MOJ
eISSN: 2379-6162


Case Report Volume 8 Issue 2
Department of Surgery, Albaha University, Saudi Arabia
Correspondence: Alzahrani Rajab A, MD, Assistant Professor, Division of Otolaryngology, Department of Surgery, Faculty of Medicine, Albaha University, Saudi Arabia, Tel 966509766298
Received: April 16, 2020 | Published: May 6, 2020
Citation: Alzahrani RA. Subcutaneous emphysema after tonsillectomy: a case report and literature review.MedCrave Online J Surg. 2020;8(2):27-30. DOI: 10.15406/mojs.2020.08.00166
Tonsillectomy is one of the most commonly performed surgical procedures among patients in the Otolaryngology Department for different indications. Although it is a relatively safe surgical procedure, tonsillectomy may be accompanied by rare complications, such as surgical emphysema, which is considered a fatal complication if incorrectly managed or misdiagnosed. We report a case of surgical emphysema following a routine tonsillectomy, as well as conduct a retrospective review of every such case published in English between January (1, 2000 to March 30, 2020). The aim of this case report was to report the pathogenesis, clinical presentation, treatment and management outcomes of patients with surgical emphysema after tonsillectomy.
Keywords: tonsillectomy, complications, surgical emphysema, patients, tracheostomy
Tonsillectomy is among the most frequently applied operations in patients who visited the Otolaryngology Department. Although tonsillectomy can potentially often involve complications such as nausea, vomiting, throat infection, odynophagia, otalgia, damage to teeth and hemorrhage, it is a comparatively safe operation.1 Unusual complications can also occur;2 for example, surgical emphysema, which is regarded as a life-threatening complication in certain cases. However, most cases followed a benign course and were managed with conservative treatment. Herein, we report a case of surgical emphysema following routine tonsillectomy. The aim of this review is to report the clinical presentation, pathogenesis and management outcomes of patients who developed post-tonsillectomy emphysema.
Case report
Our ENT clinic at Saudi German Hospital received a patient who had endured a record number of acute tonsillitis attacks. We examined this 40-year-old female and found red swollen tonsils. The diagnosis confirmed that she was suffering from chronic tonsillitis. Preoperative examinations including laboratory investigations and electrocardiography were normal; therefore, the patient was admitted and a tonsillectomy was performed under general anesthesia, which was induced by protocol and maintained by sevoflurane. Monopolar electrocautery dissection was used to remove the tonsils and hemostasis was attained through bipolar cautery. The operation was uneventful, and the patient recovered promptly from anesthesia, without vigorous coughing or violent neck movement; however, she began to complain of left painful submandibular swelling six hours following the operation. A marked crepitus was detected and a visible pulsation was seen on oral examination; this conformed surgical emphysema, which extended from the mandibular angle to the left side of the upper area of the neck. The patient was regularly monitored and her condition was found to be good, with minimal signs of airway compromise in the first 24 hours which then improved gradually. Computed tomography angiography of the neck was performed (Figure 1) and a small collection of serous fluid was discovered on the left operative bed, as well as marked surgical emphysema on the left side of the neck that reached superiorly to the skull base level and inferiorly to the upper mediastinum. The chest radiograph results were normal without any indication of pneumomediastinum or pneumothorax. Immediately subsequent to this diagnosis, a pressure dressing, high flow oxygen and further intravenous antibiotics were administered to the patient including Augmentin and Flagyl, steroid was not given. The patient showed significant improvement and exhibited a noticeable reduction in swelling after four days. Furthermore, to assess the pharyngeal wall, a gastrografin swallow was performed, which showed no fistulous tracts or contrast leakage. A follow-up computed tomography of the neck (Figure 2) indicated a significant reduction in the volumes of the previously observed fluid and air locules. The patient was monitored at the hospital for an additional four days, and then discharged in a generally good condition.
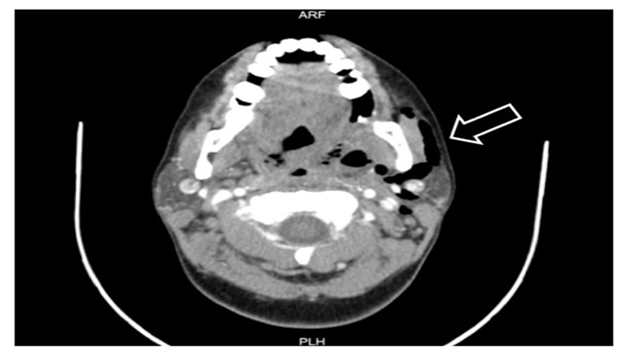
Figure 1 Computed tomography of the neck reveals subcutaneous emphysema. The arrow indicates the presence of air in the left side of the neck.
Literature review and data extraction
The MEDLINE database was searched from January 1, 2000 to March 30, 2020 using the key words “emphysema”, “tonsillectomy” and “adenotonsillectomy”. The search strategy aimed to identify all reported cases of emphysema following tonsillectomy published in English. The search identified 34 articles for review, which were sequentially reduced to 26 (Figure 3). Specifically, information regarding age, sex, surgical technique, time of onset and treatment course was gathered.
Over the past 18 years, 26 cases of post-tonsillectomy surgical emphysema were identified and summarized (Table 1). An additional case from our institution was included, bringing the total number of reported cases to 27. Thirteen of these cases were males and 14 were females, with an average age of 30.5 years (range, 3-55 years). Tonsillectomy was performed by the electrodissection method in 12 cases and by the cold dissection method in 10 cases. The surgical technique used in the remaining 4 cases was not documented. Concurrent adenoidectomy was performed on 8 patients.7,11,21,25,28 The indication of surgery was recurrent tonsillitis in 20 patients. One patient had a granular tumor over the right tonsil with a bulging surface on the nasopharynx and was scheduled for a tonsillectomy and nasopharyngeal biopsy.17 Furthermore, one patient was a down syndrome,3 one young patient was shown to have a significant medical history of attention deficit disorder and seizure disorder.25 The time of symptom presentation ranged from prior to extubation to four days following surgery, and 20 patients (the majority) developed symptoms in the 24 hours following surgery. Generally, a physical examination combined with a CT scan and/or X-ray was used for diagnosis. However, in three cases, the diagnosis was verified exclusively by physical examination.14,17,18 Overall, all patients attained total remission after treatment. In most cases, including our case, the subcutaneous emphysema was treated by conventional methods. However, tracheostomy was required in one complicated case in which the emphysema compromised the airway.18
|
No |
Age (y) |
Gender |
Technique |
Indication |
Time to SE presentation |
Diagnosis |
Treatment |
Country |
Year |
Author |
|
1 |
3 |
M |
bovie electrocautery |
RT, OSA |
Recovery room (1hour) |
Xray |
conservative |
USA |
2020 |
Jenna H Barenget al3 |
|
2 |
6 |
M |
bipolar diatherm |
RT, OSA |
4 hours |
Xray |
conservative |
Bangladesh |
2019 |
Naha A et al4 |
|
3 |
3 |
M |
Cold dissection |
RT+OSA |
Few hours |
PE, CT |
conservative |
Belgium |
2019 |
L De Coninck et al5 |
|
4 |
30 |
F |
Cold dissection |
RT |
POD#3 |
PE, CT |
Conservative |
UK |
2019 |
Kirsten Shoemaker et al6 |
|
5 |
6 |
M |
Cold dissection with bipolar |
RT. OSA |
I hour |
PE, Xray, CT |
Conservative |
Turkey |
2018 |
Görgülü et al7 |
|
6 |
40 |
F |
Not documented |
RT + Peritonsillar abscess |
POD#1 |
PE, Xray |
Conservative |
UK |
2018 |
Mahmood et al8 |
|
7 |
21 |
M |
Cold dissection with bipolar |
RT |
POD#3 |
PE, CT |
Conservative |
Germany |
2017 |
Saravakos et al9 |
|
8 |
12 |
F |
Harmonic Scalpel |
RT |
15 hours |
PE, Xray, CT |
Conservative |
UK |
2017 |
Crosbie et al10 |
|
9 |
4 |
M |
Cold dissection with bipolar |
RT + OSA |
10 minutes |
PE, Xray |
Conservative |
Turkey |
2016 |
Erol et al11 |
|
10 |
30 |
F |
Monopolar electrocautery |
RT + Tonsillith |
POD#4 |
PE, Xray, CT |
Conservative |
US |
2015 |
Tran et al12 |
|
11 |
18 |
M |
Bipolar diathermy |
Hypertrophied tonsils + Dysphagia |
36 hours |
PE, Xray |
Conservative |
UK |
2014 |
Yelnoorkar et al13 |
|
12 |
29 |
F |
Bipolar scissors |
RT |
14 hours |
PE |
Conservative |
Finland |
2014 |
Bizaki et al14 |
|
13 |
21 |
F |
Cold dissection with bipolar |
Peritonsillar abscess |
1 hour |
PE, Xray, CT |
Conservative |
Greece |
2013 |
Koukoutsis et al15 |
|
14 |
36 |
F |
Monopolar electrodissection |
RT |
POD#1 |
PE, Xray, CT |
Conservative |
South Korea |
2010 |
Kim et al16 |
|
15 |
37 |
M |
Not documented |
Granular tumour |
Immediately |
PE |
Conservative |
Taiwan |
2009 |
Hung et al17 |
|
16 |
31 |
F |
Cold dissection with bipolar |
Not documented |
Immediately |
PE |
Tracheostomy |
Brazil |
2005 |
Panerari et al18 |
|
17 |
31 |
M |
Bipolar diathermy |
RT |
6 hours |
PE, Xray |
Conservative |
UK |
2005 |
Patel et al19 |
|
18 |
25 |
M |
Not documented |
RT |
4 hours |
PE, Xray, CT |
Conservative |
Brazil |
2005 |
Lima et al20 |
|
19 |
7 |
F |
Electrodissection |
OSA |
20 minutes |
PE, Xray |
Conservative |
Australia |
2005 |
Shine et al21 |
|
20 |
36 |
M |
Cold dissection |
RT |
POD#4 |
PE, Xray, CT |
Conservative |
Canada |
2004 |
Yammine et al22 |
|
21 |
22 |
F |
Electrodissection |
RT |
Immediately |
PE, Xray |
Conservative |
US |
2004 |
Stewart et al23 |
|
22 |
24 |
M |
Not documented |
RT |
POD#1 |
PE, Xray |
Conservative |
Japan |
2004 |
Watanabe et al24 |
|
23 |
21 |
F |
Monopolar cautery/ ABH |
RT |
Immediately |
PE, CT |
Conservative |
US |
2003 |
Fechner et al25 |
|
24 |
34 |
F |
Cold dissection with bipolar |
RT |
5 hours |
PE, Xray, CT |
Conservative |
Italy |
2003 |
Marioni et al26 |
|
25 |
55 |
F |
Not documented |
RT |
8 hours |
PE, Xray, CT |
Conservative |
Japan |
2003 |
Nishino et al27 |
|
26 |
11 |
M |
Cold dissection |
Hypertrophied tonsils |
Immediately |
PE, Xray |
Conservative |
Turkey |
2001 |
Miman et al28 |
Table 1 Summary of all published cases of post tonsillectomy emphysema from 2000–2020
SE, subcutaneous emphysema; RT, recurrent tonsillitis; OSA, obstructive sleep apnea; Y, years; F, female; M, male; POD, post-operative day; PE, physical examination; CT, computed tomography; ABH, argon beam haemostasis
The literature review revels that several complications have occurred with tonsillectomy although it is among the most frequently performed procedures by otolaryngologists and is regarded as a comparatively safe operation. Leong et al2 reported several rare complications of this routine procedure. These complications included intraoperative vascular injury, surgical emphysema, mediastinitis, Eagle syndrome, taste disorder, cervical osteomyelitis and atlantoaxial subluxation. In the case of tonsillectomy leading to subcutaneous emphysema, several hypotheses exist as to the pathogenesis of this condition. Mucosal damage to the pharyngolaryngeal wall due to surgical or anesthetic causes is the first of these. This disturbance enables air to travel through the superior constrictor muscle into the masticator and pharyngeal spaces. Consequently, vomiting, straining and coughing, which involve an increase in upper airway pressure, eases the accumulation of air. Consequently, as result of the anatomical connection between the laryngeal and pharyngeal spaces, this air accumulation may move to the mediastinum [descending route].28 Second, when an excessive increase in intrapulmonary pressure causes the marginal alveoli to rupture, there is precipitation of the pneumomediastinum, which then reaches the neck [ascending route].23 The third theory suggests that the release of gas by organisms or neighboring solutions is liberated into an enclosed space, causing emphysema.29 In this review, the majority of the tonsillectomies were performed using electrodissection methods. Weimert et al30 conducted a randomized control trial comparing the removal of the tonsils by the cold dissection method with selective cauterization versus electrocautery dissection. They concluded that an equivalent or better outcome was found for electrodissection tonsillectomy when compared to cold dissection in terms of efficacy and safety. However, negative aspects such as slower healing and greater pain can occur after electrodissection, which might be associated with this rare complication.
The severity of this complication can range from self-limiting emphysema of the neck to extensive emphysema over the chest with or without respiratory difficulties and may also predispose the patient to mediastinitis and necrotizing fasciitis. Furthermore, the main clinical characteristic of subcutaneous emphysema is crepitus, and air can be detected by chest X-ray or CT scans, which were performed in most of the cases reported in this review. The treatment of subcutaneous emphysema varies according to the level of severity; nevertheless, conventional management was applied in the majority of the cases. During such treatment, the airway and the level of emphysema are carefully monitored for a few days and any activity that leads to upper-airway pressure such as straining, vomiting and coughing should be averted. Furthermore, the administration of analgesia together with wide spectrum antibiotics is performed, and when there is apparent mucosal disruption, the injured mucosa may be sutured to prevent the secondary entrance of bacteria into the emphysematous space as well as to restrict its extension. Rarely, a tracheotomy or even a thoracotomy is required. Panerari et al18 reported a case of a 31-year-old female who needed a tracheostomy as a result of an airway blockage caused by mediastinal and cervical emphysema. After a period of five days, the tracheostomy was removed successfully and the patient attained complete recovery31.
Despite the rarity of this complication in the medical literature, it is important to detect subcutaneous emphysema after tonsillectomy in order to avert unnecessary and excessive treatment. Whereas this complication may be anticipated in the immediate postoperative period or late, indicating the possibility of a patient who is initially asymptomatic presenting many days following surgery. The reason for that is, subsequent to tonsillectomy, dysphagia, odynophagia and swelling are already frequent complaints; therefore, the provider ought to have increased perception, particularly with any mention of crepitus or breathing difficulties. In conclusion, a closer observation and greater perception will help ensure these potential complications do not develop into life-threatening situations.
Dr. Arwa obeid ENT demonstrator for her arrangements and review. Dr. M. Amjad ENT Consultant for scientific review.
The author declares that there is no conflict of interest.
None.

©2020 Alzahrani. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.