnancy, having more than one previous pregnancies, with in more than one birth order, received ANC service, found to be significantly associated with safe delivery service utilization.18 Study conducted in southern Ethiopia showed that Mothers with the age range of 15-19 yrs were about five times more likely to give birth at health facility.22 This could be due to improved access to reproductive health information for young generation through Medias like, TV, radio or internet than those old aged mothers.
Mothers with government employed husband were 1.6 times [AOR=1.669 (1.475-81.642) more likely more likely to deliver their babies in health facility than farmers. This is in line with studies conducted in different regions of Ethiopia indicated that maternal education family size, husband occupation and education were all significantly associated with health facility delivery.16 Mothers with monthly income above 5000 ETB were 2 times [AOR=2.196 (1.051-4.590) more likely to deliver their babies in health facility than those earing below 200 ETB per month.This is in line with EDHS findings household wealth status is highly correlated with whether their deliveries are assisted by a skilled provider and whether they are delivered in a health facility.6 This could be due to increased wealth of family could help other factors hindering institutional delivery like distance from health facility by that they can pay transportation cost to get ANC service or attend delivery in health facility.
Mothers with no ANC follow-up were less [AOR=0.915 (0.375-0.953) likely to deliver in health facility than those who have ANC follow-up, Mothers with four times ANC visit were 5 times more [AOR=5.615 (1.851-17.040) likely to deliver in health facility than those with one time follow-up. This similar with findings from Study conducted in North West Ethiopia showed that mothers who received ANC service, birth complications in previous and immediate pregnancies and had every used professionally assisted delivery in preceding delivery were commonly found to be significantly associated with safe delivery service utilization (18). Antenatal care service utilization is independent predictor of utilization of institutional delivery. Mothers making one or more ANC visits were more likely to use delivery care service. This might be due to advice from healthcare workers during antenatal care increases a woman’s use of institutional delivery. The healthcare workers could provide good information regarding safe health care delivery and encourage women to deliver at health facility. A previous study in Ethiopia found that proper counseling and advice to deliver at health care facility increased institutional delivery.19
Mothers who reported health professionals are not well skilled were less [AOR=0.227 (0.085-0.607) likely to deliver in health facility than those who reported professionals are well skilled. This is similar with study in Cambodia indicated that delivery with skilled attendant at the preceding delivery was a significant determinant for subsequent use of skilled attendant. Once a woman has delivered with the aid of an unskilled attendant, she is five to seven times less likely to seek skilled help than a primipara.20 Mothers with nearest health facility in less than 5 km distance were 3 times more [AOR=3.116 (1.916-5.068) likely to deliver in health facility than those with more than 5km distance. This similar with findings from Bahir Dar, Ethiopia showed that Mothers who gave birth at home have different reasons 46% of them think giving birth at health facility has no necessity, 33% of mothers said the service at health facility is not customary, 21% of the mother said that the health facility was either too far or that they did not have transportation. Rural women were more likely to report that facility deliveries are not customary 33%, health facilities were too far or they had no transportation 22%.23
In conclusion this study revealed that prevalence of skilled birth attendance below one third. ANC visit for four and more times low, Mothers knowledge about pregnancy, labour and delivery was low. Age of the mother 21-25 years, Mothers with government employed husband, mothers with monthly income above 5000 ETB, Mothers with ANC follow-up, Mothers with four times ANC visit, Mothers who reported health professionals are not well skilled and Mothers with nearest health facility in less than 5 km distance were predictors of skilled birth attendance utilization.
Strengths and limitations of the study
Strengths: Random sampling technique was employed. i.e., random selection of the Villages, Data collectors speaks local languages and was the same sex with study subjects to minimize information biases and Standardized questionnaire based on similar studies.
Limitations: The study design was cross-sectional and determinants of skilled birth attendance cannot assessed, there could be recall bias, since the women were asked for events within the last one year prior to the survey.
Recommendations: Based on the findings of this study, the following specific recommendations were made to respective bodies.
To health care providers:
To woreda health sector officials
To community: Community leaders should encourage health facility visit during pregnancy, labour and delivery and discourage involvement of traditional birth attendants on delivery assistances.
Contribution of researcher
Mende Mensa: is a senior researcher who conceived the study and prepared the proposal; analyzed the data and presented the work for responsible bodies analyzed and interpreted the findings of this study and he also prepared this document for publication. Melkenesh Nigatu has participated in data entry and analysis.
Above all our thanks go to Almighty God, Who provided us time, health and endurance to conduct this study. We would like to express our deepest gratitude to our friends Mr. Habitamu Samuel (Health officer, Coordinator of research and publication core process owner), for his unreserved help during analysis, interpretation of statistical data and the writing of final paper. Our appreciation also goes to all staffs of Arba Minch college health Sciences for their unreserved support throughout the course and final thesis writing. Our heartfelt gratitude and thanks to staffs of Gamo Gofa Zone health department, Chencha district council and health office and mothers participated in this study for offering us all necessary materials and vital information during data collection and writing final thesis . Really, we are very grateful for your whole rounded support. Thank you very much! We are heartily thankful to our children, Kalkidan and Mikiyas and all other family members and friends for their continuous encouragement, moral and material support throughout this research work. Your closeness was very vital for our success. Really, I am proud of you!
We have no conflict of interest during conducting this study or developing the manuscript. All expenses regarding this paper were from out of pocket of the researchers.

©2019 Mensa, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.