MOJ
eISSN: 2574-9935


Case Report Volume 2 Issue 5
Orthopedics and Traumatology Clinic, Ankara Diskapi Yildirim Beyazit Education and Research Hospital, Turkey
Correspondence: Halis Atil Atilla, Orthopedics and Traumatology Clinic, Ankara Diskapi Yildirim Beyazit Education and Research Hospital, Ziraat Mahallesi, ?ehit ?mer Halisdemir Caddesi - No:20 D??kap? Alt?ndag/Ankara, Turkey, Tel +90 545 214 28 89
Received: January 01, 1971 | Published: December 26, 2018
Citation: Akdogan M, Atilla HA, Barca F. Pediatric Achilles tendon laceration: a case report and systematic review of literature. MOJ Sports Med. 2018;2(5):153-156. DOI: 10.15406/mojsm.2018.02.00066
Pediatric Achilles tendon laceration is a less reported injury type. In this report, a case of Achilles tendon laceration of 12 years old boy was presented and a review of the existing literature on the Achilles tendon laceration in the pediatric age group was performed.
Keywords: pediatric Achilles tendon laceration, child Achilles tendon laceration
Achilles tendon is the largest tendon of the body. Main function of the tendon is to plantarflex the foot, while it also contracts eccentrically during walking to prevent excessive dorsiflexion and lurching.1 Achilles tendon rupture is a common injury seen in 35-40 years of age during recreational sports and causes severe disability. There are many studies about treatment and follow-up of Achilles tendon rupture and both surgical and conservative treatment modalities are reported. On the other hand Achilles tendon laceration is a much less reported injury.2 The ankle injury of Achilles according to the myth was also a laceration injury. Achilles, who gave his name to the tendon, was injured with an arrow posterior to the ankle and died from bleeding or could not fight again due to permanent disability.3 In this report, a case of Achilles tendon laceration of a 12 years old boy was presented and a review of the existing literature on the Achilles tendon laceration in the pediatric age group was performed.
From the PUBMED database, reports with "Achilles” and “laceration” and “children" keywords were scanned from 01.01.1980 to 22.10.2017. The summaries of the reports that were found after the PUBMED search were reviewed by two authors (AA, FB). Reports that are related to the subject, including the patients from the child age group and the studies in English are obtained in full texts. Due to the confusion of terminology about “laceration” and “rupture” in Achilles injury, PUBMED scans were performed with keywords “Achilles laceration”, “Achilles rupture pediatric”, “Achilles rupture children” in order not to miss any related report. Among the abstracts obtained from this screening, clinical studies with adults belonging to the adult age group and patients with rupture injuries; experimental and biomechanical studies were excluded. Studies which are not in English and that have not mentioned about treatment were also excluded. The overlapping articles were removed. References of included articles were also scanned. Articles containing child patients with acute lacerations and treatment methods, outcomes and mechanisms of injury were included in the study. Informed consent was taken from the patient’s parents.
A 12-years-old boy was consulted to our Emergency Orthopedic Clinic with a wound on the left Achilles tendon after a glass cut. The wound was in the form of a flap approximately 4 cm wide with an opening facing proximally. Skin of the wound had been sutured at another center (Figure 1). The patient had normal neurovascular examination. Physical examination showed a nonreactive Thompson test and a reduced plantarflexion strength compared to the contralateral side. Ankle graphs were compared bilaterally; it was observed that the Kager triangle was disrupted on the injured side (Figure 2). Ultrasonographic evaluation of the diagnosis confirmed that the integrity of the Achilles tendon was deteriorated. Sutures were removed and emergent irrigation and debridement was performed. On the same day, patient was operated in prone position with an application of pneumatic tourniquet. When the wound was explored, distal stump of Achilles tendon was seen with well-defined margins. The proximal stump of the tendon was not visible from the incision site and retracted proximally. Because of retraction, the wound was extended about 2 cm from the medial aspect to the proximal side. There was a gap of about 4 cm between the two stumps of the Achilles tendon. Proximal stump was brought to the incision site by milking of gastrocnemius muscle belly and getting the knee to flexion. Figure 3 with knee flexion and ankle plantar flexion, the two stumps of the Achilles tendon were approximated at an appropriate tension and repaired by modified Kessler technique with No. 2 Ethibond EXCEL (ETHICON, Johnson & Johnson, Tokyo, Japan) suture. Subsequently, the repair was supported with interrupted 2-0 Vicryl (ETHICON, Johnson & Johnson, Tokyo, Japan) sutures. Paratenon tissue was found around the tendon and repaired with a 3-0 Vicryl suture (ETHICON, Johnson & Johnson, and Tokyo, Japan) (Figure 4). After closure of skin, a long leg circular cast was made with ankle in neutral position, and knee flexed about 30 degrees. Controlled weight bearing was allowed after four weeks and the cast was removed in the sixth week. At the post-operative six months follow-up, the foot plantar flexion strength was the same as the contralateral side. The heel rise test was equally observed on both feet. Achilles tendon total rupture score (ATRS) was assessed as 97. The gait was considered normal. No wound complications were encountered.
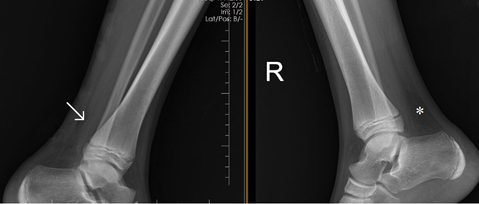
Figure 2 The area marked with an arow on the left shows disrupted Kager triangle compared to contralateral side (marked with asterisk).
PUBMED database search with the terms "Achilles laceration children" yielded seven studies that have been published between 01.01.1980 and 22.10.2017. Of these seven studies, one was considered as a case report of a child with Achilles tendon laceration.4 One of the other studies5 was in Chinese, three studies,6–8 were excluded because of not mentioning about whether surgery was done or about treatment method, one9 had not mentioned how many patients were children, one10 was about secondary wound site complications. From results of the "Achilles laceration" search, 45 studies were yielded. From abstracts, two studies were found to be relevant. One of these two studies4 coincided with those previously included. There was one study that has involved pediatric patients with Achilles tendon laceration11 but number of pediatric patients in the study and the treatment method applied to the disease was not specified so this study was excluded. The only study associated with laceration in the search made with the search term "Achilles rupture pediatric" was a case report that have been included previously.4 One case report12 was included from the search result made with the search terms "Achilles rupture children". When the references were searched for included studies, one study was also included13 (Figure 5) (Table 1).
Study |
Patients |
Mechanism of injury |
Treatment |
Follow-up and results |
Vasileff et al.4 |
10-year-old boy |
Partial laceration six weeks ago and second trauma – total rupture |
Debridement and repair (Bunnell) |
Orthoses removed in ten weeks, mild plantarflexion weakness |
Massoud et al.13 |
24 patients (6 children) |
Acute |
Krackow and reinforcement sutures through calcaneus tunnel |
23 perfect, one good results (with wound adhesion) |
Tudisco et al.12 |
7-year-old girl |
Overlooked tendon injury after skin laceration eight weeks ago – retracted tendon |
Repair (Bunnell) and plantaris tendon augmentation |
Cast in full equinus for two weeks, then less equinus, cast removed in five weeksr, asymptomatic in three years after physical treatment |
Table 1 Studies included after PUBMED searches
Achilles tendon rupture in adults is a very common sports injury of the ankle.14 It is very common especially in the fourth decade. In child age group, the Achilles tendon rupture is an uncommon and rarely reported pathology. In this age group, it appears as avulsion from the calcaneus insertion. There is no widely accepted treatment approach. Only one author reported that in a seven-year-old boy, he successfully treated an injury other than avulsion in a conservative manner.15 Achilles tendon laceration is rarely reported in the adult age group. A large series of 205 patients16 underwent surgery for complete or partial lacerations and the results were good. Lennox et al.,17 İnvestigated follow-up of 20 patients with Achilles tendon injury including Achilles tendon laceration and results of patients with primary open Achilles laceration were perfect with primary repair.17 To the best of our knowledge, this is the first report in a child with an Achilles tendon laceration treated with early surgical intervention. Superficial soft tissue injury can be accompanied by other underlying pathologies. Overlooked tendon injuries have already been reported in hand injuries.18 The consultation of the current wound in a sutured manner reveals once again the importance of clinical suspicion and examination in such injuries. It is important to examine and determine whether tendon and other neovascular structures are damaged under the skin laceration around the Achilles tendon, just as in the hand injuries. Recognition of partial tears of the Achilles tendon by emergency or primary care physicians is important. Partial tears can turn into complete ruptures over time. In a study involved in our review,4 the possible partial rupture after the first injury in a hockey injury was overlooked, and then it became a complete rupture with a relatively minor injury. Negative Thompson test with physical examination is not enough and imaging with X-ray, USG or MR and in case of a suspect with partial rupture, exploration of wound site during irrigation may be helpful for diagnosis and treatment of tears that may require repair. Decision of Achilles tendon laceration in our case was made by comparing Kager triangle with contralateral X-ray (Figure 2). It was found that the triangles of all patients with acute Achilles tendon ruptures were lost in lateral graphs.19
Conservative treatment of Achilles tendon ruptures after closed injury has comparable results with surgical treatment and is accepted as a widespread and routine treatment option.20 However, we anticipate that the results of conservative treatment may be poor after such a serious gap and retraction in laceration injuries. In the experimental models reported, Achilles tendon injuries are created with a sharp dissection, but Achilles tendon injury is considered as a closed and intrinsic rupture. As a matter of fact, in the pre-1980 literature, it can be seen that these concepts (rupture, tear or laceration) are used instead of each other.21–23 An acute overload is thought to be present on the existing chronic changes in the mechanism of rupture,24 so laceration is supposed to be a different injury from closed rupture. Injury to childhood Achilles tendon can be considered as similar to tenotomy applied in Ponseti method (clubfoot treatment). Even though the age group for the Ponseti method is much younger, it is shown ultrasonographically that the tendon cannot recover to its old structure even after two years.25 It can be thought that the healing of a tendon completely deteriorated in the age of active gait may be even more difficult. A case report stated that after a missed Achilles tendon laceration proximal stump retracted too much and repair could be done very tightly.12 Degenerative appearance is often accompanied by a closed injury pattern in rupture; some of the fibers do not allow the stumps to go away from each other. It has previously been reported in the literature that the proximal stump is retracted and the flap must be made to skin for exposure.11 Wray et al.,26 reported that the Achilles tendon tenotomized in the cadaveric study could be approximated by the ankle and knee joint position.26 Our patient could be followed up conservatively by casting as such. However, just as in the hand flexor tendons,27 it is seen in our case that there is difference between the tendon gaps of spontaneous rupture and complete laceration of the tendon (Figure 3). A cadaveric study without muscle tone may not be sufficient alone to achieve an idea about tendon convergence in acute laceration. Roberts et al.,28 observed in their Achilles laceration study that there was marked difference between stress tolerance of the repaired and non-repaired tendons.28
Spontaneous rupture and laceration of Achilles tendon are different injuries. In the case of rupture, there is little continuity of fibers which holds the stumps closer but there is a complete disruption of continuity of fibers in laceration. It is seen that powerful gastrocnemius and soleus muscles, just like in hand flexor tendon injuries, retracts the proximal stump of tendon. Therefore, treatment of laceration should be evaluated differently and surgical treatment should be performed even in pediatric patients with complete laceration.
None.
Authors declare that there is no conflicts of interest.

©2018 Akdogan, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.