MOJ
eISSN: 2574-9935


Research Article Volume 5 Issue 1
PHYSIO MADOU GMBH, Switzerland
Correspondence: Karel Madou, PHYSIO MADOU GMBH, Barzstrasse 3, 5330 Bad Zurzach, Switzerland
Received: March 08, 2022 | Published: April 11, 2023
Citation: Madou K. Wingate-based shuttle run test and limb symmetry index (back to activity algorithm) as the basis for a function-based rehabilitation of a young soccer player with torn ligament injury of the left ankle due to inversion trauma. MOJ Sports Med. 2022;5(1):12-16. DOI: 10.15406/mojsm.2022.05.00110
A paradigm shift is taking place in the treatment of athletes: time-based post-treatment are increasingly being replaced by function-based concepts.
The affected tissue plays an important role, as the healing of a muscle is different in time than the healing of ligaments or bones. Instead of immobilization the affected joint after a ligament injury, it has now been discovered that healing ligaments are dramatically affected by the presence or absence of joint movements. Early, controlled resumption of activity after injury, including repeated strain on injured soft tissue structures such as ligaments and tendons, has profoundly positive effects.
Method: Based on the above-mentioned findings, a female footballer was treated using a practical and function-oriented treatment protocol. The selected and proven function-based treatment concept was the ''back-to-activity-algorithms'' concept, which was used in the rehabilitation of a twenty-year-old footballer who had injured her ankle ligaments after inversion trauma. The performance level of the non-injured limb or the performance level of the affected limb from the immediate pre-injury period, insofar as known / present, serves as the desired performance and is represented as the Limb Symmetry Index, ((LSI) = current level divided by target level) in a number.
Results: Being injured on april 4th 2021, the rehabilitation program started 5 days later. LSI Level I was reached on 29th of April. LSI Level IV on 10th of May. One day later the training with the team was resumed, on May 29 the player played for 45 minutes during a match.
An important component in the treatment of injuries is the affected tissue. The healing of a muscle is different in time than the healing of ligaments or bones. In a time-based rehabilitation concept,1 depending on the scientific view, three (e.g. Hauser et al.)1 or four2 successive phases are distinguished in healing (Table 1, Figure 1)): the hemostatic phase (one to three days), the acute inflammatory phase (three to twenty days), the proliferation phase or regenerative phase (one to 42 days) and the remodeling phase (42 to 180 days and more). Since this approach does not consider what the current performance and resilience are, any increase in load seems to be quite speculative. An early increase in load often means a new injury, a too late increase an unnecessary loss of time and should therefore take place very carefully, considering the sporting requirements of the various sports for the athlete. Especially in sports with physical contact such as handball and football, the requirements are very high and complex.
|
Phase |
Day |
Week |
Main therapeutic action |
Goal |
Running Tool Block (2x5’’+1x10’’) |
SRT-Madou6 30” |
|
1. Haemostasis
|
1-3 |
1 |
RICE, Orthesis, Lymph drainage |
Stop bleeding |
Zero times |
|
|
1a. (2: Mellot) Inflammation |
3-20 |
1-3 |
Mobilisation, functional Movement (low intensity), aerobic exercises |
New framework for blood vessel growth |
W2 (10x) W3 (10x) (Every second day) |
(W2-3) Walking – speed walking |
|
2. (3: Mellot) Proliferation (Granulation)
|
1-42 |
1-6 |
Mobilisation, Stabilisation, Coordination |
Pulls the wound closed |
W4 (10x) W5-6 (15x) |
Week 4-6 Jogging to running |
|
3. (4: Mellot) Remodelling (Maturation) |
42- (?) |
6- (24) |
Mobilisation, Functional training, Strength, Aerobic and Anaerobic |
Prepares Body on Sport Performance |
W7 (15x) W8-16 2 x(10-15x)
|
Week 7-(24) Running to Sprint |
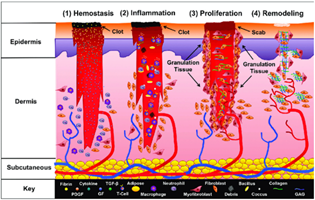
Figure 1 Wound Healing Phases (Mellot et al.)2 is licensed under (CC-BY) license
(http://creativecommons.org/licenses/by/4.0/).
Injured limbs are/were traditionally immobilized/supported by splinting or "casting". While immobilization of the affected joint after a ligament injury has long been prescribed, it has now been discovered that healing ligaments are dramatically affected by the presence or absence of joint movements. The theory is that rest or immobilization prevent further tissue damage in the joint by restricting movement, thereby reducing pain, and swelling. It is also believed that rest can improve recovery time, reduce functional problems, and reduce long-term pain. However, immobilizing a joint with a ligament injury can cause adverse side effects such as synovial adhesions, increasing collagen degradation with decreasing collagen synthesis, and a higher percentage of disorganized collagen fibrils. Despite this evidence, rest, and the RICE (rest, ice, compression, elevation) protocol continue to be commonly prescribed as a first-line treatment for ligament, tendon, and other soft tissue injuries. Immobilization causes the ligament to gradually change from an anabolic to a more catabolic state. In fact, some of these processes have proven to be detrimental to the ligament healing process by suppressing and inhibiting certain cellular processes required to repair the ligament tissue.
Therefore, a rethinking is taking place in the treatment of patients, especially injured athletes. The function-based approach is increasingly replacing the purely time-based approach. In the time-based treatment concept, the 3 (resp 4) individual wound healing phases serve as the basis for the load increases. The first, the acute inflammatory phase, starts within minutes of the injury and continues for the next 48 to 72 hours. During this phase, blood accumulates at the site of injury and platelet cells interact with certain matrix components to change their shape and initiate the formation of clots. The platelet-rich fibrin clot releases growth factors necessary for healing and provides a platform on which many cellular events take place. The (second) proliferation/repair phase begins when immune cells release various growth factors and cytokines that initiate fibroblast proliferation to rebuild the ligament tissue matrix. The formed tissue initially appears as disoriented scar tissue with more blood vessels, fat cells, fibroblast, and inflammatory cells than normal tissue. After a few weeks, the proliferative phase passes into the remodeling phase, in which collagen maturation takes place for months to years after the initial injury. Over time, the tissue matrix begins to resemble normal ligament tissue, but critical differences in matrix structure and function remain. In fact, evidence suggests, that the injured ligament structure is replaced by tissue that roughly resembles histological, biochemical, and biomechanical scar tissue.
Early, controlled resumption of activity1 ,3 after injury, including repeated strain on injured soft tissue structures such as ligaments and tendons, has profoundly positive effects, including improved cellular synthetic and proliferative effects, increased strength, size, matrix organization, and collagen content of ligaments and tendons. Mobilization has been shown to benefit the injured ligament by forming more connective tissue, resulting in a stronger and stiffer tissue than an immobilized counterpart. Exercise leads to increased blood flow to the affected joint and provides the damaged ligament tissue with nutrients and metabolites necessary for tissue repair and healing. Under loading conditions, cells within the ligament recognize tissue strains and react with a change in the tissue. Thus, effect-based therapies have been shown to contribute to healing by stimulating certain cellular actions, involved in the regeneration of ligament tissue.
Based on the above-mentioned findings, a female footballer was treated using a practical and function-oriented treatment protocol. The selected and proven function-based treatment concept was the ''back-to-activity-algorithms'' concept,4 which was used in the rehabilitation of a twenty-year-old footballer who had injured her ankle ligaments after inversion trauma. In addition, a purely run-based instrument was used, the modified ''shuttle-run-test,5,6 according to Madou and Pribish (2020), as this element was not included in the concept. The ''back-to-activity-algorithms'' concept (BTA) is based on the thesis that the best possible functional recovery determines whether to switch to the next level. The BTA concept contains four successive levels (Table 5), which must be achieved successively. Each level distinguishes an A-level (qualitative) and B-level (quantitative). The performance level of the non-injured limb or the performance level of the affected limb from the immediate pre-injury period, insofar as known / present, serves as the desired performance and is represented as the Limb Symmetry Index, ((LSI) = current level divided by target level) in a number. The LSI should be at least 0.85,7 others claim 0.90,8 and, if possible, calculated based on the pre-injury level. Often, however, the non-injured limb is used as a comparison, as this can be tested in any phase.
At each load level, the qualitative test (A level) must first be passed before the quantitative (B level) may be carried out. The assessment of the four qualitative tests is carried out based on specified criteria. However, since they are not part of this work, they will not be discussed further at this point. The quantitative tests are assessed based on a Limb Symmetry Index (LSI), which expresses differences between the affected and the unaffected side in percent.7 If the patient passes the qualitative test (LSI, if quantitative data are available) and the quantitative LSI value of over 85% (90%) is achieved, the level is passed.4,8 The patient can now start with the next level, if he/she strives for the goal of a higher level of stress.9 This depends on the sport being played (Table 3)7 or desired activity of daily living.
|
Test Date |
30’’ Shuttle run (m/t) |
Average m/s |
Meter in 5’’ |
FI (Fatigue Index) |
Goal to be reached6 |
|
12.4.2021 |
60m in 34,58s |
1.73m/s |
8,65m |
0.96 |
3.58-4.5m/s |
|
19.4.2021 |
75m in 34,3s |
2,18m/s |
10,92m |
0,96 |
|
|
26.04.2021 |
90m in 32,4s |
2,77m/s |
13,88m |
0,93 |
|
|
03.05.2021 |
105m in 29,0s |
3,62m/s |
18,10m |
0,97 |
|
|
10.05.2021 |
120m in 29,8s |
4,01m/s |
20,05m |
0.92 |
|
|
17.05.2021 |
135m in 33,0s |
4,09m/s |
20,45m |
0,90 |
|
|
26.05.2021 |
135m in 32,8s |
4,11m/s |
20,58m |
0,79 |
|
|
31.05.2021 |
135m in 32,7s |
4,12m/s |
20,61m |
0,79 |
|
|
07.06.2021 |
135m in 32,1s |
4,20m/s |
21,03m |
0,89 |
|
Table 2 Wingate Shuttle Run Test6 (Madou) as Basic Tool for the Running Program
|
Limb Symmetry Index Test and level I - IV |
|
Targeted Index 0,85 – 0,90 |
|
Possible Activity as Level Goal is reached |
|
Level I – IV
|
Description |
Test A |
Test B |
|
|
Level I |
On foot on 30cm bench behind P |
60s balance test (wobble board) - Time recorded. |
30s one legged 105° squat Number of repetitions |
Sports without jumps (e.g. Golf, Hiking, Biking) |
|
Level II |
3 seconds in balance after (last) landing |
3s Single Leg Hop - Distance |
3s Three Leg Hop - Distance |
Sports without turns and stops (e.g., Jogging/Running) |
|
Level III |
3 seconds in balance after (last) landing |
3s Three Cross Hops - Distance |
30s Side to Side Hops – Number (30cm) |
Sports with side hops, stops and turns (e.g., Tennis, Ski) |
|
Level IV |
As Level IIA: Side hops (left/right) are added. |
90° One Legged Hop – Distance of left and right hop is added |
30s Square Hops – Number (30cm) |
Sports with fast turns, stops (e.g., Basketball, Soccer) |
Table 3 Overview of Lower Limb Symmetry Index Test (Level I-IV A and B)
Level 1: Consists of two balance tests, the 60'' balance test (wobble-board) and the balance squat. The Balance Squat, i.e., a one-legged squat, tests the stability of the joint to be tested in the sagittal level.
Level 2: Consists of a Balance Front Hop Test and the Front Hop Test. While the quality of the former is decisive, the front hop only depends on the length of the jumps in the side comparison.9
Level 3: Examines the frontal plane using Balance Side Hop and the Side Hop Test.
Level 4: Includes the frontal and sagittal level through the 90° Balance Hop and the Square Hop Test. In the quantitative tests from level 3 and 4, it is not the distance, but the number of correct jumps that is decisive.9
The load level of the running element (Table 4: 30 seconds and 15m modified shuttle run tests)4,5 is determined by a weekly repeated test, starting with walking speed. The average running speed (= Mean Lap Velocity (MLV)) is calculated as well as a Fatigue Index (FI). The average running speed (in m/s) serves as a calculation basis to determine a distance length that must be covered repeatedly in 5 seconds. 2 distances, covered in the calculated running speed, are alternated with a distance in half the running speed (in 10 seconds). Such a block (2 x 5 seconds and 1 x 10 seconds) is initially repeated up to 10 times every other day (Table 5). If the MLV cannot be adhered to for two consecutive laps, the running program will be terminated prematurely.
|
Test protocol (Shuttle Run)6 |
|
|
A distance (lap) of 15m is marked on a flat indoor surface |
To ensure the same circumstances
|
|
Marker is a traffic cone |
Because of visibility |
|
The lap is covered going back and forth (turning point) |
Not around the cone |
|
The time is 30 seconds (plus one extra lap) |
To ensure, participant does not ‘’finish’’ |
|
HLV (Highest Lap Velocity) and LLV (Lowest lap Velocity)⁵ as well as MLV are calculated |
MLV to calculate training distance. HLV and LLV to calculate FI |
Table 4 Test Protocol ‘’Modified 30 Seconds and 15m shuttle Run Test’’6
|
Training protocol running
|
|
|
Running distance = 5 x latest MLV |
|
|
P must run a number of blocks |
One block = 2 x Lap in MLV (5’’) and 1 Lap in half MLV (10’’) |
|
In week 1 to 4 a total of 10 blocks
Week 5 to 7 a total of 15 blocks
From Week 8-12 the program of 10 blocks is executed 2 times (2 Minutes rest)
From Week 13-16 the program of 15 blocks is executed 2 times (2 minutes rest) |
No rest between blocks |
|
Every second day.
|
Training is stopped if P cannot keep the MLV for more than one lap. |
Table 5 Test Based Training Protocol
Rehabilitation time-protocol
The inversion trauma occurred on April 4th, 2021 (Easter Monday) during a football match among friends. The physiotherapy program started on 9.4.2021. Balance (one legged) was only possible for 45 seconds (pain-related). The ankle joint was painful and swollen (photo in Table 6). The joint showed no blue discoloration. The medical diagnosis was rupture of LFTA (ligamentum fibula-talar anterior) and LFC (ligamentum fibula-calcaneal). The patient was asked to tape her foot during each training. On 12.04.2021 the first ''shuttle run test'' was carried out (see Figure 2). The patient walked 60 m (slightly limping) in 34.68 seconds. The average speed (MLV) was 1.73m/s. Based on this test; a running (walking) program was tailormade. The P had to go 5 seconds there and back in the MLV (= 5 x 1.73m = 8.56m) followed by the same distance in 10 seconds (0.87m/s). This block had to be completed 10 times every other day in weeks 1 to 4. Afterwards as needed this was increased if not yet started during the team training. The LSI (Limb Symmetry Index) tests (B) were started along with the running training/running tests. The tests were given as a home program. On 26.04.2021 it was possible to switch to running. On 11.5.2021, besides physiotherapy, the team training was started again in a dosed way. On May 22 the player returned to play for 15 minutes during a match and for 45 minutes on May 29.
|
Rehab-Phases |
Rehab-Dates |
Level (B and A) Passed |
First Test Result |
Passing Result |
|
Trauma (Inversion) |
Inversion Trauma 4.4.2021 |
9.4.2021 |
|
|
|
Start shuttle- ‘’run’’ W = walking R = running |
12.04.2021 (W) 19.04.2021 (W) 26.04.2021 (R) 03.05.2021 (R) 10.05.2021 (R) 21.06.2021 (R) |
15.04.2021 |
60m (MLV 1.73m/s) 75m (MLV 2.18m/s) 90m (MLV 2.77m/s) 105m (MLV 3.62m/s) 135m (MLV 4.01m/s) 135m (MLV 4.23m/s) |
|
|
LSI Level I |
A on 29.04.2021 |
B on 29.04.2021 |
A 45s B 9 squats |
A 60s B 14 squats |
|
LSI Level II |
A on 03.05.2021 |
B on 03.05.2021 |
A 41cm B 41cm |
A 106cm B 377cm |
|
LSI Level III |
A on 10.05.2021 |
B on 10.05.2021 |
A 220cm B 50 reps |
A 402cm B 56 reps |
|
LSI level IV |
A on 10.05.2021 |
B on 17.05.2021 |
A 100cm B 70 reps |
A 100cm B 70 reps |
|
Return to Team-training |
11.05.2021 |
|
|
|
|
Return to Play |
22.05.2021 (15 Minutes) |
29.05.2021 (45 Minutes) |
|
|
Table 6 Overview of Rehabilitation Results from Day of Injury until Return to Play
A paradigm shift is taking place in the treatment of athletes9 with injuries to the lower extremity: purely time-based post-treatment concepts are increasingly receding into the background and are increasingly being replaced by function-based concepts.
Making the decision to ‘’return to activity’’ (training and competition), based on the above-mentioned rehabilitation protocol, is easy to plan as long as it concerns Level I and II sports. In Level III and especially Level IV sports, such as soccer, the player should be introduced to the team training under close supervision, as the training load often is situation dependent. The role of the therapist should not be underestimated, and he should work closely together and coordinate with the coaches who are primarily responsible. In professional teams, after a period of purely rehabilitation treatment, an injured player returns to team training after completing an individually offered physical bridging program with a rehabilitation coach. In a non-professional environment this switch from purely individually guided rehabilitation treatments to the team training is highly crucial and often underestimated. The risk of being injured again is greatest in the early returning phase to team training. Therefore, the final return to the team requires not only a well planned and executed rehabilitation program but also a lot of tact and instinct from those responsible.
The function-based treatment of sports injuries is increasingly replacing the time-based approach and can be used very successfully, especially on the extremities, but must be tailored to the individual athlete and remain under constant medical control. As a treatment basis, the back-to-activity-algorithm is used, which, for field athletes, can be combined with a test-based running program. The basis of this running program is the Wingate-based Shuttle Run Test according to Madou and Pribish.6 The individual steps of the treatment should be discussed with the patient to achieve optimal compliance and motivation, The conditions to change to the next level of the rehabilitation protocol are very clear and help the patient to adhere to the specifications. This case study shows the individual elements of the therapeutical program and its progress in a professional soccer player after an inversion trauma.
None.
None.

©2023 Madou. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.