MOJ
eISSN: 2379-6162


Mini Review Volume 2 Issue 2
1Department of Pediatric Surgery, Astrid Lindgren Children's Hospital, Sweden
2Department of Pediatric Surgery, Landsp
3Department of Pediatric Surgery, Sk
4Institution of Clinical Sciences, Lund University, Sweden
Correspondence: Einar Arnbjornsson, Department of Pediatric Surgery, Skane University Hospital, Lund and Institution of Clinical Sciences, Lund University, Sweden , Tel +46706496380
Received: March 21, 2015 | Published: March 27, 2015
Citation: Gunnarsdóttir A, Stenström P, Arnbjörnsson E. Two ports laparoscopy-assisted colostomy in neonates–a method described. MOJ Surg. 2015;2(2):21-23. DOI: 10.15406/mojs.2015.02.00011
This is a description of the technique used for laparoscopy-assisted colostomy in neonates with anorectal malformations (ARM), using 2 laparoscopic ports only. The technique is easy to use and has the advantages of enabling identification of the sigmoideum, the internal genitals and to establish a stoma leaving only minimal scars in the umbilicus. In our departments, we routinely perform stoma operations using this technique. We do not claim any benefits or disadvantages of LAC compared with the traditional open technique.
Keywords: colostomy, neonates, anorectal malformation (ARM), laparoscopy, laparoscopic colostomy
ARM, anorectal malformations; LAC, laparoscopy-assisted colostomy
Laparoscopy-assisted colostomy for colonic diversion in adults was introduced in 1994.1 In comparison with conventional open creation of colonic stomas in adults, the laparoscopic technique is reported to facilitate earlier return of intestinal function and earlier postoperative food intake, to cause less postoperative pain, and shortens hospital stays.2 There is only a single report on laparoscopic-assisted colostomy in children, in which the surgeons used 2-4laparoscopic ports in addition to the colostomy site.3 Here, we describe our technique for laparoscopy-assisted colostomy (LAC) in neonates with anorectal malformations (ARMs), using only 2laparoscopic ports of which one of them is used for the stoma site.
The child is placed in the supine position on the operating table. General anesthesia is administered and ropivacaine hydrochloride, 2mg per kilogram of body weight, is administered as local anesthesia to the port sites. Metronidazole and cefuroxime are administered as pre-operative antibiotic prophylaxis. The first port to be placed is for the camera. Using open technique, a supra-or subumbilical 3-or 5-mm laparoscopy port is established. The supraumbilical location provides a longer and more favorable distance for inspecting the pelvic floor and the sigmoid colon compared with a subumbilical position. In order to avoid the umbilical vessels in the newborn child, the supraumbilical port can be placed slightly to the right or left of the midline. Insufflation is achieved with a maximum pressure of 8 to1mmHg and a flow rate of 1liter/min. A 30-degree, 3-or 5-mm videoscope is introduced through the supraumbilical port into the peritoneal cavity. The internal organs of the abdomen are inspected, the distal colon is visualized, and an optimal place for the colostomy site on both the colon and the abdominal wall is chosen. Any anomaly of the abdomen or internal genitalia is identified and recorded.
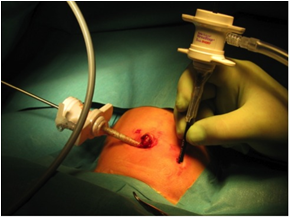
A skin incision is made at the site chosen for the colostomy on the abdominal wall. A second troacar of 5 mm is placed under laparoscopic visualization, and a grasper is introduced through this port (Figure 1). With the help of the grasper and by using varying patient positioning, the abdominal cavity and internal organs can be fully visualized. The internal genitalia can be inspected, in order to secure that both ovaries and uterus are identified and to rule out duplex uterus, single or none ovaries or undescended testes.
The sigmoid colon is then identified, and the optimal colostomy site is chosen on the colon. The bowel is grasped and checked for mobility; it has to be loose enough to enable creation of a stoma and, at the same time, not so mobile as to predispose to postoperative prolapse. In patients with ARM, the distal length of the colon must be secured so that the rectum and anus can be reconstructed at a later time.
The grasper is used to hold the part of the colon chosen for the stoma, which is pulled up to the trocar (Figure 2); the trocar is then withdrawn. The grasper is used to bring the bowel out through the abdominal-port opening. After displacing the marginal artery, the colon is divided outside the abdominal cavity. The effluent is suctioned away to prevent peritoneal contamination. This step decompresses the intestine, giving the neonate enough relief and relaxation for completion of the procedure. The decompression also creates space for further examination of the bowel and other abdominal structures.
In our experience the LAC can be used both for loop colostomy or a divided colostomy which is recommended for infants with ARM. In the case of loop colostomy the abdominal opening is widened as much as needed, and an enterotomy is made in the colon at the anti-mesenteric side for eversion of the bowel folds in a traditional way (Figure 3). In the case of divided colostomy the stomas are established without an incision wound in between (Figure 4). The colon is divided extra corporally after displacing the marginal artery. The divided ends of the sigmoid colon are held with either Babcock tissue forceps or 2 stay sutures, 1 on each end, to prevent the ends from falling back into the abdominal cavity. The distal stoma must be displaced some centimeters distally from the active stoma on the abdominal wall. A small incision is made for the chosen distal stoma site and through the fascia and opened in to the peritoneum. The distal stoma end is fetched with Babcock tissue forceps or with clamps to the stay sutures and taken out through the distal stoma site. Both stomas are then fixed to the abdominal wall using conventional 4-point sutures or 3-point sutures if constructing a mucous fistula only. In patients with ARM the distal stoma end must be displaced to a location some centimeters away on the abdominal wall in order to avoid a spill over into the distal stoma and the recto-urethral or recto-vesical fistula.

A colostomy bag is placed immediately after surgery. The operative time is less than 1hour, and patients are able to take fluids by mouth during the first 24hours after surgery. Up to now 11 children have been operated using the two ports laparoscopy-assisted colostomy. One child was five years of age and the other were neonates. In one child, with cloaca and severe cardiac malformation, the operation was converted due to anesthesia problems when filling the abdomen with CO2 and thereby increasing the intra-abdominal pressure and influencing the cardiac and ventilator output. The diagnostic laparoscopy provided information on the intra-abdominal anatomy and internal genitals of importance for future planning of operative interventions for the child’s cloaca. Further surgery conducting a colostomy was performed with open surgery.
In the group of children a late stricture, after 5months, was noted and treated surgically. There were no prolapses. In one child the operating surgeons misinterpreted the two ends of the bowel. This did not influence the course of the child. In one child a minor postoperative infection occurred which was treated with antibiotics. In all the other children the post-operative course was uneventful.
We describe herein a method for 2-port laparoscopy-assisted colostomy, loop or divided, which now is used routinely at our departments of Pediatric surgery. The LAC can be used as an alternative for standard open surgical colostomy in neonatal children in order to facilitate to assess the direction of colon and enable a good position of the stoma. The technique described improves the positioning of the stoma-both on colon and the abdominal wall - and help to determine the status of internal genitals.
Children born with ARM are the group with the highest frequency of colonic stomas. The standard open procedure in ARM is performed through an oblique gridiron laparotomy incision in the left lower quadrant, and a descending or sigmoid colostomy is made using separate stomas, placing the stomas at each edge of the surgical wound. The distal stoma is recommended to be left as a mucous fistula.4 In LAC enough length of the distal part can be carefully spared, which is important for the later reconstruction of anus. LAC also enables the assessment of inner genitals, which is of special concern in cloaca.5 In a recent report of a 2-port laparoscopic loop colostomy creation, the authors described the use of a minilaparotomy in the left lower quadrant, equally distant from the umbilicus and iliac crest, to help locate the first laparoscopic port. The site of the minilaparotomy in this technique is the location chosen for the proximal stoma for the descending colon.6 The disadvantage with this method is that the stoma placement has to be decided at the beginning of the operation, and thus some flexibility is lost.
The LAC technique allows for excellent visualization of the abdomen and pelvis, even in patients with dilated bowel. Good visualization makes it easier to select the optimal stoma site on the colon, without twisting the bowel or injuring or trapping an intestinal loop. The operating surgeon can ensure that sufficient bowel remains below the colostomy for future anorectal reconstruction in infants with ARMs. Furthermore, the surgeon can evaluate whether the bowel is anchored sufficiently in the abdomen to prevent the development of a postoperative stoma prolapse. The procedure is not technically demanding, and better cosmetic results than those seen with conventional techniques can be expected.
The LAC is as easy to perform as conventional open colostomy. However, as with any surgery there is the possibility of operative errors such as wrongly interpreting the laparoscopic findings, leading to incorrect choosing of the distal or proximal parts of the colon for the stoma. This could also happen in open procedures. The present described laparoscopic procedure, as with all other surgical interventions, may also lead to minor complications such as skin infection and discomfort during management of the colostomy bag after surgery.7–9 Severe wound infection, stoma prolapse, and evisceration can also occur.
In our department, we routinely perform stoma operations using LAC. According to our routine after LAC the children start oral nutrition within 24hours of the operative intervention. We are now collecting a prospective follow-up of all children operated on with the described method at our department. A prospective study and preferably randomized study is necessary to demonstrate the benefits and also possible disadvantages of LAC compared with the traditional open technique.
To BioMed Proofreading LLC for linguistic revision.
The author declares no conflict of interest.

©2015 Gunnarsdóttir, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.