MOJ
eISSN: 2475-5494


Case Report Volume 8 Issue 6
Department of obstetrics gynecology unit, Pikine National Hospital, Senegal
Correspondence: Moussa Diallo, Department of obstetrics gynecology Unit, Pikine National Hospital, located in Thiaroye Camp, Dakar, Senegal, Tel 338530071
Received: November 03, 2019 | Published: November 26, 2019
Citation: Tall A, Diallo M, Diouf AA, et al. Case report of spontaneous bilateral tubal ectopic pregnancy in the National Hospital of Pikine, Dakar. MOJ Women’s Health. 2019;8(6):303-305. DOI: 10.15406/mojwh.2019.08.00254
Ectopic pregnancy still remains an important cause of maternal morbidity and mortality notably because of using assisted reproductive techniques. The diagnosis is usually made intra operatively and levels of serum BHCG and ultrasound has not been useful in the diagnosis of bilateral tubal ectopic pregnancy. This leads to emphasize on the importance of meticulous ultrasound examination when an ectopic pregnancy is suspected but also a complete tubal and abdominal examination at the time of surgery even if there may be issues with significant adhesive disease. Conservative treatments like “tubal caesarean,” despite the risk of recurrence, are still very useful in our context because of the inaccessibility of assisted reproductive treatment. Risk factors for ectopic pregnancy have not been found in our case but a research track could be opened on a traditional pharmacopoeia called “ALDANKE” widely used in Senegal.
Keywords: ectopic, bilateral, tubal pregnancy, pharmacopoeia, laparotomy, echography, trans-abdominal, abdomino-pelvic, menstruation, salpingectomy, hemoperitoneum, estro progestative
In the first trimester of pregnancy, ectopic location is one of the important causes of morbidity and mortality. Recently, the incidence of ectopic pregnancy, which was 4.5-16.8 per 1000, has increased because of using assisted reproductive techniques.1 Bilateral tubal pregnancy is a rare disease, which occurs in 1 per 200,000 pregnancies. Its incidence has been reported to be increasing as a result of increased use of induction ovulations.1 However, bilateral tubal pregnancy in the absence of preceding induction of ovulation is a rare condition with an estimated incidence of 1 in 725 to 1 in 1,580 ectopic pregnancies,2 the rarest form of ectopic pregnancy is bilateral tubal pregnancy, which occurs spontaneously. According to the World Health Organization in 2007, 5% of maternal mortality in the developing countries is due to ectopic pregnancies. Hemorrhage and infection cause half of the deaths associated with ectopic pregnancy.3,4 There has been an increase in the number of published case report of bilateral tubal pregnancies following the use of induction ovulation, but spontaneous bilateral unruptured tubal pregnancy remains a rare event and the diagnosis usually is made intra operatively. Here we report a 33-year-old woman referred to the hospital for a heterotrophic pregnancy that underwent another echography showing an ectopic pregnancy and laparotomy finally permitted to diagnose a spontaneous bilateral tubal pregnancy.
A 33-year-old, third gesture, primipara, with one healthy child, referred the January 1st 2019 at 9PM to the National Hospital of Pikine for a heterotrophic pregnancy of 8 weeks without cardiac activity, was admitted with complaints of abdominal pain and slight spotting. She was married for 8 years and is the second wife of a polygamous household, without consanguinity with the husband and with a regular cohabitation. She had a history of injectable contraception use stopped 2years before. There was no history of repetitive sexually transmitted infections or previous abdomino pelvic surgery and use of induction ovulation drugs. The patient reported having taken a decoction based on "Typhi" more known in Senegal under the name of "ALDANKE" at the end of her last menstruation there was 3months. The antecedent of twinning had not been found in the family.
The symptomatology was a week before her admission marked by abdomino pelvic pain and slight spotting that led her to consult in a private clinic that referred her for the management of a heterotrophic pregnancy. General examination revealed pulse rate 89/min, blood pressure118/82 and a good general condition without pallor. Her abdomen was supple on palpation, right lower quadrant and hypogaster with positive rebound tenderness. On pelvic examination, there was spotting, the uterus was bulky and both adnexal were tender on palpation with brownish losses. Trans-abdominal ultrasound revealed a right adnexal mass suggestive of an ectopic pregnancy, uterine cavity with a gestational pseudo-sac appearance and an average amount of fluid was seen in the pelvis (Figure 1). Hematological evaluation showed, platelets count 254 000/mm3, hemoglobin 11,5g/dl, prothrombin 100% and bHCG was 55000IU/l, because of a report of fluid in pelvis with a high rate of BHCG, emergency laparotomy was performed. The patient was under spinal anesthesia, the skin incision was Pfannenstiel type.
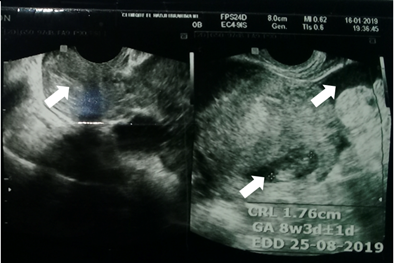
Figure 1 Ultrasound aspects: Left image: arrow showing the uterine emptiness line. Right image: arrow showing a juxta-uterine gestational sac and a hemoperitoneum.
The investigation revealed an ongoing tubal-abdominal abortion on the right and an unruptured left ampullary ectopic pregnancy with a slightly enlarged uterus and a hemoperitoneum of about 500cc (Figure 2). The tubal-abdominal expression was first made on the right followed by total anterograde salpingectomy by electro coagulation after failure of a conservative attempt. A salpingotomy was performed on the left with the evacuation of the tubal pregnancy; the hemostasis was satisfactory (Figure 3).
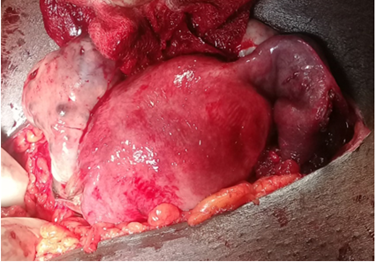
Figure 3 Operative aspects; final image showing total right salpingectomy (white arrow and circle) and left salpingotomy (white arrow).
The histopathologic samples were taken for the 2 ectopic pregnancies, the right salpingectomy specimen and the product of the intrauterine aspiration. Immediate postoperative outcomes were clinically and biologically simple. The patient was put on oral contraception by estro-progestative pill and her exit was performed after 5 days. The bHCG level was 2750IU/ml at day 9 and 36.8IU/I at day 17 and undetectable at day 31 postoperative.
Hysterosal pingography performed at 6months showed a left unilateral tubal permeability, the right Fallopian tube not being visualized (Figure 4).
Bilateral ectopic pregnancy is very rare, making the preoperative diagnosis difficult because it is rarely mentioned despite the sensitivity of ultrasound widely available in the emergency room.
There are three possible explanations for a bilateral ectopic pregnancy:
In our case also preoperative ultrasound failed to demonstrate bilateral tubal ectopic pregnancy. The most common method of diagnosing the second ectopic is direct inspection of contralateral tube in the operating room or laparoscopic examination. The frequency of bilateral ectopic pregnancy has been estimated at 1/200000 uterine pregnancies and 1/725-1/1580 ectopic pregnancies. In the past 20years a 3-fold increase in the incidence has been observed. Heterotypic as well as bilateral tubal ectopic pregnancies are seen after the introduction of assisted reproductive treatment.5,6 The occurrence of spontaneous bilateral ectopic pregnancy is, however, exceedingly rare. Comprehensive clinical guidelines for the treatment of ectopic pregnancy have been published by the Royal College of Obstetricians and Gynaecologists,7 because of its rarity, synchronous ectopic pregnancy is not covered, but the principles of treatment can still be applied. Laparoscopic surgical treatment is preferred to open procedures, because the patient recovers more quickly. Ben Haj Hassine Amine and Siala Haythem8 of Tunis Hospital, in their case report in 2015 did a bilateral salpingectomy. This permit to lower the risk of relapse and fertility still has a very good prognosis because of medical assisted procreation techniques commonly used.
Nayereh Ghomian et al.,9 of Mashdad University in Iran in 2013,7 performed a salpingectomy with a contralateral salpingostomy but no information had been found about the practicality of the conserved Fallopian tube. Andrews et al.,10 reported a bilateral tubal pregnancy that laparoscopic salpingectomy was used in ectopic pregnancy and the patient was subsequently treated with methotrexate because of persistent ectopic pregnancy. Since the diagnosis of bilateral tubal pregnancy is usually made at the time of surgery, there are no case reports of successful primary medical treatment with methotrexate. Our patient, because of her acute symptoms, was not suitable for either laparoscopic surgery or medical management with methotrexate and we chose a conservative method. Indeed, medical assisted procreation notably the in vitro fecundation remains inaccessible for most of Senegalese women and the patient had clearly told us her desire to procreate again notably in a context of polygamy. As for others cases in literature, no major ectopic pregnancy risk factors have been found for our patient. However, a research track could be opened on a traditional pharmacopoeia called “ALDANKE” widely used in Senegal for “cleaning the uterus after the menstruations”. The patient had been taken it. Our case demonstrates once again the importance of thoroughly examining the entire pelvis at the time of exploratory laparotomy undertaken for a suspected ectopic pregnancy. The necessity of carefully examining both the adnexal, as postulated by Sherman et al.,11: “the patient who has had one ectopic pregnancy is at risk of having another in future and also at the same time”.
Ectopic pregnancy is still an important cause of maternal mortality especially in the context of medical assisted procreation use. The diagnosis of bilateral tubal pregnancy is usually made intra-operatively. This underscores the importance of identifying and closely examining both tubes at the time of surgery, even in the presence of significant adhesive disease. The conservative treatment as ‘tubal caesarian’ , helped by a soaked compress with adrenaline for hemostasis in our case, despite important risks of relapse, still remains a common choice in our context because of expensiveness of medical procreation techniques. No ectopic pregnancy risk factors have been found for our patient but a research track could be opened on a traditional pharmacopoeia called “ALDANKE” widely used in Senegal.
To all ours Professors in Obstetrical and Gynecological Clinic in Dakar, in the National Hospital of Pikine and all of the team and fellow students in maternity hospital especially to doyen Diatta, anesthetist assistant.
The author declares that there are no conflicts of interest.
None.

©2019 Tall, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.