MOJ
eISSN: 2574-9935


Research Article Volume 5 Issue 2
1Department of Orthopaedics, Jawaharlal Nehru Institute of Medical Sciences Imphal, India
2Arthroscopy & Sports Surgery, Apollo Multispecialty Hospital Kolkata, India
Correspondence: T Pausiam, Senior Resident, Department of Orthopaedics, Jawaharlal Nehru Institute of Medical Sciences Imphal, India
Received: August 19, 2022 | Published: August 30, 2022
Citation: Pausiam T, Mallick MNB, Arya P. Early outcome of medial meniscus posterior root repair in elderly- a clinical and radiological study. MOJ Sports Med. 2022;5(2):43-46. DOI: 10.15406/mojsm.2022.05.00116
Meniscus functions as a load distribution, shock absorption, proprioception, lubrication, and stabilization. Meniscal roots anchor the medial and lateral menisci to the tibial plateau, allowing the meniscus to disperse axial loads into hoop stresses. Currently, repair of meniscus root is the treatment of choice for meniscus root tears. The aim of this study is to evaluate the clinical and radiological outcome of medial meniscus posterior root repair in elderly patients.
Material and Methods: It is a prospective clinical and radiological study in 10 consecutive patients, who met the inclusion criteria and operated between June 2017 to June 2018 by a single surgeon. Patients were followed up for clinical and radiological evaluation by MRI. Duration of follow up ranges from 24 to 36 months.
Results: Of the 10 patients (2 male and 8 female) with the mean age of 64 years. Mean follow-up period is 30 months. Mean BMI of the patients is 26.14 + 1.95 kg/m2. The difference in pre-operative and post-operative patient’s IKDC and Lysholm scores are significant (p value < 0.05). 2 patient showed complete healing of meniscus root, 8 patients showed partial healing and there was no repeat tear. Meniscus extrusion decreased from 5.2 + 0.8 mm preoperatively to 4.13 + 0.55 mm postoperatively.
Conclusion: In this study, the outcomes after posterior medial meniscus root repair in elderly results in significant improvements in function, symptoms of pain, and activity level in spite of partial root healing in MRI in this short term follow up.
Keywords: root tear, transtibial tunnel, suture post, degenerative changes, meniscus extrusion, meniscus root repair
MRI, magnetic resonance imaging; BMI, body mass index; IKDC, international knee documentation committee
Posterior medial meniscus root tear is mainly due to degenerative meniscus disease and common in elderly patients.1,2 Root tears are similar to a total meniscectomy because it alters tibiofemoral contact pressures and area.3–6 Early diagnosis and treatment is important in age above 50 years4 because progression of osteoarthritis can be delayed.7,8
However, age has been considered a poor prognostic factor in root healing and elderly peoples are usually not considered for root repair. Thus, our aim in this study is to assess the outcome of posterior medial meniscus root repair in elderly patients by assessing clinically and radiographically.
A prospective clinical study conducted in 10 patients from June 2017 – June 2018. Informed consent was taken from all the patients. The period of follow up ranges from 24 -36 months. The patients had a history of trivial trauma (squatting and minor slippage) or can’t recall an inciting event of injury. Commonly presented with posteromedial knee pain worsens on deep squatting or rising from chair. Ligamentous examinations are normal. Diagnosis was based on magnetic resonance imaging (MRI). Signs of posterior medial meniscus root tears on MRI are breach of high signal intensity, loss of posterior insertion of medial meniscus in axial, coronal images and a normal dark meniscus replace by high signal intensity ghost meniscus in sagittal images. It was often associated with stress injury pattern in corresponding femoral and tibial condyles with meniscus extrusion. Meniscus extrusion is measure by a vertical line drawn at the margin of medial tibial plateau and a second vertical line drawn at the outer margin of the medial meniscus. The measurement between the two vertical lines is define as the width of meniscus extrusion.9
Clinical outcome is assessed using international knee documentation committee (IKDC) and Lysholm scores. Radiological outcome is assessed using MRI at 12,24, and 36 months respectively. For evaluation of meniscal extrusion9 and root healing using Kim et al.,10 criteria, in which a complete healing is describe as a confirmed continuity in all sagittal, coronal, and views, partial healing as loss of continuity in any one view and repeat tear as no continuity in any view.
Surgical procedure
All the patients underwent posterior medial meniscus root repair by transtibial tunnel pull-out technique. To confirm the diagnosis, a diagnostic arthroscopy is performed and a tibia socket is created for easy passage of drill guide. Through the anteromedial portal, drill guide is inserted and a guide tip is placed at the footprint of meniscus root. Medial to the tibial tuberosity a skin incision of 2-4cm is made and the outer cannula is impacted into the anterior cortex of the tibia. Through the inner cannula a guide wire of 2.4-mm is drill till it reach the tip of the guide intra-articularly. A 3.5-mm Arthrex FlipCutter with 8 mm diameter head is drilled through the same tunnel of the 2.4- mm wire. The FlipCutter head is deployed inside the joint and the tibia is retro drilled up to a depth of 5-mm to create socket for fixation of meniscus root. A number 0-Fiberwire (Arthrex) suture loop is passed in the posterior medial meniscus root with a self-retrieving suture passing device (Firstpass mini, Smith& Nephew). To create a cinch configuration the Fiberwire suture is passed through the loop and tightened around the posterior medial meniscus root. A second number 0 -Fiberwire (Arthrex) is similarly used to create a second repair point in the root. All the sutures are shuttled down through the tibial tunnel to exit at anteromedial tibial surface. To fixed the repair meniscus root into the tibial socket a moderate tension is applied.. With knee in 30° of flexion both the sutures are tied over suture post fixed on anteromedial tibial surface 1cm distal to tibial tunnel. Using a probe, the stability of fixation is confirmed (Figure 1).
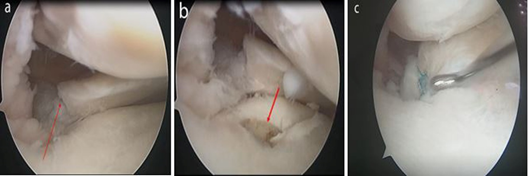
Figure 1 Arthroscopic images of a left knee.
a) Medial meniscus posterior root tear (red arrow). b) Tibial socket for root fixation (red arrow). c) Medial meniscus posterior root after repair.
Rehabilitation protocol
Patients remained non weight bearing in a straight leg brace for the first 6 weeks after surgery. Passive range of movement exercises from 0-90 degree is started in post-operative day 1. After 2 weeks advance knee flexion as tolerated and deep knee flexion is avoided up to 4 months postoperative.11
Statistical Analysis: All the data were analysed using SPSS Statistics Desktop 22.0. For comparison of preoperative and post-operative values, a paired t test is used. Preoperative and post-operative values are considered significant if the p-value is < 0.05.
Out of 10 patients, 2 are male and 8 are female. The male: female ratio is 1:4. Mean age of the patient is 64 years (Range, 60 – 75 years). The mean follow-up period is 30 months (Range, 24-36 months). Mean BMI of the patients is 26.14 + 1.95 kg/m2 (Range, 22.5 – 29.2 kg/m2) (Table 1). No patients complain of pain, catching or giving way. No patient had joint line tenderness or effusion. The difference in mean preoperative and postoperative patient’s IKDC and Lysholm score are significant (Table 2). Follow-up MRI is performed in all the patients in which only 2 patients show complete meniscus root healing (Figure 2), 8 patients show partial meniscus root healing (Figure 3) and there was no case of repeat tear. Mean extrusion of meniscus decreases from 5.2 + 0.8 mm (Range, 4 -7 mm) preoperatively to 4.13 + 0.55 mm (Range, 3.5 - 5.2 mm) postoperatively, respectively.
|
Cases |
Age/Sex |
Laterality of knee |
Kellgren- Lawrence grade |
Duration of pain (in weeks) to Surgery |
BMI (kg/m2) |
|
1 |
60/ Female |
Left |
II |
8 |
25.9 |
|
2 |
64/Female |
Left |
II |
6 |
26.33 |
|
3 |
75/Female |
Right |
II |
10 |
24.93 |
|
4 |
64/ Female |
Left |
II |
9 |
27.33 |
|
5 |
61/Male |
Right |
II |
11 |
26.6 |
|
6 |
67/Female |
Left |
II |
7 |
25.5 |
|
7 |
62/ Female |
Right |
II |
14 |
24.57 |
|
8 |
61/Female |
Left |
II |
9 |
28.5 |
|
9 |
65/Male |
Left |
II |
12 |
29.2 |
|
10 |
63/Female |
Left |
II |
10 |
22.5 |
Table 1 Patients demographic data
|
Score |
Mean Preoperative |
Mean Final follow up |
p value |
|
IKDC score |
31.9 + 5.34 |
74.1 + 3.28 |
<0.00001* |
|
Lysholm score |
46 + 4.4 |
79.5 + 3.3 |
<0.00001* |
Table 2 Preoperative and postoperative clinical scores
Note: Values are mean + Standard Deviation, *significant if the p value is < 0.05
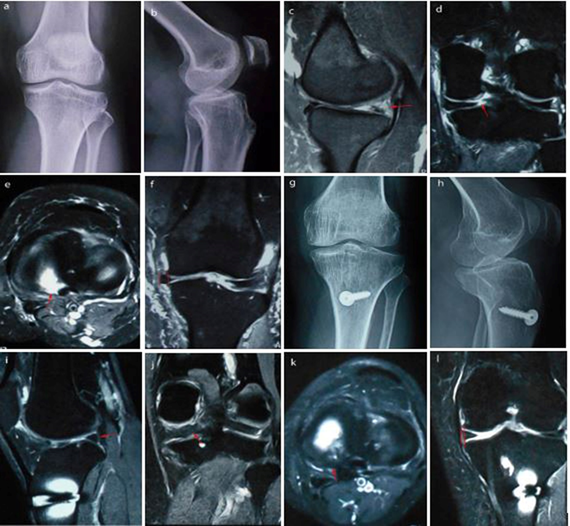
Figure 2 Preoperative left knees.
a) Anteroposterior. b) Lateral radiographs. c) Preoperative MRI showing root tear (red arrow) in sagittal. d) Coronal.
e) Axial. f) Meniscus extrusion (measured between two red vertical lines). g) Radiographs at 3 years follow up anteroposterior. h) Lateral view. i) MRI scans at 3 years follow up showing complete healing (red arrow) on sagittal view. j) Coronal view. k) Axial view. l) Coronal view showing decrease meniscus extrusion (measured between two red vertical lines)
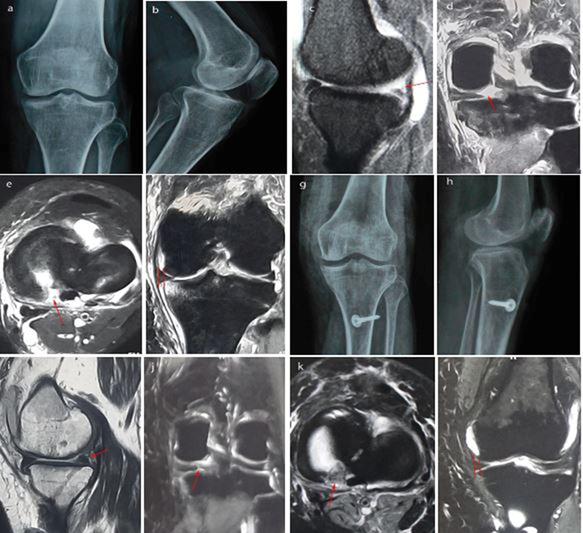
Figure 3 Preoperative left knee.
a) Anteroposterior. b) Lateral radiographs. c) Preoperative MRI showing root tear (red arrow) in sagittal. d) Coronal. e) Axial. f) Meniscus extrusion (measured between two red vertical lines). g) Radiographs at 3 years follow up anteroposterior. h) Lateral view. i) MRI scans at 3 years follow up showing partial healing (red arrow) on sagittal view. j) Coronal view. k) Axial view. l) Coronal view showing decrease meniscus extrusion (measured between two red vertical lines)
The goal of Meniscal root repair is to restore Meniscal function, thereby relieve pain, improve mobility and delaying or ultimately arrest the progression of osteoarthritis. But few literatures have described the outcome of meniscus root repair in elderly. Following root tear, the peak contact pressure of knee joint increases up to 25%. if left untreated, it results in accelerated articular cartilage degeneration causing painful bone oedema12,13 Early degenerative joint disease14,15 and subchondral insufficiency fractures of the knee (SIFK).7 The cultural requirement in Asian population to sit in hyper flexed knee result in higher incidence of meniscus root tear16 Patients age should not be the only criteria to exclude meniscus root repair, various factors like grade of osteoarthritis , high body mass index, the ability to co-operate with the rehabilitation.17 A high BMI result in increased pressure over the knee joint, causing higher risk of Meniscal injuries.18 Patients with chondral lesion of grade 3 and 4 Outerbridge and varus knee greater than 5 degree had poor outcome.19 The two most commonly used repair techniques are suture anchor repair20,21 and transtibial Meniscal root repair.22 The advantage of transtibial technique as compare to suture anchor technique is, it provide a wider anatomical footprint for meniscus root fixation, release of various biological factor while drilling enhanced root healing.4,22–26 In a human cadaver study by LaPrade et al22 comparing the biomechanics of single and double Transtibial Tunnels, they concluded that both techniques have similar biomechanical properties. In a 5- year follow-up, meniscus root tear treated by partial meniscectomy, 35% of the patients require total knee arthroplasty.27 Regarding root healing, using only MRI for assessing meniscus to bone healing is unsatisfactory and greater emphasized should be made to arthroscopically recheck for root healing.28 Our study shows that, the clinical improvement after posterior medial meniscus root repair in elderly patients had a significant outcome based on IKDC score and Lysholm score. However, radiological outcome shows that only 2 out of 10 patients had successful complete meniscus root healing but meniscus extrusion is significantly decreased. In spite of short term follow up, the clinical and radiological outcome are comparable with various published document. But various clinical studies have had conflicting results in meniscus extrusion following root repair. In a study by Kim et al.10 in repair group, mean age is 55.2+ 8.7 (Range, 42-65 years). Male: female ratio is 1:5. The mean period of follow-up is 48.5 months. Average Body mass index is 26.81+2.57 kg/m2. The mean Lysholm score and IKDC increased preoperatively from 56.8+5.5 and 42.6+6.3 to 85.1+5.8 and 77.2+ 6.3 postoperatively, respectively. Radiologically, 17 cases (56.7%) show complete root healing and extrusion of meniscus decrease from 3.13mm to 2.94 mm post-operatively.
Feucht MJ et al.,14 study shows that, 62% show complete root healing, 34% show partial healing, and failed in 3% in a mean period follow-up of 30.2 months. Meniscus extrusion is decrease in 56% and Lysholm score improve significantly. Seo HS et al.,15 conclude from their study that, the mean Lysholm scores improved significantly, but no case of complete root healing till last follow-up. In their study they don’t evaluate the meniscus extrusion.
LaPrade et al.,17 compare the outcomes of posterior meniscus root repair in patient age less than 50 years and above 50 years. The mean age in patient above 50 years is 58 (Range, 51.3 -65.7). The age cohorts, Lysholm and WOMAC scores shows significant clinical improvement. All surgical failures are in patients age less than 50 years whereas no failure in patient age above 50 years. The limitation of their study is that, they did not evaluate the rate of meniscus root healing postoperatively. In a study by, Moon HK et al.,19 the mean VAS pain score and Lysholm score improve significantly. On their MRI evaluation, root healing is shown in 90.3% of the patient show root healing. In spite of 90.3% root healing, the meniscus extrusion increased from 3.6 + 1.2 mm to 5.0 + 1.7 mm (P < .001). In a study by Jung et al.,21 5 patients showed complete healing, 4 patients showed partial healing, and 1 showed no healing in a mean follow-up period of 30.8 months (Range, 24-40 months). Meniscus extrusion decrease from 3.9 mm (Range, 2.2-7.1mm) preoperatively to 3.5 mm (Range, 1.2-6.1 mm) postoperatively. They characterize the causes of incomplete root healing is due to the fact that, firstly, most of the root tear are radial tear and repaired radial tear has more repetitive distraction forces from weightbearing as compare to horizontal tears. Secondly, a protection postoperative weight bearing of 6 weeks might not be sufficient for healing. Thirdly, improper indications for surgery. AlaiaM et al.,29 concluded that, the clinical IKDC score and Lysholm score increase significantly. But radiologically out of 18 patients only 1 patient show complete root healing and meniscus extrusion increased from 4.74 mm to 5.98 mm post-operatively (p< 0.02). Only 1 of 18 patients in the study by Kaplan et al.,30 had complete root healing (5.5%) and meniscus extrusion increased from 4.74 ± 1.7mm to 5.98 ± 2.8 mm post-operatively. They concluded that, chondral wear, subchondral fracture, meniscus extrusion are the reliable indicators of Meniscal integrity.
Thus, we concluded that, the outcomes after posterior medial meniscus root repair in elderly results in clinical improvement of function, symptoms of pain, and activity level of the patient, in spite only 2 cases of complete root healing in MRI in this short term follow up. There are various limitations. Firstly, the number of patients is less. Secondly, we did not evaluate anatomic foot print of tunnel placement. Thirdly, second-look arthroscopy is not performed, and thus, the real status of root healing cannot be determined. Fourth, duration and follow up is short for evaluation of progression of root healing and osteoarthritis after surgery.
None.
The author declares that there are no conflicts of interest.

©2022 Pausiam, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.