MOJ
eISSN: 2641-9300


Case Report Volume 1 Issue 1
1Department of Surgical Science, General Surgery and Pancreatic Diseases Unit-Policlinico Umberto I, Sapienza University of Rome, Italy
2Department of Radiology, Interventional Radiology Unit-Policlinico Umberto I, Sapienza University of Rome, Italy
Correspondence: Piero Chirletti, General Surgery and Pancreatic Diseases Unit-Policlinico Umberto I, Sapienza University of Rome, Italy
Co-correspondence: Luca Sacco, Department of Surgical Science, General Surgery and Pancreatic Diseases Unit-Policlinico Umberto I, Sapienza University of Rome, Italy
Received: September 04, 2017 | Published: September 12, 2017
Citation: Chirletti P, Sacco L, Corona M, et al. Severe intestinal bleeding due to left-sided portal hypertension after pancreatoduodenectomy with portal resection and splenic vein ligation. MOJ Tumor Res. 2017;1(1):1-3. DOI: 10.15406/mojtr.2017.01.00001
Pancreatoduodenectomy (PD) with portal vein (PV)/superior mesenteric vein (SMV) resection is well accepted for pancreatic head cancer because of the improvement in margin-negative resection and survival rates, without increasing postoperative morbidity and mortality in high volume centers. There is controversy in the surgical literature regarding the safety of splenic vein (SV) ligation during a PD with PV-SMV resection. Simple SV ligation has been associated with the development of left-sided portal hypertension, gastrointestinal bleeding and hypersplenism over the long term. We report a rare case of severe intestinal bleeding due to left-sided portal hypertension in patient who underwent a PD with PV-SMV confluence segmental resection and splenic ligation, preserving left gastric vein and inferior mesenteric vein, for cephalic pancreatic adenocarcinomas, seven months previously.
PV, Portal Vein; SMV, Superior Mesenteric Vein; PD, Pancreatoduodenectomy; SV, Splenic Vein; IMV, Inferior Mesenteric Vein
In patients with pancreatic head cancer, tumor invasion of the portal vein (PV) or superior mesenteric vein (SMV) is common because of the close anatomical relationship of the pancreatic head and uncinate process to the venous portal system. Pancreatoduodenectomy (PD) with portal vein or superior mesenteric vein resection is well accepted for pancreatic head cancer because of the improvement in margin-negative resection and survival rates, without increasing postoperative morbidity and mortality in high volume centers.1−4 When tumor infiltration involves PV-SMV confluence the splenic vein (SV) is ligated to achieve a margin negative resection. However, SV ligation may result in sinistral (left-sided) portal hypertension and gastrointestinal bleeding. Usually, compression of the splenic vein causes backpressure in the left portal venous system and subsequent gastric varices but, in the postoperative state, the pathophysiologic condition is altered and makes it difficult to diagnose.5−10 We report a case of severe intestinal bleeding due to left-sided portal hypertension in patient who underwent a PD with PV-SMV confluence segmental resection and splenic ligation, for pancreatic adenocarcinoma, seven months previously that have required a massive haemostatic resuscitation and surgical procedure (Figure 1).
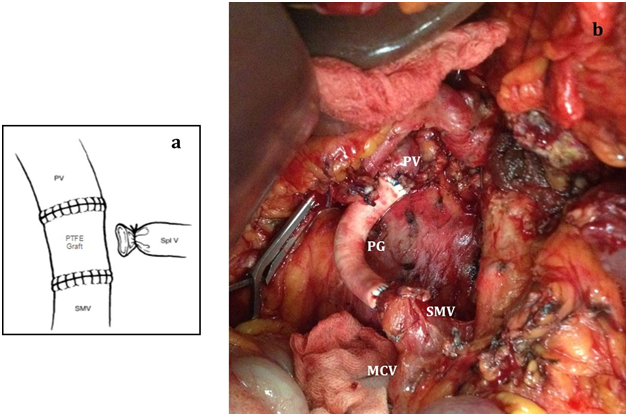
A 58-year-old man with pancreatic head cancer and no comorbidity has been undergone, at our institution, a PD with Total Mesopancreas Excision, PV-SMV confluence segmental resection with prosthetic graft interposition, splenic ligation with no reimplantation. We did not observe postoperative complications. Contrast-enhanced Multidetector Computed Tomography performed in VII postoperative day, showed graft patency with no signs of thrombosis (Figure 2). The preoperative diagnosis of pancreatic adenocarcinoma and the neoplastic invasion of PV wall up to the tunica media were both confirmed in the pathologic specimen. The patient started adjuvant chemotherapy with gemcitabine according to international guidelines on management of pancreatic cancer. After seven months of surgery the patient was readmitted to our hospital for a severe intestinal bleeding, subsequent to continuous melena, with severe anemia (Hb 6.6 g/dL; normal range 11.2-14.5 g/dL). The serum levels of liver enzymes and the other laboratory data were in the normal ranges. The causes of bleeding were not identified by several endoscopy including upper, lower gastrointestinal tract and small bowel. An abdominal-CT scan showed signs of portal hypertension, with slight dilation of the SMV and the presence of venous peripheral and perigastric collateral circles. Varicose veins in the gastro-digestive anastomosis were also noted, with signs of hyperemia of anastomized joints. No active arterial bleeding was identified. During the examination period, the anemia rapidly progressed and the patients needed numerous blood transfusions (total 56 units during 29 days), fresh froze plasma and platelets units. Then, he developed massive melena, with subsequent hypotension. An urgent angiography was performed to identify the cause and to treat the bleeding. A pseudoaneurysm of ileum-colic branches was showed by selective arteriography of superior mesenteric artery and it was treated by embolization with three metal spirals.
It looked like the bleeding had stopped but, twenty-four hours later; the patient presented a new episode of massive melena. Trans hepatic portography showed portal graft patency with normal mesenteric-portal axis pressure (PV pressure 5-6cm H2O, SMV pressure 11-12cm H2O) (Figure 3). The posterior and short gastric veins were also slightly dilated. This atypical drainage developed collateral vessels mainly adjacent to the pancreas and proximal jejunum and we considered it as so-called sinistral portal hypertension. Splenic artery embolization followed by splenectomy was performed stopped the bleeding and abdominal CT scan one month later showed reduction in the size of the collateral vessels.
This patient is still alive after forty-one months after PD, in good general conditions, but developed lung metastases treated by chemotherapy.
Greenwald and Wasch11 first reported, in 1939, sinistral (left-sided) portal hypertension. It is a localized form of portal hypertension that occurs as a result of isolated thrombosis or obstruction of the splenic vein.12-14 The features distinguishing it from other forms of portal hypertension are preserved liver function and a patent extrahepatic portal vein. There is controversy in the surgical literature regarding the safety of SV ligation during a PD with PV-SMV resection.9-5 Some authors state that it is safe but others claim that sequelae of left-side portal hypertension may follow. Consequently, some authors have advocated reimplantation of the SV into the SMV or into the left renal vein in order to decompress the left portal system.15-18 On the other hand, some surgeons report that reconstruction of the SV is not necessarily required, especially when the left gastric vein and inferior mesenteric vein (IMV) are preserved.19-21 When the IMV was not divided, the blood flow from the spleen may pass through the IMV or arc of Barkow to the colonic marginal vein and finally into the PV. If the left gastric vein is not divided, the blood flow from the spleen passes through the short gastric vein and it drains into the PV via the left gastric vein9 also described the important anatomy of venous flow patterns from the spleen via the colic marginal vein after PD with SV ligation. In the present case when PD with PV-SMV resection, SV ligation was performed, left gastric vein and inferior mesenteric vein was preserved therefore SV was not reimplanted. Despite that the patient developed left-side portal hypertension and severe bleeding. In these cases it would be useful to associate splenectomy. In conclusion, we presented a case of severe intestinal bleeding caused by atypical sinistral portal hypertension and we hypothesize that other mechanisms not yet well understood could exist that in some patients may cause left-sided portal hypertension. In order to avoid these complications, if not contraindicated, it is mandatory to associate splenectomy
All authors of this work have met all of the following criteria:
a. Substantial contributions to the conception or design of the work, or the acquisition, analysis, or interpretation of data for the work.Authors declare there is no conflict of interest in publishing the article.
Informed consent was obtained from patient.

©2017 Chirletti, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.