MOJ
eISSN: 2379-6162


Conceptual Paper Volume 4 Issue 1
Hairmyres Hospital vascular and endovascular unit Europe, UK
Correspondence: Bryce Renwick, Hairmyres Hospital vascular and endovascular unit G75 8RG Scotland, UK, Tel 013-555-845-16
Received: October 05, 2016 | Published: January 20, 2017
Citation: Montgomery BRS, Mardurska M, Pickard C, et al. Viabahn in unusual situations the gore heparin-bonded bioprosthesis in complex arterial pathology. MOJ Surg. 2017;4(1):1-3. DOI: 10.15406/mojs.2017.04.00055
The Gore Viabahn vascular heparin-bonded bioprosthesis has been available for several years and has a proven track record in complex superficial femoral artery and iliac segment disease.1–3 However the flexibility and conformability of the device lends itself to treatment of other complex arterial lesions. We present 3 recent cases of endovascular management of complex arterial problems that were successfully treated by the Viabahn device.
A 62-year-old lady in otherwise good health underwent CT scanning for abdominal pain. The incidental finding of a 2.5cm aneurysm of the common hepatic artery was identified. The aneurysm was felt by the multidisciplinary team to represent a significant rupture risk.4 The patient was worked up with diagnostic angiography and intravascular ultrasound5,6 (IVUS) to accurately confirm luminal diameter of the parent artery. Subsequent transfemoral stenting of the hepatic artery was performed with a 5mmx5cm Gore Viabahn endoprosthesis with excellent result on completion angiography and subsequent follow-up CT scanning. Care was taken to ensure continued perfusion of an early hepatic artery branch. The patient remains alive and well with normal liver function one year post-procedure (Figure 1a-1c).
A 55-year old heavy smoker presented with an acutely painful finger with bluish discolorations of the digit. Brachial and radial pulses were diminished but the arm was fully viable. CT angiography demonstrated a ragged moderate-length subclavian stenosis which was the source of distal embolisaiton. Cardiac echo was normal. The patient was treated via an transfemoral approach with a 6mmx10cm Viabahn stent which was gently balloon impacted across the stenosis. Post-implant angiography was satisfactory and the brachial and radial pulses returned to normal. The patient was treated with clopidogrel for six months post-procedure and has not experienced any further embolic phenomenon (Figure 2a-2b).
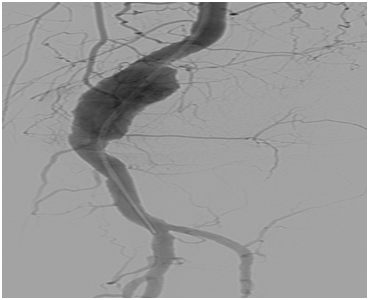
An otherwise fit 72-year-old man presented with left calf swelling. Initial investigations for DVT were negative but clinical examination revealed a Popliteal artery aneurysm. This was confirmed on duplex and subsequent CT angiography. The case was discussed at a multidisciplinary meeting and given the good landing zones in the proximal and distal popliteal artery the patient was put forward for endoluminal stenting. Given the slight tapering of the Popliteal artery a 8mmx5cm Viabahn stent was placed in the distal landing zone followed by a 9mmx10cm Viabahn, overlapped by 2cm and landed in the proximal popliteal. This was accomplished by a transfemoral antegrade approach. The stents were gently balloon impacted into the native artery and into the junctional region with a 9mmx4cm angioplasty balloon. Check angiography was satisfactory and stent expansion was confirmed with IVUS prior to the end of the procedure. The patient is alive and well 6 months post-stenting (Figure 3a-3d).
The excellent results of the Viabahn device in complex fem-pop disease mean it is an established tool in the armamentarium of the vascular interventionist. Given adequate planning, we believe it can also be used with good effect in other arterial sites and pathologies. In particular, the conformability and flexibility of the device, as well as its radiopaque markers mean it can be accurately placed and deployed in challenging situations.
All patients provided express written consent for medical use of images.
None.
The author declares no conflict of interest.

©2017 Montgomery, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.