MOJ
eISSN: 2475-5494


This case report is about a 43year old patient in Poland who had been pregnant 6times previously and they all ended in spontaneous abortions prior to 20weeks. She had been trying for 15years to become pregnant. She was never given any reasons for the 6 spontaneous abortions by various doctors except she was told “It happens”. This “explanation” sounded very unusual to us. No tests were ever performed on her or her husband and naturally when she stopped trying, she got pregnant. This 7thpregnancy was relatively uneventful except for some hyperemesis gravidarum that started around the 30thweek and the fact that she was high risk due to her advanced age, however, again, no one ever supposedly told her this. She received no special care being such a high risk patient, nor would she tell us who her OB/GYN was, which is very unusual as in Poland, during pregnancies, all visits throughout the 40weeks and delivery results are documented in a book that is given to the patient at the start of the pregnancy. She had no such book and could not explain herself. According to this patient, she was in excellent condition and reported being thin and working out on a regular basis prior to becoming pregnant. She came into the maternity hospital emergency room “feeling strange”. We checked her in the Emergency Room because the nurse couldn’t believe the blood pressure reading she was getting. She was found to have a blood pressure of 200/130 and a pulse of 60, tachypnoea at 40; an obvious case of massive shock and preeclampsia - but why? Also, why such severe bradycardia?? Why this had never been discovered by her primary OB/GYN at her weekly visits is a mystery to her and to us (we suspected no prenatal care, ever), but this was the time to act, not to debate as to why this was happening while the patient died. We also suspected that the patient had been lying to us all along, that she never had any hospital care at all and that simply she had a midwife with each previous pregnancy. It seemed like she just did not want to admit to us the embarrassment of her multiple mistakes.
Keywords: preeclampsia, eclampsia, pregnancy induced hypertension (PIH), hyperemesis gravidarum, placenta previa, abruptio placentae, caesarean section
Such a high blood pressure usually just doesn’t “happen” suddenly. The patient reported that she never knew about any high blood pressure prior to this or during the other 6 pregnancies. We explained to her that we needed to admit her immediately for Pregnancy Induced Hypertension (PIH) that was this high and get this blood pressure under control immediately. We also explained that preeclampsia can lead to eclampsia, a potentially fatal condition. She was very agreeable to this however she did make it very clear to us that she wanted to try to have another child after this child was born. We explained to her that the risks were extremely high for someone with PIH, especially at her age to have it happen again on her next pregnancy and that even regardless of her advanced age for a pregnancy, it was highly likely to happen again, risking both her and the next child’s life. We even explained to her that patients at her age were at extremely high risk of preeclampsia happening again and thus at this age can lose their uterus due to uncontrolled bleeding.
We also explained all the other risk factors, such as genetic problems (Trisomy 21, etc.) but she was insistent that we do everything possible to save her uterus. Due to her being so high risk, we admitted her immediately into the hospital which happened to coincide with her being at exactly 34 weeks gestation (by dates)as she was starting to show signs of preeclampsia and her hyperemesis gravidarum 1 was becoming quite severe, according to her. We wanted to control her fluid ins and outs, watch them closely, she was also showing mild proteinuria so we felt the best place for her was in the hospital where she could be closely watched. She was placed on IV Magnesium Sulfate and on total bedrest.
Preeclampsia2 is defined as a potentially dangerous pregnancy complication characterized by high blood pressure. If uncontrolled, this condition can lead to Eclampsia,2 a life-threatening condition in which one or more convulsions occur in a pregnant woman suffering from high blood pressure, this can often be followed by a coma and posing a serious threat to the health and life of mother and baby.
As reported in the Abstract, we admitted a 43 year old in her 34th week of pregnancy with severe previously undiagnosed pregnancy induced hypertension (PIH)2 and severe bradycardia and hyperemesis gravidarum. Patient had 6 miscarriages previously and was admitted by us through the Obstetrics Emergency Room at 34 weeks of pregnancy. Patient was placed on total bedrest and given IV Magnesium Sulfate to control the high blood pressure. The Magnesium Sulfate worked quite well in controlling her blood pressure, but another problem was discovered during an ultrasound we ordered. The patient had a placenta previa that completely covered the cervical os3 eliminating the chance for any kind on natural birth. The mother was immediately told, explained why it was a problem and was quite disappointed but her only concern was what was best for the child.
At 35 weeks and 5 days, on the 12th day after admission, we were called in the middle of the night that the patient was bleeding quite severely from the vagina. We went and saw the patient immediately, ordered an ultrasound to ascertain that this was not a placental abruption, which usually cannot be differentiated by clinical findings alone from a placenta previa. Patient did not have a placental abruption, but she was still bleeding quite massively so we ordered 4 units of whole blood to be typed and crossed matched, increased her fluids in the meanwhile to keep her blood pressure up, which was falling. I also ordered the OR to prepare for an emergency Caesarean Section.
The Caesarean Section was started 10 minutes after the order was given under general anesthesia, the abdomen was opened by the standard Pfannenstiel approach and the operation type was a laparotomy: sectio caesarea transperitonealis suprapubica transversa. The male child was removed in two minutes and 15 seconds from the time the mother was placed under general anesthesia, he was easily removed by my assistant surgeon and handed off to the neonatologist. The child’s APGAR Score was 9 and 10, and the child was found to weigh 2,100 grams at birth.
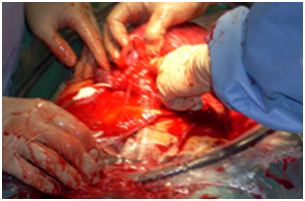
After the delivery is where more problems began. After sweeping the uterus with my hand and removing the placenta, the placenta was checked on a table and it appeared all parts were removed, no excessive tearing, standard 3 vessel umbilical cord and no placental parts were missing. The nurses reported that there was still a large amount of blood coming from the vagina and the patient had already received two units of whole blood during the operation. My surgery assistant, Author #2, has a smaller hand than I do, I asked her to sweep the uterus again and place a finger into the cervix from above and ascertain if she felt anything unusual. She did that and reported everything normal. I also had my assistant surgeon go from below and do a vaginal exam, again no problems were found. After my assistant changed her gown and gloves, she returned to the operating field and we discussed the problem, no arterial or venous bleeders were seen, even under direct visualization of the interior of the uterus under highly bright lights and microscopic 3X glasses. I asked the circulating nurse to get 4 large sterile, bulky gauze rolls and give them to us. We pushed the first gauze roll (unrolled of course down into the cervix and had a nurse from below grab the end with a clamp and leave the clamp in place, for ease of later removal (Figure 1). Also the clamp stayed outside of the vagina, so it wouldn’t get pulled back up into the vagina and uterus. Our plan was to pack the uterus tightly with unrolled bulky gauze (my assistant’s idea and a very good one). My partner continued to unroll and pack the uterus with sterile gauze roll, tying the ends together, making sure we could pull it out later through the vagina. We ended up tying all four rolls together, packing the uterus quite snugly with gauze. The uterus was then closed with a running, 2/0 absorbable suture (Figure 2), the uterus was inspected thoroughly on the exterior surface for any anomalous bleeding, (Figure 3), placed back inside the mother and before we even started closing the skin, the nurses reported a significant decrease in the amount of blood coming out of the vagina. The anesthesiologist reported the blood pressure had stabilized and was coming backdown to a normal range and the pulse was staying steady at 80 beats per minute. The peritoneum, 1.5 cm. fat layer were closed in the standard manner and the skin was closed with a subcutaneous running suture by my partner surgeon. The patient received all four units of blood in the operating room.
The patient was transferred to a private room, nurses were instructed to not leave the patient alone under any circumstances and to take her blood pressure every 15 minutes for the first 12 hours. Any bleeding, drop in pressure or other problems were to be reported to both of us immediately.
On post-op day 3, the patient was taken back to the operating room for removal of the gauze packing. If she had started hemorrhaging, she was informed that she would have to have an urgent hysterectomy, as we knew of no other way to stop the bleeding and save her life. We gently and slowly pulled on the end of the gauze roll (a total of 20 meters) which came out easily, I gently placed a hysteroscope (uteroscope) into her uterus. Everything looked fine, no obvious bleeding was seen and the patient was sent back to her room. Patient was observed for 5 more days to make sure ambulation did not re-start the bleeding. After this, mother and child were discharged home with instructions of no heavy lifting for two weeks.
Always take the mother’s wishes into account, unless they can kill her or the baby. Most of my colleagues, including the professor who was my chief, said they wouldn’t have done all that work and simply done a hysterectomy, due to her advanced age. I told them it was the easy solution but it is not for us to decide who can have a baby at what age and that our duty as a doctor was to save lives and try to help the patient in any way we can. Personally we do not like to take the easy way out in any surgery! This case was worrisome and difficult, as there wasn’t much of a chance to stop bleeding from an unknown foci in such a large organ, but think outside of the box and try innovative solutions–they do work sometimes. In addition, this was a great teaching case for my Assistant Surgeon, who is an excellent third year medical student (M.D.) and she is extremely intelligent and she looks for innovative solutions that can save a patient’s life. Third year medical students are not usually allowed to be the 1st Assistant on any surgery, especially a potentially life threatening problem, however my student is so good she received permission to assistant anywhere I felt confident for her to assist. This happened during her summer break so she was technically between her 2nd and 3rd year of medical school but officially she was classified as a 3rdyear. Obviously she was right in this case and I am proud of her that she is my medical student. Congratulations Dr. Stephanie Obrowski – Class of 2019.
None.
The author declares no conflict of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.