MOJ
eISSN: 2641-9300


Liposarcomas of the kidney and retroperitoneum are rare malignancies that have been reported in individuals aged between 36 and 86 years. They may be diagnosed incidentally or may present as: mass/lump in the loin or abdomen; loin pain; dyspnoea; shoulder tip pain; sudden abdominal pain with collapse; and other non-specific symptoms. Various radiology imaging scans are undertaken to identify the lesion. Diagnosis relies upon microscopy and immunohistochemistry features of the tumours which do illustrate features of: Well-differentiated and de-differentiated liposarcomas (WDLPS/DDLPS); Myxoid and round cell liposarcoma (MLS and RCL); Pleiomorphic liposarcoma. Microscopy examination does show lipoblasts which are relatively specific. Immunohistochemistry studies do show positive staining for S100 and calretinin. Treatment has been mainly by wide surgical excision: in the form of radical nephrectomy alone mostly for liposarcoma of the kidney most often, but rarely adjuvant therapy including chemotherapy plus or minus radiotherapy; for retroperitoneal liposarcoma, wide excision of the tumour plus or minus resection/excision of structures encased by the tumour including the kidney, pancreas, inferior vena cava, aorta, or iliac artery with reconstruction of the excised vascular structure (vessel) and in majority of cases adjuvant therapy had not been given due to controversies that exist globally about the usefulness of adjuvant therapy. Nevertheless, anecdotal reports had illustrated the usefulness of adjuvant therapy in achieving long-term disease-free survival. Generally the long-term prognosis is poor and for this reason there is need for a global multi-centre trial to compare wide surgical excision alone with wide surgical excision plus adjuvant therapy including combination chemotherapy plus or minus radiotherapy.
Keywords: Liposarcoma, kidney, retroperitoneum, S-100, calretinin, immunohistochemistry, radical nephrectomy, wide excision, chemotherapy, radiotherapy, CT scan, MRI scan, ultrasound scan
Liposarcomas are malignant tumours of mesenchymal origin which are derived from adipose tissue and they do constitute less than one percent of all malignant tumours. Primary liposarcomas of the kidney are extremely rare to the extent that some clinicians may not encounter a case of liposarcoma of the kidney during their working times. Liposarcoma of the retroperitoneum is also a very rare disease which sometimes could encase intrabdominal and retroperitoneal structures including the kidney, ureter, renal pelvis, pancreas, the abdominal aorta, inferior vena cava, and the iliac vessels. Retroperitoneal liposarcoma could also push the diaphragm upwards leading to dyspnoea as well as it could also push the gut to the contralateral side. The ensuing article on liposarcoma of the kidney and retroperitoneum encasing the kidney, renal pelvis and ureter, is divided into two parts: (A) Overview and (B) Miscellaneous narrations and discussions from case reports, case series, and studies related to liposarcoma of the Kidney and Retroperitoneum encasing the ureter, renal pelvis and kidney.
Aim
To review the literature on liposarcoma of the kidney and retroperitoneal liposarcoma involving or encasing the kidney and or ureter and renal pelvis.
Method
Internet data bases were searched including Google, Google Scholar and PUB MED. The search words used included: Liposarcoma of kidney, Renal liposarcoma, Retroperitoneal liposarcoma, and liposarcoma of the retroperitoneum. Twenty six references were identified that were used to write the review article. Information from various references were divided into general overview description of various aspects of the disease including the definition, epidemiology, presentation, clinical examination findings, investigation, diagnosis, treatment, differential diagnosis and outcome of the disease, Furthermore, suitable references were identified that provided miscellaneous narrations related to the diagnosis and management of various cases of the disease managed by different clinicians as well as the lessons learnt in the management of the disease.
(A) Overview
Definition/general comments
It has been stated that Liposarcoma is the commonest soft tissue sarcoma that is encountered in adults.1
Epidemiology1
Sites1
It has been stated that liposarcomas had been found manly in the following areas of the body1
Presentation
Liposarcomas of the kidney and or retroperitoneum may present as follows:
Clinical examination findings
Some of the possible clinical examination findings in cases of liposarcoma of the kidney or retroperitoneal liposarcoma encasing the kidney include:
Laboratory tests
Haematology investigations
Biochemistry investigations
Serum urea and electrolytes, serum glucose and liver function tests are part of routine tests that are undertaken in the general assessment of patients who have liposarcoma of the kidney and or retroperitoneum and most of the time the results would be normal. Very rarely if a retroperitoneal liposarcoma has encased the kidney or the ureter causing ureteric obstruction there may be some element of impaired renal function. In the event that the pancreas is invaded completely by liposarcoma then perhaps the serum glucose level theoretically could be raised. The liver function tests would generally be normal but in the rare case of disseminated liver metastasis the liver function test results may be normal. If pancreatitis is suspected as a differential diagnosis most often the serum amylase level would be normal.
Urine investigations
Urinalysis and urine microscopy and culture are routine tests that are done in the geneal assessment of patients who have loin pain and pyrexia of unknown origin. In cases of liposarcoma of the kidney or retroperitoneum the results would generally be normal but at times there may be evidence of non-visible or visible haematuria but this would not be diagnostic of liposarcoma.
Radiology investigations
Ultrasound scan
Ultrasound scan of abdomen and renal tract is a common investigation that is undertaken in the investigation of liposarcoma of the kidney and or retroperitoneum which would show the lesion in the kidney or retroperitoneum, its exact location in the kidney or retroperitoneum, its size can be measured and if there is any associated cystic elements or haemorrhage this could be commented upon but the findings would not be made based upon ultrasound scan. The ultrasound scan cold at times shows a hypo-echogenic or a hyper-echogenic heterogeneous lesion. However ultrasound guided biopsy of the lesion can be done for histology assessment and when the diagnosis is made appropriate treatment can be planned. Generally in the sporadically reported cases in the literature ultrasound guided biopsies had not been dine. Doppler ultrasound scan can be done to assess the vasculature of the tumour. Ultrasound scan of the entire abdomen and pelvis can be done to check if there is any lesion anywhere else in the abdomen and pelvis. Ultrasound scan can also be used as part of follow-up assessment to find out if there is any local recurrence or distant metastases.
Computed tomography (CT) scan
Contrast CT scan of renal tract or abdomen and pelvis is a useful may of investigating renal and retroperitoneal liposarcomas and this may show a contrast-enhancing heterogeneous mass within the kidney or retroperitoneum. The size, position, and the extent of the lesion as well as its relationship to other organs would also be shown. CT-scan biopsy of the lesion could theoretically be done for histology examination to confirm diagnosis of the lesion; however, this is not a common day to day practice. Furthermore if a retroperitoneal liposarcoma lesion is encasing organs including the ureter and kidney, the pancreas, the inferior vena cava, aorta, or iliac vessels, or the lesion is pushing the diaphragm upwards and compromising breathing the CT scan would show it. In the case of a liposarcoma of the retroperitoneum pushing the bowel anteriorly and to the contralateral side the CT scan will show it. CT scan of thorax is done for full staging of the liposarcoma of the kidney and or retroperitoneum after histology diagnosis has been confirmed. CT scan of thorax, abdomen, and pelvis forms part of the follow-up assessment for patients after they had undergone surgical plus or minus adjuvant therapy for the liposarcoma.
Magnetic resonance imaging (MRI) scan
MRI scan of renal tract or abdomen and pelvis is a useful may of investigating renal and retroperitoneal liposarcomas and this may show a contrast-enhancing heterogeneous mass within the kidney or retroperitoneum. The size, position, and the extent of the lesion as well as its relationship to other organs would also be shown. CT-scan biopsy of the lesion could theoretically be done for histology examination to confirm diagnosis of the lesion; however, this is not a common day to day practice. Furthermore if a retroperitoneal liposarcoma lesion is encasing organs including the ureter and kidney, the pancreas, the inferior vena cava, aorta, or iliac vessels, or the lesion is pushing the diaphragm upwards and compromising breathing the MRI scan would show it. In the case of a liposarcoma of the retroperitoneum pushing the bowel anteriorly and to the contralateral side the MRI scan will show it. MRI scan of thorax is done for full staging of the liposarcoma of the kidney and or retroperitoneum after histology diagnosis has been confirmed. MRI scan of thorax, abdomen, and pelvis can also be used as part of the follow-up assessment for patients after they had undergone surgical plus or minus adjuvant therapy for the liposarcoma.
Bone scan
Isotope bone scan can be done at times when there is suspicion of bone metastasis to confirm whether or not there is bone metastasis.
Positron emission/computed tomography (PET/CT) scan
PET / CT scan done in the investigation of something else may be the first investigation to alert the radiologist or the clinician to the fact that there is a lesion in the kidney or retroperitoneum. PET/CT scan could also be utilized in the follow-up assessments of patients.
Chest X-ray
Chest X-ray could be undertaken in the initial assessment of a patient who presents to the accident and emergency department with dyspnoea related to the pushing upwards of the diaphragm by a large retroperitoneal liposarcoma prior to the establishment of the diagnosis of liposarcoma of the retroperitoneum or kidney. Chest X-ray could be done at regular intervals in the follow-up of patients who undergone treatment for liposarcoma to establish whether or not they have developed pulmonary metastases; however, this has been superseded by CT scan or MRI scan of thorax which form part of the CT or MRI scan of thorax, abdomen and pelvis. In the developing countries where CT and MRI scans are not readily available in all hospitals, Chest X-ray and ultrasound scan of abdomen and pelvis would form the regular follow-up assessment options.
Retrograde ureteropyelogram plus or minus insertion of a ureteric stent
When a retroperitoneal liposarcoma has encased the kidney, renal pelvis, and ureter and has caused hydronephrosis cystoscopy plus retrograde ureteropyelogram and insertion of a ureteric stent could be undertaken to maintain or improve upon renal function and also if a kidney preserving operation is planned in the excision of the liposarcoma, insertion of a ureteric stent would make it easier for the surgeon who is undertaking open surgical excision of the liposarcoma to identify the ureter by palpation in order not to damage the ureter during the operation and the stent would then be removed after the operation/
Treatment
Macroscopic features
Microscopy features
It has been stated that: (a) lipoblasts do have round, sharply demarcated cytoplasmic lipid-clear vacuoles that scallop the nucleus and that they are smaller in comparison with vacuoles of mature adipocytes, (b) spikes of chromatin could project between the vacuoles, (c) lipoblasts may mimic signet-ring cells or they could have central nuclei that have small indentations by multiple fat vacuoles.1
Immunohistochemistry features
Positive staining
It has been stated that liposarcomas do exhibit positive immunohistochemistry staining for the following makers as follows:
Negative staining
Liposarcoma of the kidney has been shown to exhibit negative staining for5
Electron microscopy features
Electron microscopy examination features of liposarcomas have been summated as follows1
Differential diagnoses
Some of the documented differential diagnoses of liposarcoma include1
Outcome
It has been stated that the 10-year local recurrence-free and metastasis-free survival associated with low-grade group of liposarcomas is 87% and 95% and that with regard to high-grade group of liposarcomas, the 10-year local recurrence-free and metastasis-free survival is 75% and 61%.1,7
Matsuoka et al.8 reported a 66-year-old housewife who had presented with fever and left flank pain. She underwent various investigations including renal angiography and reno-scanning. The renal angiography had revealed pooling and avascularity and a cold spot was observed within the lower pole of her left kidney and based upon the findings a diagnosis of left renal tumour was made. She underwent left nephrectomy. Gross examination revealed that the nephrectomy specimen had weighed 270 grams and had measured 15 cm x 7 cm x 5 cm. Microscopy examination of the tumour revealed features that had been adjudged to be consistent with the diagnosis of differentiated liposarcoma. Electron microscopy studies of the tumour showed: fat droplet and inclusion body of microtubule which had been stated to be characteristic of liposarcoma that had occurred in other organs. Matsuoka et al.8 stated the following:
It would be argued that the case was well reported to remind clinicians about this rare condition and to illustrate the immediate success of nephrectomy in the treatment of liposarcoma. Nevertheless, the case was reported without any long-term follow-up data, therefore the long-term outcome would not be known. Some people would argue that in order to aim at achieving a good long-term disease-free survival adjuvant therapy including combination chemotherapy and radiotherapy should be given.
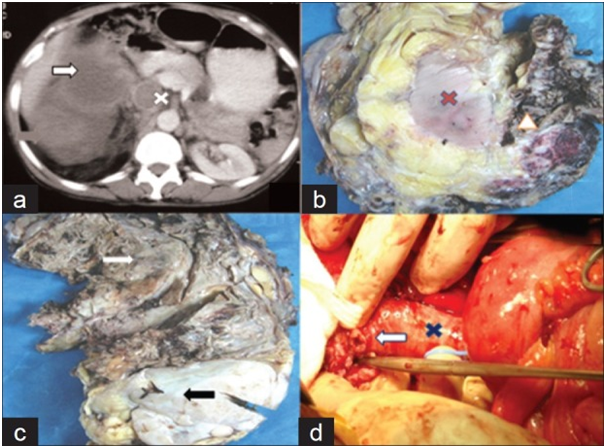
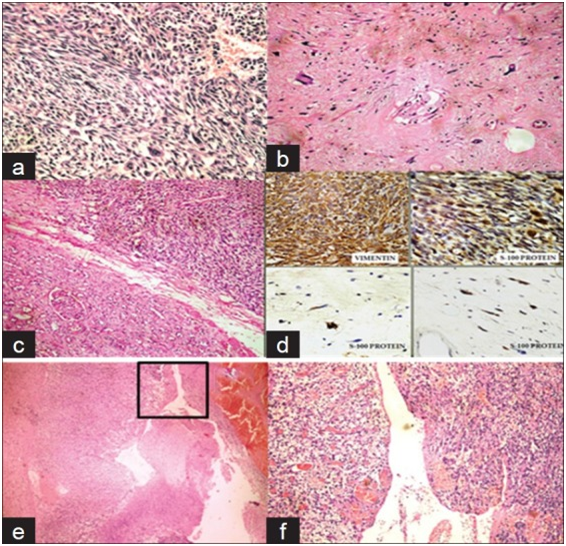
Shastri et al.5 reported a 65-year-old man who had presented with a lump in his abdomen and right flank pain of 4 months duration. He was asymptomatic otherwise. He did have a large, nodular mass was found in his right hypochondrium, epigastrium, and lumbar region. He radiology imaging studies including ultrasound with Doppler scan, computed tomography (CT) scan, and magnetic resonance imaging (MRI) scan which showed a mass within the upper pole and mid pole of the right kidney that measured 20 cm x 16 cm x 10 cm which had extended from the subdiaphragmatic region to the bifurcation of the aorta. Additionally the radiology images had also shown retroperitoneal lymph node enlargement and thrombus within the intravenous vena cava (IVC) with some doubtful fat density (Figure 1A). Thrombus was seen within the inferior vena cava which had extended from the intra-hepatic part of the IVC to the right common iliac vein. Based upon the radiology image findings a provisional clinical diagnosis of right renal cell carcinoma was made. During operation the tumour was found to have extended from just inferior to the liver down to the bifurcation of the aorta. The tumour was adherent to the wall of the IVC at the confluence of the right renal vein and the IVC and in view of this about 2 cm patch of IVC was resected and the IVC repaired (Figure 1D). The man therefore underwent right radical nephrectomy and removal of all the thrombus within the IVC. Gross examination of the specimen showed on cut surface, a large heterogeneous growth which had consisted of a distinct large necrotic tan brown area together with smaller fleshy yellowish part which together had measured 20cm x 14cm x 9m see Figure 1C and this was found to have infiltrated the renal sinus and had encased the rest of the kidney completely (Figure 1B). The macroscopically normal looking kidney did measure 11cm x 6cm and it could be easily shelled out from the tumour mass with the exception of the renal sinus, which in the opinion of the surgeon had suggested a possible origin of the tumour from the renal sinus. Microscopy examination of sections of the necrotic tan brown area showed a malignant mesenchymal tumour which was predominantly malignant fibrous histiocytoma (MFH)- like high grade sarcoma with brisk mitosis of between 20 to 25 mitoses per 10 high power field (Figure 2A). Microscopy examination of the tumour within the white fleshy area did reveal a well-differentiated liposarcoma that showed lipoblasts that had been lying within myxoid and focally sclerosed background, which had been well demarcated from the de-differentiated part (Figure 2B). The tumour was noted not to have infiltrated the kidney in any part of the planes with the exception of the renal sinus (Figure 2C). Microscopy examination of sections of tumour thrombus from the IVC did reveal de-differentiated areas of tumour only (Figures 2E & 2F). There was no evidence of tumour at the surgical resection margins including the ureter and renal artery. Based upon the overall microscopy features of the tumour a diagnosis of de-differentiated liposarcoma was made. Immunohistochemistry studies of the tumour showed that they tumour cells had exhibited strongly positive staining for vimentin and S-100 but negative staining for pancytokeratin, epithelial membrane antigen (EMA), desmin, and KMB-45 (Figure 2D). He received 6 cycles of combination chemotherapy which included doxorubicin and ifosfamide and he had n uneventful follow-up for 9 months at the time of the publication of the case report. Shastri et al.5 iterated that their case was the first case of liposarcoma of the kidney with tumour thrombus within the IVC that had been successfully treated by means of nephrectomy and post-operative chemotherapy with an ensuing uneventful follow-up.
Oh et al.9 reported a 71-year-old lady who had presented with progressive distension of her abdomen. She had ultrasound scan which revealed a huge retroperitoneal or mesenchymal mass which had occupied her entire abdomen. She was asymptomatic otherwise. She had a history of hypertension. She had a contrast-enhanced computed tomography (CECT) of her abdomen which showed a huge fatty mass which had originated from the retroperitoneum that had been interpreted to be probably indicative of retroperitoneal liposarcoma. The CT scan additionally showed encasement of the entire left kidney by the tumour. Septations and solid portions were also seen within the mass. The mass had pushed the spleen anteriorly and had deviated the small bowel to the right side of the abdomen. In view of the age of the patient it was decided she should undergo an organ preserving surgery at laparotomy. Successfully, the left kidney was preserved by utilization of a wide excision and separation of the tumour from the aorta by shaving it away thus preserving both the kidney and the aorta. Upon gross examination, the specimen had measured 45.0cm x 30.0cm x 11.0cm and had weighed 25.0kilograms. Microscopy examination of the tumour did reveal a combined type of liposarcoma with tumour components that included (a) well-differentiated liposarcoma that constituted greater than 95% of the tumour, and (b) myxoid liposarcoma that constituted less than 5% of the tumour. An average of 1 mitotic figure to 2 mitotic figures had been noted per high power field. Based upon the grading system of the French Federation of Cancer Centers, the tumour had been classified as grade 1. She recovered well from her operation. At her 16-month follow-up she had a CT scan which showed a newly defined low-density soft tissue mass in the aortocaval and pre aortocaval region that measured 3.5cm 1.8cmx4.3cm that was suggestive of locally recurrent tumour within the retroperitoneum. She did undergo surgical excision of the newly discovered mass. Microscopy examination of the completely excised newly discovered mass showed features that had been adjudged to be diagnostic of well-differentiated liposarcoma of the sclerosing type. Fluorescent in situ hybridization test revealed MDM2 amplification, which was interpreted as being consistent with the diagnosis of liposarcoma. Pursuant to the second surgery, the patient had undergone regular follow-up CT scan assessments for about 12 months without any clinical or CT scan evidence of recurrent disease. Oh et al.9 stated the following:
It would be argued that there is too much fear about utilization of chemotherapy and radiotherapy in liposarcomas of the retroperitoneum and the kidney and for this reason to clarify the situation there is need for a multi-centre trial of adjuvant therapy including chemotherapy and radiotherapy in good tertiary centres with close monitoring of patients in order to define the role of chemotherapy and radiotherapy in the treatment of liposarcomas of the kidney and retroperitoneum. It is true that there is no consensus opinion about the best option of management of liposarcoma. Some people would advocate complete surgical excision alone but others would recommend complete surgical excision plus adjuvant therapy including combination chemotherapy and radiotherapy. It could be argued that the fact that the tumour had recurred within 16 months of complete excision of the tumour should make clinicians have a rethink about utilization in that perhaps if the patient had undergone adjuvant therapy perhaps she may not have developed a recurrent disease. This argument though conjectural because there is still the possibility that the patient could still develop recurrent disease but still experience gained from the management of liposarcoma by surgical excision alone needs to be discussed by academic oncologists who should also review the experience gained by treating liposarcomas by complete excision plus adjuvant therapy to see if a consensus opinion would be formed to recommend surgical excision plus adjuvant therapy or not.
Bader et al.10 reported a 49-year-old Caucasian lady with a family history of polycystic kidney disease, who had been elected for organ donation. During her pre-operative assessment, she had ultrasound scan of abdomen and renal tract which revealed a rounded, heterogeneous, well-defined mass that had a solid aspect, adjacent to the lower pole of the left kidney. She also had CT scan which showed an expansive, solid, heterogeneous, lesion that had an attenuation of 38 Hounsfield Units (HU), was poorly defined within the external edge of lower third of the kidney that measured 3.8cmx3.8cm and CT scan evidence of preservation of perirenal fat. There was no CT scan evidence of contrast medium impregnation within the tumour during the late phase of the scanning procedure. The angiography did show a hypo-vascularized and hypo-dense mass. She had intravenous urography which was normal. She underwent left radical nephrectomy following intra-operative frozen section histopathology diagnosis of a malignant lesion. Macroscopic examination of the left radical nephrectomy specimen showed a brownish nodular structure with a diameter of 4.8 cm. Microscopy examination of the specimen showed a neoplastic tissue of mesenchymal origin, spindle and oval cells that had abundant cytoplasm, hyperchromic nuclei and intense pleomorphism that had been adjudged to be characteristic of pleomorphic liposarcoma of the kidney. The patient at the time of publication of her case report had undergone follow-up for four years and had remained asymptomatic without any control ecographic examination evidence of recurrent disease. Whilst it was good to realize that the patient had been free of recurrence for four years there is no way anyone could know or anticipate the long-term 10-year and 20-year outcome. Controversies exist regarding the management options of liposarcomas in that some people would still argue that perhaps from hind sight the patient should have been offered adjuvant therapy to as attempt to achieve long-term disease free survival. Other people would argue that these days less extensive organ preserving surgery should be undertaken in cases of kidney tumours that less than 5 cm and with no evidence of no lymph node involvement. Other people could argue that fine needle aspiration biopsy of the tumour should be undertaken for a small tumour on the periphery of the kidney and when a histology diagnosis of well differentiated tumour is made then various options of management should be discussed including:
In view of the aforementioned possible alternative treatment options and in view of the rarity of liposarcoma of the kidney there would be the need for a consensus opinion meeting of academic oncologists and urologists to discuss the merits and demerits of the treatment options in order suggest more feasible treatment options that are aimed at preservation of the kidney as well as ensuring long-term disease free survival. There would be the need for the establishment of global multi-centre trials on the management of primary liposarcoma of the kidney. Kim et al.11 reported a 36-year-old man who had presented with right flank pain of two weeks duration. He had a contrast computed tomography (CECT) scan of abdomen and renal tract which showed a large lobulated mass with focal areas of enhancement within the lower pole of the right kidney. He underwent radical nephrectomy under a provisional clinical and radiology image finding diagnosis of primary renal cell carcinoma involving the lower pole of his right kidney. Gross examination of the radical nephrectomy specimen revealed an 11 cm-sized well demarcated solid mass within the lower pole of the right kidney. Microscopy examination of the tumour showed that the tumour had comprised of pleomorphic spindle and epithelioid cells with focal areas that showed distinct adipocytic differentiation and geographic necrosis. A few diagnostic lipoblasts were seen on microscopy examination. Extensive search was undertaken on the samples but no carcinoma component was seen. Immunohistochemistry studies of the tumour showed that all of the tumour cells had exhibited negative staining for cytokeratin, but they had exhibited positive staining for vimentin. The lipoblasts exhibited positive staining for S-100 protein as well as for vimentin. A final diagnosis of primary pleomorphic liposarcoma of the lower pole of the right kidney was made. At his six months follow-up he was asymptomatic and there was no evidence of local recurrent disease or distant metastasis. Kim et al.11 stated that when a kidney tumour is found to be exclusively sarcomatous, they would recommend a generous sampling of the tumour with proper immunohistochemistry staining studies to differentiate a primary sarcoma of the kidney from a sarcomatoid carcinoma of the kidney.
Yang et al.12 reported a 60-year-old woman who had presented with a history of right sided abdominal distension of 2-monhs duration as well as having identified a touchable mass over in her abdomen the previous 1 month. She not has any other significant medical history. On examination she was found to have a 10cmx15cm flexible non-tender mass that did not have any clear boundary on the right side of her abdomen. The results of her routine blood haematology and biochemistry tests, tumour markers as well as urine tests were normal. She had computed tomography (CT) scan and magnetic resonance imaging (MRI) scan which revealed a huge mass within the right side of her abdomen. A diagnosis of well-differentiated retroperitoneal liposarcoma was made and there was no evidence of metastasis; however, based upon the scans a possibility that the tumour had invaded the kidney was inferred. During her operation it was observed that the mass had originated from the right fatty renal capsule and the kidney was covered by the tumour. Complete resection of the tumour was undertaken with preservation of the right kidney. The renal fascia was left intact with no obvious sign of invasion macroscopically. The periphery of the kidney was completely bare, including the renal portal, the ureter, and the inferior vena cava. The total excised tumour mass measured 20 cm x 15 cm x 10 cm. Microscopy examination of the specimen showed features that had been adjudged to be consistent with the diagnosis of retroperitoneal well-differentiated liposarcoma full of lipocytes. The case was reported to document feasibility of preservation of the right kidney at a time when there was no long-term follow-up outcome available. Yang et al.12 sated the following:
It would be argued that even though a kidney preserving resection of the right sided retroperitoneal liposarcoma was achieved there was no long-term follow-up data on the outcome of the patient; however, it could extrapolated or speculated that there is a high chance that local recurrence would subsequently develop. Based upon the idea that if a tumour load is small chemotherapy and radiotherapy would perhaps work better with regard to achieving cure in comparison with when the tumour load is large and for this reason it could be argued from hind-site, it would have been better for the patient who had undergone kidney preserving resection of retroperitoneal liposarcoma to receive adjuvant chemotherapy and radiotherapy rather than wait till the patient develops recurrent disease.
McCartney & Wynne.13 in 1936 commented on a previous report of Hartwig in which a 36-years-old woman had been reported by Hartwig who had had an enlarged abdomen over a preceding period of eight years. She suddenly became seriously ill and had collapsed. She underwent exploratory laparotomy and removal of her right kidney which had contained tumour on the same day. She died shortly after completion of the operation. Gross examination of the specimen showed that tumour mass had weighed 3500 grams and was of variable consistency as well as lobulated. Foci of haemorrhage were observed in the tumour. Small nodules that mimicked the large tumour were seen in other parts of the kidney. Microscopy examination of the specimen revealed that the tumour had comprised of largely pure adult adipose tissue, but scattered through the tumour were cellular foci that had been made up of spindle and round cells and fat-containing cells. Hartwig adjudged the tumour to have been lipoma which had undergone sarcomatous change into liposarcoma. Based upon this report it would be inferred that liposarcoma of the kidney could undergo spontaneous haemorrhage.
El Howains et al.14 reported an 86 year old man who had been referred with an asymptomatic kidney mass that was incidentally found a computed tomography (CT) scan. He had undergone 2 years earlier local excision of a malignant melanoma on the planter surface of his right foot. During his routine follow-up he had a chest radiograph which showed a soft tissue shadow in the lower lobe of the right lung which was confirmed CT scan as a small nodule which was considered to be a metastatic deposit that had ether originated from the primary melanoma or from a potential renal cell carcinoma considering the cystic nature of the renal mass. He had also been undergoing follow-up for raised serum PSA of 9.2 micrograms per litre. He had hypertension and bilateral cataracts. His general and systematic examinations were normal. The results of his routine haematology and biochemistry blood tests as well as urine examinations were normal, He underwent laparoscopy which showed as s large right sided kidney mass within the lower pole. An open partial nephrectomy was undertaken (lower pole partial nephrectomy on the right side). The tumour measured 14.0cmx9.0cmx3.0cm. Microscopy examination of the tumour revealed that the tumour was a well-differentiated liposarcoma of the kidney that was present around the nodular areas of dedifferentiated liposarcoma with positive surgical margins which had indicated an incomplete surgical resection. Immunohistochemistry studies of the tumour showed that the tumour cells had exhibited a strong diffuse positive reaction with smooth muscle actin (SMA) and weak focal positive staining for CD99. Immunohistochemistry studies also showed that the tumour cells had exhibited negative staining for: AE/3, S100, HMB45, Melan A, Cytokertin7, Cytokeratin 20, desmin, and inhibin which had been important in excluding metastatic melanoma and metastatic carcinoma after having taken into consideration the past medical history of the patient. He did not receive any chemotherapy or radiotherapy. T his 6-month post-operative follow-up he was well and he had CT scan which did not reveal any local recurrence or metastasis. It would be argued that the patient had not had a long-term follow-up therefore one cannot tell what the long-term outcome of the patient would be but considering that there was tumour at the surgical margin the operation should be considered as not having achieved treatment of curative intent and for this reason adjuvant chemotherapy plus radiotherapy should have been given.
Tanaka et al.15 reported a 60-year-old woman who had a large retroperitoneal liposarcoma that was removed by means of resecting the descending abdominal aorta and infra-hepatic inferior-vena cava, right nephrectomy and pancreatoduodenectomy pursuant to the creation of extra anatomical femoro-femoral crossover bypass after left axillo-left femoral bypass. The patient did develop oedema of the leg for a few weeks following her operation but the swelling gradually resolved with (11Tanaka et al.15 stated that complete surgical resection with negative margins is the only potential curative treatment for such types of large retroperitoneal liposarcomas encompassing the kidney and other organs in the abdomen and retroperitoneum. Pathology examination of the specimen showed a dedifferentiated liposarcoma with negative margins. Despite the evidence of no recurrence at her 16-month follow-up it could be argued that the extensive surgery alone is not to provide treatment of curative intent for liposarcoma that had invaded retroperitoneal organs that had been excised and that adjuvant chemotherapy plus radiotherapy would have been an additional treatment that would help provide treatment of curative intent rather than wait and treat recurrent tumours in the future by means of chemotherapy and radiotherapy.
Taniquchi et al.16 reported a 65-year-old man who had computed tomography(CT) scan as part of investigation for melena that magnetic resonance imaging (MRI) scan which showed a tumour that did not have adipose components in the perirenal space. A provisional pre-operative diagnosis of retroperitoneal malignant tumour was made. He underwent excision of the tumour and left nephrectomy. Pathology examination of the surgically excised specimens showed features that had been adjudged to be consistent with the diagnosis of inflammatory liposarcoma. He did not have any additional treatment and at his 10-month follow-up there was no evidence of local recurrence. Whilst it would be said that the short term outcome of surgery alone has been good up to his 10-month follow-up one cannot tell what the long term follow-up outcome would be like. Despite the controversies relating to the appropriate management, some people would still advocate for utilization of adjuvant therapy. If there was a long-term follow-up outcome on this patient one could then infer whether or not surgery alone is an adequate treatment for renal and perirenal liposarcomas.
Crisan et al.17 reported two patients who had been diagnosed with retroperitoneal perirenal myxoid liposarcoma. The two patients had had radiology imaging which in both cases had shown a huge right retroperitoneal tumour mass that had compressed the abdominal organs and large blood vessels. The surgical management of both cases had entailed en bloc resection of the tumour and the right kidney (nephrectomy) through a trans-peritoneal approach. Three years following the surgery, both patients developed local recurrence, for which they received chemotherapy. Crisan et al.17 stated the following:
Based upon the lessons learnt in the management of the patients, some people could argue that the option of such tumours should be wide surgical resection plus adjuvant therapy and perhaps if both patients had received adjuvant chemotherapy plus radiotherapy they might not have developed local recurrent disease. The answer and best solution would not be known and for this reason the best way to find and answer would be to establish a multi-centre trial that would compare wide excision alone with wide excision plus adjuvant therapy.
Ioannidis et al.20 reported a 55-year-old woman who had dyspnoea and light diffuse abdominal pain which was caused by a giant retroperitoneal liposarcoma. She had a CT scan which showed a large mass a t the right side of the abdomen, with its upper limits to the lower edge and the gate portion of the liver. The mass was in contiguity with the right kidney, the inferior vena cava, and the right renal vein which had caused mild dilatation of the right renal pelvis. There was no evidence of metastasis in the abdomen. The tumour was surgically excised. Pathology examination showed that the tumour was a well-differentiated liposarcoma. She had remained well and at her 4-years follow-up there was no evidence of recurrence. Ioannidis et al.20 stated that retroperitoneal liposarcoma is a clinical entity which is associated with unclear clinical symptoms and physicians should consider including retroperitoneal liposarcoma in the differential diagnosis of a majority of symptoms including dyspnoea. It would be argued that lessons learnt from this case do indicate that wide surgical excision alone without adjuvant therapy in some cases of retroperitoneal liposarcoma is associated with good prognosis. This case also has shown that retroperitoneal liposarcomas can cause dilatation of renal pelvis from external compression without initially invading the kidney itself.
Yamaguchi et al.21 reported a 65-yerar-old man who presented with abdominal pain. He had computed tomography (CT) scan of abdomen which revealed a well-enhanced retroperitoneal tumour which was resected together with the right kidney as well as the right adrenal gland. The histopathology features of the tumour had been adjudged to be diagnostic of dedifferentiated liposarcoma adenocarcinoma. Eleven months pursuant to the operation, he was diagnosed as having developed local recurrence of his previous tumour and this recurrent tumour was resected. Following this, he was diagnosed with the development of repeated local recurrences for which he underwent repeated tumour resections. At 5.9 years following his initial operation, local recurrence of tumour and distant metastases in the axilla and soft tissue of the scapula were detected. He was started on Bevacizumab therapy, and the tumour reduced in size markedly. Bevacizumab treatment was continued for 6.7 years after the initial operation, with no local tumour recurrence or development of metastasis. This case report has highlighted the usefulness of Bevacizumab therapy in the treatment of liposarcoma adenocarcinoma. Based upon the clinical course of the disease in this case and the usefulness of Bevacizumab therapy it would wondered whether the patient would have developed any local recurrence or distant metastasis at all if he had received adjuvant chemotherapy around the time of his initial wide resection of tumour plus right radical nephrectomy with right adrenalectomy. This question would be a common debatable question always in the management of liposarcoma of the kidney and retroperitoneum.
Iwama et al.22 reported a 52-year-old man who presented with abdominal distension. He had enhanced computed tomography (CECTT) scan which showed a giant retroperitoneal tumour that had surrounded the left internal iliac artery and left kidney. He underwent en bloc tumour resection along with resection of his left internal iliac artery and left kidney. The tumour did weigh 6.860 grams and had measured 35 cm. The pathology features of the tumour had been consistent with the diagnosis of dedifferentiated liposarcoma. Following his operation, the patient did experience left lower limb paralysis. His clinical examination and neurological examination findings had suggested a lumbo-sacral problem. Six months following the operation, the patient’s lower limb paralysis had not improved. Iwama et al.22 pointed out that it is important for clinicians to note that ischaemic neuropathy could be an emanation related to internal iliac resection.
Fichera et al.23 described a series 3 cases of radiologically- and histologically-confirmed liposarcoma of the kidney out of 3,224 surgical operations undertaken for primary cancers of the kidney that had been undertaken over 28 years between 1987 and 2015 that amounted to 0.09% in a single tertiary care centre. With regard to the results, Fichera et al.23 stated that the patients had undergone open radical nephrectomy through an anterior trans-peritoneal access with complete resection of the retroperitoneal mass and retroperitoneal lymph node dissection. After a mean follow-up of 45 months all of the 3 patients had died from progression of tumour. Fichera et al.23 stated the following:
Based upon the fact that all three patients in this series had died within a mean period of follow-up would make some people wonder whether the patients would have lived longer if they had received adjuvant chemotherapy plus or minus radiotherapy. Lessons learnt from this study would make the author form the opinion that perhaps all patients who undergo nephrectomy or wide excision of large retroperitoneal liposarcomas should be considered for and given adjuvant therapy including chemotherapy and radiotherapy especially cases of dedifferentiated liposarcomas and perhaps the wait and see approach could be adopted for cases of well-differentiated tumours if the surgeon is not inclined to go through the route of adjuvant therapy.
Al Sheikh et al.24 reported a 61-year-old Caucasian lady who had presented as emergency after collapsing at home with pain in her abdomen radiating to the back. She had urgent CT angiogram to exclude a ruptured aortic aneurysm but the CT angiogram showed a large 21 cm fat-containing lesion which had arisen from the mid-portion of her left kidney and an adjacent 4 cm peri-renal haematoma. A provisional diagnosis of ruptured angiomyolipoma was made. Her haemoglobin was 105 grams per decilitre, and her serum creatinine was 104 millimoles per litre as well as her estimated glomerular filtration rate (EGFR) was 47 millilitres per minute. Her clotting was normal. Pursuant to her resuscitation, she underwent an emergency open left radical nephrectomy through a left flank incision following which she was discharged after six days. Histopathology examination of the specimen confirmed the diagnosis to be well-differentiated liposarcoma. The lesson learnt from this case report is to remember that liposarcoma of the kidney can also present as an emergency as a result of spontaneous rupture which would mimic ruptured intra-abdominal aortic aneurysm. Considering that the liposarcoma was well differentiated perhaps it would be unlikely to recur in comparison with undifferentiated liposarcomas but the patient would require careful follow-up and if she develops a recurrence this could be excised followed by chemotherapy.
Uchihashi et al.25 reported a case of dedifferentiated liposarcoma with huge cystic change without preoperative chemo- or radiation- therapy. The lesion had arisen in the retroperitoneum juxta-posed to the right kidney of a 67-year-old lady. She underwent a surgical excision of the retroperitoneal cyst. The cystic tumour had contained 1600 ml of old bloody fluid, and its wall had been comprised of oedematous, inflamed, or sclerosing fibrous tissue and fatty tissue that contained abundant atypical stromal cells, which upon immunohistochemistry studies had exhibited positive staining for MDM2 and CDK4, and had depicted MDM2 gene amplification by means of fluorescence in situ hybridization test. The wall was in contiguity with an atypical lipomatous nodule that was located within the mesentery. Pathology examination of the surgical specimens of the right hemicolectomy and right nephrectomy showed atypical cells that had infiltrated into the sub-serosa of the colon and the peri-renal fat tissue or that within the renal sinus. Uchihashi et al.25 stated their reported case had indicated that liposarcoma should be c well differentiated or de-differentiated liposarcoma should also be taken into consideration with regard to the differential diagnosis of a peri-renal cystic mass.
Ono et al.26 reported a long-surviving patient who had retroperitoneal liposarcoma which required 6 surgical resections in 16 years. They reported a 62-years-old man who had been diagnosed with liposarcoma that was first excised in 2001. Following that they had excised recurrences in the retroperitoneum with the left kidney in 2004. They also excised recurrences with the left half of the colon in November 2007 and in February 2010. Furthermore, Ono et al.26 excised recurrences with part of the intestine in November 2014 and at that time they had excised recurrences under the right abdominal rectus muscle and near the left half of the colon. Histopathology examinations of the specimens showed well-differentiated liposarcoma. Ono et al.26 stated the following: There had currently not been any evidence of recurrence 16 years after the first recurrence excision.. In their case, active excision of recurrences and identification of high-grade de-differentiated type of liposarcomas were factors of long survival. Based upon this case report, despite the 6-years survival, it could be asked why the patient did not receive chemotherapy or radiotherapy after the development of the first recurrence because it could be argued that if chemotherapy plus or minus radiotherapy had been given conjecturally the patient may not have developed so many recurrences.
Rhu et al.27 analysed the clinical impact of radical nephrectomy on retroperitoneal liposarcoma near the kidney. Rhu et al.27 obtained data of patients who had undergone surgery for unilateral primary retroperitoneal liposarcoma near the kidney in a retrospective undergone nephrectomy and combined resection of other organs. Kaplan-Meier survival analysis was utilized to estimate disease-free survival as well as overall survival. Multivariate Cox analysis was utilized to analyse the factors that are related to disease-free survival and overall survival. Rhu et al.27 summated the results as follows: Nephrectomy (HR=0.260, CI=0.078-0.873, p=0/029) did have a beneficial effect on disease-free survival while interaction model of nephrectomy*other organ resection (HR=4.655, CI=1.767–12.263, p=0.002) did show poor disease-free survival. Other organ resection was not found to be related to disease-free survival (HR=1.453, CI=0.146–16.251, p=0.718). Operation method (p=0.007) and FNCLCC grade (p<0.001, G2, HR=1.833, CI=0.684–4.915, p=0.228, G3, HR=9.190, CI=3.351–25.199, p<0.001) had been significant factors related to disease-free survival. Whilst combined organ resection without nephrectomy group (HR=1.604, CI=0.167–15.370, p=0.682) and radical nephrectomy with combined organ resection group (HR=1.309, CI=0.448–3.825, p=0.622) did not show any significant difference with regard to disease-free survival from the mass excision only group, radical nephrectomy without combined organ resection group (HR=0.279, CI=0.078–0.991, p=0.048) did show superior disease-free survival. Rhu et al.27 concluded that radical nephrectomy of unilateral primary retroperitoneal liposarcoma near the kidney does have a beneficial effect on disease-free survival. Whilst the observation from this study is well understood, it could still be argued that the role of adjuvant therapy needs to be studied as well.
Li et al.28 reported a 67-year-old man who had had hypertension for 20 years and who had had intermittent fever of no obvious source found over the preceding one month to his presentation. His routine blood haematology and biochemistry test results as well as his urine test results were normal. He had ultrasound scan of abdomen which showed a heterogeneously hypo-echoic mass of about 92mm in diameter over his left kidney. He subsequently had computed tomography (CT) scan of abdomen which showed a hypointense mass without a downward displacement of the left kidney and because the mass was considered to have an atypical enhancement of tumour in the arterial phase, the mass considered to be a renal parenchymal tumour. A magnetic resonance imaging (MRI) scan was undertaken which showed a huge tumour that measured 10.3cm x 9.3cm x 8cm and which had ambiguous border over the upper pole of the kidney. The tumour had extended into the perinephric tissue but not into the ipsilateral adrenal gland. Trans-arterial embolization (TAE) of the tumour was undertaken to reduce the blood loss before a left subcostal incision nephrectomy was undertaken. During the procedure, a solid left kidney tumour which had yellow fat component was found. Microscopy examination of the tumour showed hypercellular spindle tumour cells that had rhabdomyoblastic differentiation. Immunohistochemistry studies showed that the tumour had exhibited positive staining for murine double minute 2 (MDM2) and P16 for the tumour cells. There was evidence of tumour invasion into the renal capsule and perirenal fat. Based upon the microscopic features and the immunohistochemistry features of the tumour a final diagnosis of dedifferentiated liposarcoma of the left kidney, stage pT3 was made. At his 1-year follow-up, there was no evidence of metastasis. Whilst it was noted that there was no recurrence after 1 year of follow-up the long-term outcome would not be known. So far it would appear as if a radical nephrectomy has been adequate for the initial management of the disease, nevertheless, some people could argue that despite the controversies over the usefulness of adjuvant chemotherapy and radiotherapy, for a pT3 tumour that had invaded the renal capsule and the perirenal fat adjuvant chemotherapy plus radiotherapy could be considered as additional treatment options aimed at providing treatment of curative intent.
Liposarcoma of the kidney and retroperitoneum are rare tumours that have been reported sporadically which generally have been associated with poor long-term disease free survival. Majority of the tumours have been treated by surgical excision alone whilst very few cases have been treated by surgical excision plus adjuvant therapy in the form of chemotherapy alone or chemotherapy plus radiotherapy. There few anecdotal reported cases that had illustrated the usefulness of adjuvant chemotherapy and radiotherapy in achieving treatment of curative intent. There is need to resolve the controversies that exist regarding the usefulness and non-usefulness of adjuvant therapy in the treatment of liposarcomas of the kidney and retroperitoneum by undertaking a global multi-centre trial that would compare wide surgical excision alone with wide surgical excision plus adjuvant chemotherapy plus or minus radiotherapy. There is also the need to explore utilization of other treatment options including partial nephrectomy plus adjuvant therapy, cryotherapy plus adjuvant therapy, radiofrequency ablation plus adjuvant therapy, irreversible electroporation plus adjuvant therapy for small liposarcomas of the kidney that measure less than 5 cm by first undertaking radiology-image guided biopsies of small kidney tumours first to confirm histopathology diagnosis of liposarcoma of the kidney.
Acknowledgement to the Indian Journal of Urology for allowing figures and documentations form their Journal to be reproduced copy under right © Indian Journal of Urology. This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
None.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.