MOJ
eISSN: 2379-6162


Case Report Volume 12 Issue 3
1Colorectal Surgeon Consultant, Private Practice, Covadonga Hospital, México
2Urogynecologist Consultant, Hospital Star Médica, México
Correspondence: Julian Zilli García, Colorectal Surgeon Consultant, Private Practice, Covadonga Hospital, México
Received: August 20, 2024 | Published: September 3, 2024
Citation: García JZ, Morales AB. Transperineal perineoplasty with anal sphincteroplasty: cloacal reconstruction for 4th degree obstetric perineal tear with failed previous repair. MOJ Surg. 2024;12(3):84-88. DOI: 10.15406/mojs.2024.12.00268
We describe the case of a patient with anal sphincter injury and fecal incontinence related to obstetric trauma, who was previously treated in another center with primary repair on 2 occasions and with recurrence of the tear, developing cloacal deformity. Transperineal perineoplasty with sphincter restoration was performed with overlapping technique, with immediate postoperative recovery of fecal continence, and during the 3-year follow-up, fecal continence was maintained.
Keywords: anal sphincteroplasty, fecal incontinence, perineoplasty, 4th degree perineal tear of obstetric origin
Obstetric trauma anal sphincter injuries (OASIs) have an estimated incidence of 3%, doubling to 6% in women with the first delivery,1 and up to 19% of vaginal deliveries may have some degree of anal sphincter tears.2 Fecal incontinence is directly related to the severity of the injury, and may be considered as more serious in 4th degree tears, affecting negatively quality of life, and up to 30% of patients may suffer social abandonment if not surgically corrected.3 There is no standardized treatment for reconstructions in 4th degree tears with fecal incontinence, but it has been proposed that reconstruction with a perineal approach with anal sphincteroplasty corrects the altered anatomy and allows the possibility of recovering fecal continence in more patient affected by obstetric trauma cloaca.4
Case presentation: This is a 28-year-old Mexican female housewife, without any previous medical condition, and no relevant medical history, with a body mass index of 23 kg/m2, G:1 P:1. During her first pregnancy, she was received at a second level hospital, where she had a vaginal delivery with not specified dystocia, so an episiotomy was performed, resulting in a 4th degree perineal tear, which was repaired in the immediate postpartum period, the baby was alive and required no further medical attention, and both were discharged. Four days after the repair, the patient presented with severe pain and mild bleeding in episiotomy wound, and was taken to the operating room for lavage and debridement of the necrotic tissue, where a new repair was attempted, but was unsuccessful Four days after the repair, she presented dehiscence of the episiotomy, and was taken to the operating room for washing and debridement of necrotic tissue, where a new repair was attempted, which was unsuccessful. She was referred to the service of Coloproctology and Urogynaecology for episiotomy tear evaluation.
During the physical examination a rectovaginal cloaca was identified in upper third of the vagina, with solution of continuity in both anal sphincters. By bimanual examination, the absence of rectovaginal septum was corroborated by palpation of the explorer's fingers of both hands directly, proximal to the fórnix; and both anal sphincteric donuts disrupted, with marked loss tone at rest and active contraction. Neither anorectal manometry nor endoanal ultrasonography were available in the department at the time of the patient's evaluation. Therefore, Under these conditions, overlapping perineal and sphincter repair is suggested for the patient.
Surgical technique: In lithotomy position and under epidural analgesia and with bladder catheterization, the area is cleaned with 7.5% foam iodopovidone solution and isolation of the surgical field with sterile fields. Four traction stitches with 2-0 silk are placed on the edges of the remaining anal margin and then four additional stitches with 2-0 silk are placed for lateral traction of the vaginal introitus. Using electrocautery, skin and subcutaneous tissue are dissected from the anal margin to the external anal sphincter fibers on both sides (Figure 1), and referred with 2-0 poliglactin suture. Dissect the vaginal lining at least 2 cm on either side of the dehiscence, proximal to the cervix, and continue to the hymenal fold. The rectal mucosa and longitudinal rectal musculature are dissected en bloc, with a 2-0 chromic catgut suture placed across the rectal mucosa and its longitudinal rectal fibers (Figure 2), starting cephalad at the apex of the rectal defect and continuing the closure proximal to the internal anal sphincter. The remaining fascial fibers of the elevator plate are then overlapped using interrupted 2-0 polyglactin 910 sutures, checking that the tissue is free of tension and ischemia ((Figure 3). Overlap the remaining fibers of the internal anal sphincter with 3-0 Polyglactin 910 for the anal sphincter and 2-0 for the external anal sphincter (Figure 4), then approach the perineal muscles with separate sutures (Figure 5). A continuous 2-0 catgut suture should be applied to the vaginal mucosa proximal to the fornix and continued to the hymenal orifice, approaching the hypodermis (Figure 6). A latex sheet half an inch wide and 4 cm long is placed at the level of the perineal body, and a second sheet with the same characteristics is placed in the dead space created in the neoseptum. The skin is sutured with 3-0 chromic suture. Operative time: 3 hours 30 minutes, transoperative bleeding: 250ml.
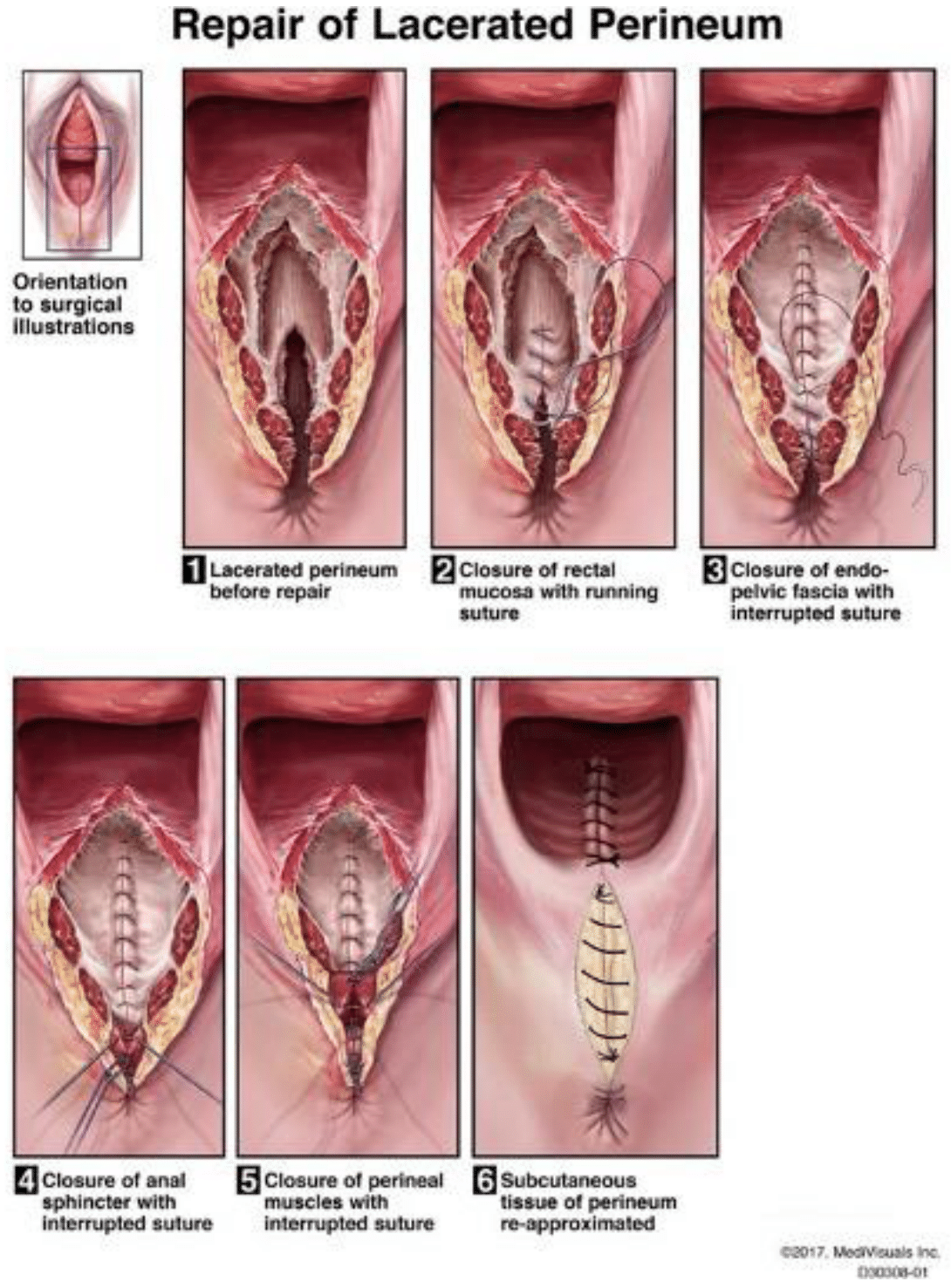
Figure 1 Lacerated perineum before repair.
Figure 2 Closure of rectal mucosa with running suture.
Figure 3 Closure of endo-pelvic fascia with interrupted suture.
Figure 4 Closure of anal sphincter with interrupted suture.
Figure 5 Closure of perineal muscles with interrupted suture.
Figure 6 Subcutaneous tissue of perineum re-approximated.
Principles of perineal tear reconstruction. Identify the extent of the laceration proximally and distally (Figure 1). Close the mucosa and rectal wall en bloc with continuous suture (Figure 2s). After identification of the endopelvic fascia, an additional layer of continuous suture is applied (Figure 3). Reconstruction of the external anal sphincter is recommended by overlap and with 3 to 4 separate stitches of absorbable suture (Figure 4). Identifying the fascial layer of perineal muscle facilitates closure (Figure 5). The subcutaneous layer is closed with absorbable sutures. This is recommended to avoid early dehiscence (Figure 6) 2017, MediVisuals Inc. D303 08-01 (Figure 7-9).
Reconstruction of distal third of the vagina and perineal body and repair of the anal sphincter with overlap technique, a penrose drain is left in place. The patient started a diet the day after surgery, recovered without immediate complications and was discharged 48 hours after the described procedure. Acetaminophen 500 mg orally every 6 hours for 7 days and metronidazole 500 mg orally every 12 hours for 7 days, with dressing changes if necessary. The wound was observed to be clean and with little edema of the soft tissues during the first check-up at 7 days. Drainage latex sheet drops spontaneously after 10 days, and the patient is trained to perform Kegel exercises for a 10 minute period 6 times a day for 4 months, since there is no biofeedback biomedical equipment available. After 3 years of postoperative follow-up, she has had no incidents of fecal incontinence as assessed by the Wexner score at office visits, but she did mention occasional episodes of dyspareunia during the menstrual cycle.
Up to 19% of women with some degree of OASIS have some degree of fecal incontinence, and up to 13% of asymptomatic women have ultrasound-detectable muscle tears. Despite primary OASIS surgical repairs, up to 55% of women persist with sphincteric muscle defects, and 38% of women with surgical repairs have some degree of fecal incontinence.5 Up to 46% of women with OASIS and fecal incontinence report significant deterioration in their quality of life, presenting as early as immediate postpartum and increasing over time.6 2008 females Where evaluated with OASIS, 245 (12.2%) had a 4th degree tear, and women with 4th degree tears in the first pregnancy are reported to have up to 30% risk of permanent fecal incontinence.7 In a meta-analysis with high heterogeneity, the effectiveness of the overlap technique versus terminal end to end was evaluated, finding that there were no differences in perineal pain (RR) 0.08, 95% confidence interval (CI) 0.00 to 1.45, dyspareunia RR 0.77, 95% CI 0.48 to 1.24, and flatus incontinence RR 1.14, 95% CI 0.58 to 2. 23, at 12 months after repair, but there were statistically significant differences with the overlap technique in terms of lower fecal urgency RR 0.12, 95% CI 0.02 to 0.86, anal incontinence standardised mean difference (SMD) -0.70, 95% CI -1.26 to -0.14, as well as a lower rate of deterioration of fecal continence at 12 months RR 0.26, 95% CI 0.09 to 0.79, although there was no statistically significant difference in quality of life.8 In a follow-up report of 29 patients who underwent overlap sphincteroplasty to correct cloacal deformities, an adequate quality of life was observed during the entire follow-up period, and it was reported that 53.8% of the patients had complete fecal continence at the end of the study with this technique, and with little perioperative morbidity.9 Non-flap surgery has been reported as a useful alternative for repairs of obstetric defects affecting both the vaginal wall and the sphincteric complex, with complete fecal continence up to 24 months after reconstruction.11 In a series of 26 cases of women with obstetric cloaca undergoing perineal body repair and sphincteroplasty, the median fecal incontinence score with Wexner scale preoperatively was 16 points, and postoperatively decreased to 2 points, the median resting anal pressure increased from 9.0 (5.25 - 11.50) mmHg (p<0.01), and increased median voluntary anal pressure to 110.0 (96.2 - 121.50) mmHg (p<0. 01) at 2 months after reconstruction, measured by anorectal manometry, and also improved quality of life score scale after 1 year of follow-up (3.10 [2.60-3.70] vs. 2.60 [1.90-3.00], P<0. 01), improvement in coping with illness (3.38 [2.57-3.44] vs. 2.33 [1.89-3.00], P < 0.01), decrease in depression and improvement in self-perception (3, 11 [2.27-3.44] vs. 2.33 [1.89-3.00], p < 0.01), and decreased feelings of shame (3.33 [2.75-3.67] vs. 2.33 [2.33-3.00], p < 0.01).11 Wang et al. performed a retrospective analysis of the outcomes of 20 women with OASIS operated on with a modification of perineal reconstruction with anal sphincter repair, had a mean Wexner score of 9 for fecal incontinence, which decreased to 1. 35 at 30 days and 0.20 at 6 months (p<0.001), and peak resting pressures had a mean of 34.05 before surgery versus 59.90 mmHg at 6 months after surgery (p<0.001).12 In a cohort study of 363 women where 125 had complete anal sphincter tears and 238 had no identifiable tear, an increased risk for fecal incontinence was observed in the group exposed to the complete tear with a 50% increase for fecal incontinence RR 2 (1.52 - 2.63 CI: 95%) in the long term.13 Transperineal 4D ultrasound is considered a useful tool in the follow-up of patients with OASIS repair, as a group of 140 women were retrospectively followed for 2 months after primary repair after delivery, and it was identified that 20%(28) of the patients had 4th degree tears and 16%(23) had unclassified 3rd degree tears, and 25%(35) of the total study population had symptoms of fecal incontinence. Residual defects were found in 40% of the cases and elevator avulsion in 16% (p=0.03; OR= 6.38; 95%CI 1.23 - 33.0), which were considered independent risk factors for fecal incontinence without reaching statistical significance (p=0.047; OR = 4.38; 95% CI, 1.02 - 18.77).14 In 1948 Arnold Kegel described specific pelvic muscle exercise routine that was later found to be effective in strengthening the perineal musculature by direct manometry using a perineometer tool.15 A randomized, controlled study analyzed 150 female patients with fecal incontinence evaluated with anorectal manometry and endorectal ultrasound to determine quality of life and functional status. Patients were randomized into 5 groups in a randomized manner: Kegel (control), kegel with electrostimulation, Kegel with biofeedback, and neuromodulation + Kegel, where all groups received treatment and reevaluation for 3 months, and were followed up for 6 months after completion of treatment. Severity of FI and QoL were similarly significantly improved after all treatments. The effect on physiology was treatment-specific: Kegel and electrostimulation + Kegel increased resting pressure (P < 0.05). Squeeze pressures increased significantly with biofeedback + Kegel, electrostimulation + Kegel, and neuromodulation + Kegel (P < 0.01). Squeeze endurance increased with biofeedback + Kegel and electrostimulation + Kegel (P < 0.01). Rectal perception threshold was reduced in biofeedback + Kegel, electrostimulation + Kegel, and neuromodulation + Kegel (P < 0.05); latency of anal sensory evoked potentials was shortened in patients with electrostimulation + Kegel (P < 0.05). They reported selection bias in control group.16
Surgery for reconstruction of 4th degree OASIS defects with failed repairs and associated fecal incontinence can be performed through the transperineal approach, where absolute knowledge of the surgical anatomy of the defects as well as repair with overlapping technique and layered closure can be performed as a measure to improve quality of life and decrease morbidity related to this type of tears. Quality of life improves significantly after successful repair, regardless of the severity of the injury. Kegel exercises can improve pelvic sensation and contractility, even in the absence of adjunctive electrostimulation devices in the treatment of fecal incontinence. A multidisciplinary team is essential to obtain an objective assessment of the severity of the injury and its impact on pelvic floor physiology.
None.
The authors declare no conflicts of interest.

©2024 García, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.