MOJ
eISSN: 2641-9300


In the context of bone injury, etiologies can be primary or secondary, manifesting imaging level mixed lytic lesions, or blastic. The spectrum of clinical manifestations ranging from asymptomatic (80%) to a pathological fracture, and in most cases an incidental diagnosis. The primary etiology of secondary lytic lesions are due to metastasis of solid tumors of prostate, lung and breast; moreover the main cause of primary bone lytic lesions occupies multiple myeloma. Cabinet Functional imaging diagnostic aids is from low sensitivity tests such as radiographic study to higher performance as bone scintigraphy. A review of 5 cases of lytic lesions occurs,
Keywords: bone metastasis, pathological fracture, lytic lesions, osteolytic myeloma
Bone lytic lesions include a wide range of etiologies, from a primary lesion of origin to those of secondary origin. Bone formed by two parts, a cortical (80%) and trabecular (20%), strikes a balance between osteoblastic and osteoclastic activity; The imbalance in this system leads to the appearance of three types of lesions: lytic, blastic or mixed.1 The clinical spectrum of patients with bone lesions, ranging from asymptomatic in 80% to have manifestations such as pain, immobility, hypercalcemia, symptoms of spinal cord compression and in more severe cases presenting pathological fractures.2,3 Osteolytic lesions are due mostly to metastatic spread, being the most common solid tumors (prostate, breast and lung) in approximately 70%.4 Prostate cancer remains the leading cause showed incidence of 21% and a mortality rate of 8%, exceeded lung cancer with a mortality of 27%.5 Within primary lytic lesions leading cause multiple myeloma is 75%, followed by osteosarcoma 20% and a lower percentage chondrosarcoma.6 In operation, the basic pillars pain management, chemotherapy, radiotherapy, hormonal therapy, bisphosphonates and even decompressive surgical management to improve neurological symptoms.7,8 The high burden of disease, causes imaging techniques take importance in early detection of these lesions, and to determine extent, stratification and coexisting complications; We present a series of five cases in which bone imaging findings and their relationship with the clinical condition of each patient in order to review relevant aspects of these lesions are described.
Case 1
65-year-old farmer with no history of importance, was admitted to the emergency department for clinical one year of consistent evolution in progressive deterioration of functional class 1 to 3, associated with loss of objective weight of 8 kg, dyspnoea, fatigue, weakness and hyporexia, with edema formation in the left lower limb pain associated with oppressive type with analogue scale pain 7/10, and limitation of motion. blood count, renal function, clotting times, reports within normal parameters (Table 1): In the approach of the patient with dyspnea in the ED, the following tests were requested. Additionally, venous doppler ultrasonography of the left lower limb is performed documented chronic DVT recanalization low superficial femoral vein and femoral popliteal junction; chest radiograph requested showed pulmonary nodule in the left upper lobe, correlated with positron simple and contrasted thorax, which also changes in bone density were observed in the lumbar spine, compatible lytic lesions (Figure 1 & Figure 2).
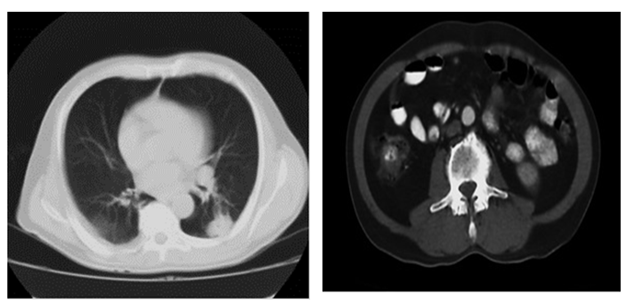
Figure 1 & 2 Single scan of the chest and contrasted.
Description: observed Figure 1 with nodule with soft tissue density of 33x26 mm, irregular edges, located in segment 6 of the left lung. In Figure 2 pattern of cortical destruction with erosion compatible with lytic lesion is observed.
Biopsy of the lung lesion that documented poorly differentiated adenocarcinoma of the lung was performed. Immunohistochemical studies biopsy bone injuries resulting in metastasis probable lung origin, bone scan requested sample bone involvement by secondary disease, multiple high uptake foci right shoulder, sternoclavicular joint, costal arch after 5 and 6 right completed and C7-T1 vertebrae T7 (Figure 1 & Figure 2). It is considered finally patient with lung adenocarcinoma with multiple bone metastases with a lytic deep pattern and a chronic syndrome (Trousseau) venous thrombosis.
Case 2
Man 81-year-old from rural areas admitted with clinical six-month history of dyspnea, fatigue, weakness, hyporexia loss objective weight of 10 kilograms, quantified fever peaks and obstructive urinary symptoms consistent with prostate disease ( micturition decreasing caliber, nocturia, urinary frequency and urgency). The patient physical examination with clinical signs of dehydration, mucocutaneous pallor, but no breath sounds in right lung base, hepatomegaly 5 cm painful, edema in lower grade I and marked members generalized muscular hypotrophy. Paraclinical with report bicytopenia (anemia and leukopenia in transfusion ranges), hyperbilirubinemia at the expense of direct bilirubin, metabolic acidosis and with findings of LDH, alkaline phosphatase and increased amylase (Table 1). Total abdominal ultrasonography showed signs of cholecystitis and cholelithiasis, bile duct with 8mm, splenomegaly and prostate hyperplasia was performed. A chest radiograph is made with evidence of generalized osteopenic changes (Figure 3) initial treatment for acute pancreatitis is indicated with Ranson 1 point and apache 14, Transfusion support and application studies for possible myelodysplastic syndrome or primary tumor to establish. Since the patient had obstructive urinary symptoms and prostate, ultrasound studies of urinary tract showed grade IV prostatic hyperplasia report transrectal prostate biopsy were expanded undifferentiated adenocarcinoma. It is done studies tumor extension with abdominal tomography (Figure 4 & Figure 5). Because clinic, patient age, and paraclinical report biopsy findings primary solid tumor, injury to process extension primary neoplastic lesion were attributed described.
Paraclinical Entry |
Case 1 |
Case 2 |
Case 3 |
Case 4 |
Case 5 |
|
haemogram |
hb |
15g/dl |
5g/dl |
12gr/dl |
9.1g/dl |
5g/dl |
HTO |
Four. Five% |
fifteen% |
36% |
28% |
17,8% |
|
VCM |
89ft |
87ft |
87ft |
90ft |
86ft |
|
HCM |
31pg/dl |
30pg/dl |
31pg/dl |
31 pg7DL |
29pg/dn |
|
leucocytes |
7,200 |
3000 |
8050 |
8900 |
22600 |
|
neutrophils% |
61% |
58% |
67% |
65% |
88.50% |
|
lymphocytes% |
40% |
40% |
51% |
39% |
7.10% |
|
platelets |
220 |
180 |
246000 |
190000 |
127000 |
|
creatinine |
0.8 mg/dl |
2.3 mg/dl |
0.6 mg/dl |
3 mg/dl |
0.98 mg/dl |
|
BUN |
8 mg/dl |
23 mg/dl |
10 mg/dl |
28 mg/dl |
32.48 |
|
TP |
13 sec |
12.6 sec |
12.7 sec |
11.8 sec |
13.4 sec |
|
TPT |
25 sec |
24 sec |
26.2 sec |
25 sec |
36.2 |
|
INR |
1.09 |
1.3 |
0.97 |
8-Jan |
1.22 |
|
Total bilirubin |
- |
6 |
- |
- |
- |
|
Direct bilirubin |
- |
4.5 |
- |
- |
- |
|
urinalysis |
- |
Normal |
- |
- |
- |
|
Sodium |
- |
136 mEq/L |
139 mEq/L |
139 mEq/L |
123mEq/L |
|
Potassium |
- |
4.1 mEq/l |
3.71 mEq/L |
2.2 mEq/L |
3.8mEq/L |
|
Calcium |
- |
8 mEq/L |
- |
13 mEq/L |
11mEq/L |
|
Glucose |
- |
91 mg/dl |
93 mg/dl |
90 mg/dl |
92mg/dl |
|
LDH |
- |
600 IU/L |
- |
580 IU/L |
713 IU/L |
|
FA |
- |
250 IU/L |
- |
300 IU/L |
326 IU/L |
|
Amylase |
- |
300 IU/L |
- |
- |
- |
|
PCR |
- |
- |
- |
3.5 mg/dl |
- |
|
TSH |
- |
- |
2.8 mU/L |
- |
- |
|
arterial blood gases |
- |
Ph: 7, HCO3: 11, PCO2: 30 |
- |
- |
pH 7.54. HCO3 24.8, pCO2: 29 |
|
Albumin |
|
- |
- |
3.62 gr/dl |
2 g/dl |
2 g/dl |
Table 1 Laboratory studies.
Hb, hemoglobin; MCV, mean corpuscular volumen; MCH, mean hemoglobin concentration; BUN, urea nitrogen; TP, prothrombin time; TPT, thromboplastin time; LDH, lactate dehydrogenase; FA, alkaline phosphatase; PCR, C-reactive protein; TSH, thyroid stimulating hormone; HCO3, bicarbinato; PCO2, partial pressure of carbon dioxide.
Case 3
52-year-old housewife with a history of hypertension staff, no known family history of clinical. Consulta five days of evolution, consisting of holocraneana headache and pulsatile characteristics associated with multiple episodes emesis without showing improvement with outpatient analgesic management. Mass under review referring systems left breast of 1 year of evolution approximately painless so there was not consulted. Physical examination of tachycardic income and tensional figures range finding hypertensive crisis with mass in the left breast, 3x3 cm retroareolar adhered to deep planes and nodular lesion in the right cervical region. income paraclinical studies with blood count, urinalysis, liver function tests, LDH, VSG, electrocardiogram performed,
Ultrasound examination of breast tissue reported in retro areolar region left breast image hypo echoic aspect 18x9x5mm, irregular borders, microcalcifications, and presence of partitions, compatible BIRADS 4B. In the context of its findings and high suspicion of neoplastic process at the level of breast tissue with persistent headache extension studies requested, it was made a CT scan simple skull with evidence of bone involvement of the cranial vault (Figure 6). Right cerebellum associated with cystic lesion, left cerebellum with four permeable ventricle, bone metastasis epidural towards the wing right sphenoid, front left and right parietal: simple and contrast skull resonance which shows space occupying lesions that capture contrast is performed. Breast biopsy showed infiltrating ductal carcinoma grade type II Nottingham ranking was performed. Therefore breast carcinoma advanced multiple bone involvement with unresectable lesions described considered.
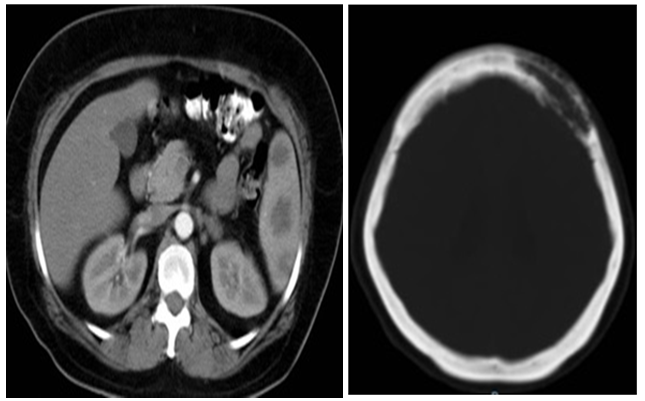
Figure 6 & 7 Tomography simple skull. Simple and contrasted tomography abdomen.
Description: Figure 6 shows osteolytic lesion ill-defined boundary level of 60x23 mm left and right 10x0,5mm level of temporal bone frontal bone. Figure 7 abdominal tomography hypodense lesions observed in splenic parenchyma -38- 26 12 and 35mm diameter.
Case 4
58 year old woman with a history of chronic obstructive pulmonary disease with spirometry classification GOLD B, enters service with clinical picture of 10-month history of abdominal pain location epigastric burning, associated with impaired functional class, asthenia, weakness, weight loss not quantified, night sweats and manes in the last 15 days. It had been previously measured in the outpatient setting with report upper gastrointestinal endoscopy with erythematous gastritis corporal and unanswered handling PPI (proton pump inhibitor). In the physical entrance exam with mucocutaneous pallor, generalized hipotrofia, decreased breath sounds in the left lung field and left axillary lymphadenopathy 2x2 cm, adhered to deep, stony planes, Income Study with reporting requirement anemia with blood transfusions (Table 1) and chest radiography is required (Figure 8). For persistent abdominal pain, abdominal ultrasonography was performed without evidence of abnormalities. The patient presented deterioration condition, with signs of systemic inflammatory response and symptoms low breathing, so tomography of the chest was performed (Figure 9). Colonoscopy extension studies showed that only internal hemorrhoids were performed. Blood cultures were negative and also smear negative, study pleural fluid by thoracentesis with lymphocytic exudate and other chronic inflammatory process. The paraclinical showed high total protein, hypoalbuminemia, hypercalcemia and progressive elevation of nitrogenous. It was performed and blood smear bone marrow biopsy (Table 1) with findings consistent with plasma cell neoplasia. This study was completed with bone number (Figure 10). For findings hypercalcemia, renal function impairment, hypoalbuminaemia and lytic bone lesions also multiple myeloma considered aspect.
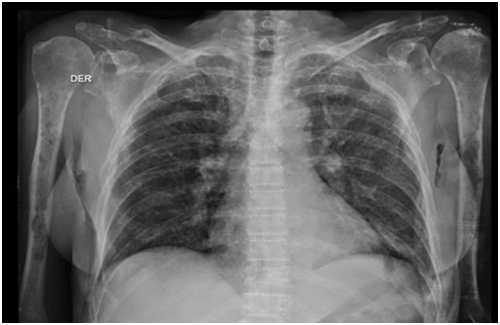
Figure 8 Chest x-ray anteroposterior.
Description: Decreased generalized bone mineralization relative to signs of osteopenia; associated with multiple osteolytic lesions which occupy the entire rib cage and both humeri.
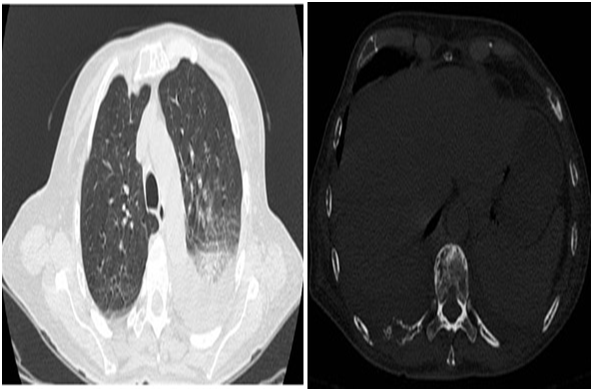
Figure 9 Single image scan of the chest.
Description: Pattern in frosted glass and consolidations with air bronchograms in the middle and lower lobe of the right lung bilaterally. Multiple lesions in costal arches and dorsal vertebrae consistent with lytic lesions.

Figure 10 Plain radiography skull.
Description: osteolytic lesions that project level calvarium to predominance of both parietal are observed.
Case 5
63 year old man with a history of Parkinson's disease Neurology outpatient follow-up entered the emergency room after presenting fall from their own height level trauma right hemisphere, with state of post-trauma postraccion in bed. Physical examination of tachycardic income quantized spiking fevers, dehydrated with evidence of pressure ulcers, need for assistance in activities of daily living; in lower right limb deformity it is evident, therefore imaging study initial approach radiography is performed, which showed lesions lytic aspect especially right hip with a pseudo-permeative pattern so we were extended studies series long bones and further laboratory studies (Table 1). He was taken to study bone scan that reported extensive metastatic disease poliotosica multifocal. Clinically with progressive deterioration and fatal multisystem complications such as neoplastic disease of plasma cells of multiple myeloma type (Figures 11-15).
Bone lesions on imaging studies constitute a finding of great importance and counselor to addressing the clinical condition of a patient admitted to the emergency department or outpatient for certain pathology. While these findings may be addressed when looking for a specific condition, a large proportion is the product of incidental evidence for the study of other entities. The proper interpretation to be given to studies that can be taken depends on decisions that could impact the treatment and / or prognosis of disease. Main tumors involved in the lytic lesions are solid tumors such as prostate, lung and breast; on the other hand the main cause of primary tumor affecting bone level are multiple mieloma.5,9 In analysis of bone images should consider four aspects: density abnormalities, alterations of the structure, signs of proliferation and lesion topography. According to these findings can be established imaging classification to predict the likelihood that the etiology of these lesions is malignant. The system allows this classification is by Lodwick scale and type of periosteal reaction. Factors including Lodwick classification are: the soft tissue involvement, the pattern of bone destruction, the size of the lesion, the transition zone, the margin sclerosis and bone response; accordingly injuries are classified into four stages, where stages III and IV have a malignancy index of 80 and 100% respectively.10 is currently have available a large amount of diagnostic for detecting lesions in the bone marrow aids, however, the initial approach in most cases is still done by plain radiography, which has low sensitivity (about 45%) and a rate of poor discrimination between soft tissues. For the observation of a lytic lesion on an x must be at least 30% destruction of the cortex, and blastic lesions they must be larger than 1 cm with increase of 30% mineralization which explains much of the findings by plain radiography are an expression of advanced stages of different clinical entities; It has the advantage that evaluates largely lesions at high risk of fracture and so it is a low-cost and widely available in the centers. Computed tomography has a sensitivity of 70-100% for the detection of osteolytic lesions, with the disadvantage of having a low sensitivity for detection of bone marrow infiltration, cost, exposure to larger amounts of radiation and also the accessibility to this method study.
Moreover, nuclear magnetic resonance has a sensitivity of 82-100% in detection of bone marrow infiltration and a specificity of 75%, with low sensitivity for detecting lesions periosteal. The best study for detection of bone metastasis is bone scintigraphy, which uses Tc-99m -bifosfonatos, with a sensitivity of 62-100%, and 78-100% specificity. Other studies that can eventually be used include PET scan with high performance tomographic data of the whole body and its uptake level.1,6,10,11 Detecting bone metastases determines changes in management strategy the primary pathology because at the time of detection, the neoplastic disease is at an advanced stage, so that treatment is no longer with curative intent and the role images plays a role mainly in monitoring the established treatment.3,8,12 Multiple myeloma is a bony tumor of primary origin, is the most common with a preponderance male- and involvement mostly axial skeleton malignancy. At diagnosis 70% of patients have lytic lesions and the remaining 90% develop over the course of the disease. Within the diagnostic criteria for multiple myeloma, not only takes into account the conventional radiography, and increasingly using methods more sensitive as CT and PET scan is most important, as well as RMN for diagnosis and monitoring treatment, the most sensitive to NMR marrow infiltration. TAC low dose whole body shows better performance over conventional radiology for the detection of osteolytic lesions.6,13‒15 In this case series 5 patients admitted to a tertiary hospital care, with various clinical manifestations in whom Functional imaging studies showing various types of lytic lesions, with different locations and patterns that suggest a specific pathology are performed are presented. The cases reported here show the lesions of both primary and secondary illustrative type data about the distribution and number of lesions in each particular patient. One consideration to keep in mind is that in principle there should be a high index of suspicion since it is evident that a series of long bones, quick study and low complexity can identify most patients with this type of injury before considering increased sensitivity studies.
University Hospital Hernando Moncaleano Perdomo for allowing the study with patients of this institution.
The authors declare that there is no conflict of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.