MOJ
eISSN: 2379-6162


Case Series Volume 9 Issue 1
1Dept of Human Anatomy & Oral and Maxillofacial Surgery, University of Nairobi, Kenya
2Dept of Oral and Maxillofacial Surgery, University of Nairobi, Kenya
Correspondence: Dr Fawzia Butt, Dept of Human Anatomy & Oral and Maxillofacial Surgery, University of Nairobi, P.O Box 30197 Code 00100 Nairobi, Kenya, Tel +254722703347
Received: January 20, 2021 | Published: February 23, 2021
Citation: Butt FMA, Guthua SW. Reconstruction of midface defect with temporalis myofascial pedicle flap: a review and case series. MOJ Surg. 2021;9(1):15-19. DOI: 10.15406/mojs.2021.09.00186
Temporalis Myofascial pedicle flap is used for mid face defects, a good alternative to free flaps for contemporary surgeons. We present a case series of 7 patients with defects following ablative surgery secondary to oral squamous cell carcinoma. The flap was used to reconstruct the defect of the orbit, buccal mucosa and palate.
Keywords: temporals flap, midface defect, reconstruction, temporalis, myofascial pedicle flap
Temporalis myofascial pedicle flap (TMPF) was first used by Golovine1 more than 100 years ago in 1898 to obliterate dead space after orbital exenteration.1 Fifty years later, Campbell 2 used it to repair maxillary defects and it remains a very reliable regional flap for the reconstruction of the maxillofacial defects.2 In 1976, Fox and Edger-ton first drew attention to the layers of well vascularized fascia and muscle in the temporal region. Their “fan” flap was a composite of periosteum, temporalis muscle and fascia.3 The presence of two independent vascular territories in the temporal region permits separate utilization of muscle or fascia in the elevation of regional flaps. The temporoparietal fascia and overlying skin are supplied by the superficial temporal artery providing thin axial-pattern fascial and fasciocutaneous flaps. The temporalis muscle and its distal peri cranial extension is supplied by deep temporal vessels and is a particularly useful source of tissue where bulk or dynamic function are required in reconstruction.4 The proximity of the oral cavity, palate, oropharynx, and the middle third of the face in addition to the reliable vascular pedicle makes the TMPF valuable for reconstruction.5 Midfacial defects following tumour or trauma involving both skeletal and soft tissue of the palate, orbit and the mucosa can be reconstructed using the TMPF. We present our experience in using this flap for reconstruction for 7 patients with defects of the orbit, palate and buccal mucosa after ablative surgery following resection of squamous cell carcinoma from the affected regions respectively.
All the patients were operated at the School of Dental Sciences-University of Nairobi. Approval was obtained to collect data for this case series from the School and the patients consent was obtained for each case. A total of seven (07) patients were included in the study. Preoperative clinical, radiographical and pathological evaluation was done for each patient. The patients presented with squamous cell carcinoma involving the orbit, buccal mucosa, maxillary alveolar and palatal region. All the patients were in stage III and IV of the TNM classification. According to the histopathological diagnosis, 5 had well differentiated and 2 moderately differentiated oral squamous cell carcinoma. Intraoperative surgical treatment included Orbital exenteration, excision of buccal mucosa and maxillectomy with selective neck dissection. The resulting maxillary defect was Class 2 and 3 according to Brown et al.,6 classification.6 The TMPF was used to cover the orbit and reconstruct the buccal defects after wide excision of the lesion. The oroantral fistula, resulting from the partial maxillectomy was covered using the temporalis muscle flap this helped to separate the maxillary sinus from the oral cavity.
In all cases the resulting, defect was reconstructed using the TMPF at the same time of the ablative surgery. The hemi coronal incision together with a pre auricular extension was used to expose the Temporalis muscle by dissecting in the subgaleal plane, and freeing it from the temporal fossa. Incision of fasciae attachment from the zygomatic arch allowed free rotation of the flap. Depending on the defect the muscle can be divided in half, cranially with respect to its blood supply when less tissue bulk is needed. The Temporal and Frontal branches of the Facial nerve were included when needed in the flap to preserve their integrity. A tunnel was created via the infratemporal fossa using blunt dissection, for passage of the elevated TMPF into the oral cavity to reconstruction the defect. Once the muscle was transposed into the defect it was secured using 3 0 vicryl suture. A drain was inserted into the harvest site after irrigation and a compression dressing applied after skin closure over the temporal area. All patients except for the one with the orbital tumor were on nasogastric tube feeding for 4-5 days to maintain oral hygiene. The patients recovered uneventfully and were discharged on the 7th post-operative day. Radiotherapy started was 4 weeks post-operatively and are on regular follow up Figures 1–3.
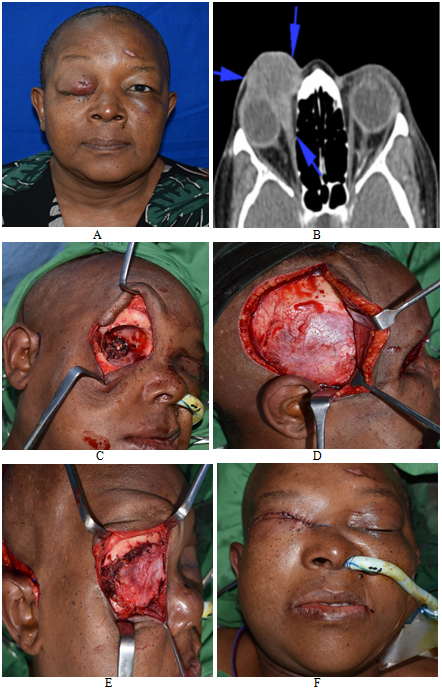
Figure 1 A Extra oral photo showing right orbital tumour causing proptosis and eye closure
B CT Scan highlighting invasion of the eye and surrounding musculature by the lesion causing reduction of the orbital volume leading to eyeball protusion
C Orbital Exenteration done of the right eye showing the bony socket
D A preauricular incision with a temporal extension shows exposure of the temporalis muscle
E Obliteration of the space with flap secured on to frontal bone with sutures
F Flap insitu after skin closure.

Figure 2 A Oral antral defects after maxillectomy via a weber ferguson approach for the midface
B Preauricular Incision marking of the TMFP and the zygomatic bone prior to elevation
C Flap elevation and Temporalis muscle being held by sutures ready to be tunneled
D Intra-oral flap tunneled beneath the arch in to the defect
E Post-operative patient has adequate mouth opening
F Mucolisation seen weeks postoperatively.
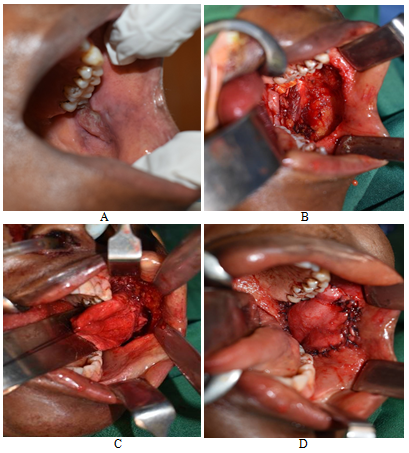
Figure 3 A Right buccal mucosa with infiltrated with squamous cell carcinoma
B Post-operative picture showing the defect after wide resection of the lesion
C Temporalis muscle visible intraorally
D Reconstructed buccal mucosa with the temporalis flap.
There were a total number of seven patients, 4 females and 3 males with an age range 45 to 83 years in the case series Table 1. Factors determining flap viability that were monitored post operatively were its colour, marginal necrosis leading to dehiscence and formation of a fistula. All of our flaps survived with, the intra-oral ones showing mucolisation/epithelization within 3 to 5 weeks. Patients were encouraged on a regular diet postoperatively once the nasogastric tube was removed. We evaluated the patients for complications arising as a resulting from the flap harvest for example trismus, dysphagia, Facial nerve paresis, mastication and temporal hollowing. Apart from one patient who presented with Temporal hollowing, all other patients had an unremarkable recovery. They then proceeded for radiotherapy and are on regular follow up.
NUMBER |
AGE/GENDER |
SITE |
BRODERS |
STAGE |
SURGERY |
FLAP |
CLASIFICATION |
||||||
1 |
78(F) |
LT MAX |
WELL DIFFERENTIATED |
IV |
PALATAL RESECTION |
TEMPORALIS |
Negative Margins |
||||||
2 |
53(F) |
LT CHEEK |
WELL DIFFERENTIATED |
III |
MUCOSAL RESECTION |
TEMPORALIS |
Negative Margins |
||||||
3 |
83(M) |
LT CHEEK |
WELL DIFFERENTIATED |
III |
MUCOSAL RESECTION |
TEMPORALIS |
Negative Margins |
||||||
4 |
49(F) |
ORBIT |
MODERATELY DIFFERENTIATED |
IV |
RESECTION |
TEMPORALIS |
EYELID |
Negative Margins |
|||||
5 |
65(M) |
RT MAX |
WELL DIFFERENTIATED |
III |
PALATAL RESECTION |
TEMPORALIS |
Negative Margins |
||||||
6 |
45(F) |
LT MAX |
WELL DIFFERENTIATED |
IV |
PALATAL RESECTION |
TEMPORALIS |
Negative Margins |
||||||
7 |
52(M) |
LT MAX |
MODERATELY DIFFERENTIATED |
IV |
PALATAL RESECTION |
TEMPORALIS |
Negative Margins |
||||||
Table 1 Case series range from 45 to 83 years
The TMPF is an excellent regional flap with a good outcome, it has a high success rate due to its good vascularity. Literature reports flap necrosis of 1% with success after surgical debridement.7 The largest case series reported by Wang et al.,8 & Browne et al.,6 of 67 and 72 patients respectively reported the continues viability of the TMPF for mid face defect reconstruction.8,9 Our case series is in tandem with these studies showing the excellent versatility of the Temporalis flap for reconstruction of buccal mucosa, closure of oral antral fistula or to cover the defect after orbital exenteration. The close proximity of the Temporalis muscle makes it ideal to reconstruct the inner lining of the buccal mucosa which had been resected as long as the carcinoma has not involved the subcutaneous layer or the skin of the cheek.
Majority of the ablative procedures in the Head and neck region need simultaneous reconstruction and the surgeon has a range of flaps available for reconstruction beginning from local, regional or microvascular.10 The main determinant of the flap is the size of the defect, the distance from the harvest site, and the desired outcome keeping mind the goal is to achieve the functionality and cosmetics as close to the premorbid state.8 Microvascular or free flaps have gained popularity over the local and regional flaps due the advantages of being less bulky and are associated with less donor site morbidity. However, free flaps demand more surgical expertise, an extra surgical team, longer operating time and financial costs on the patient. Existing co-morbidities like cardiovascular conditions or pre radiated patients are not ideal candidates for microvascular anastomosis.8 TMPF on the other hand are easy to harvest, even for the younger surgeon and the operating time is shortened. The patients can be discharged home early. Our patients were kept for a little longer for observation as they had come from rural areas where the hospitals lack specialists. TMP flap has reduced the use of obturators which were in use after a partial maxillectomy, but were cumbersome, difficulty to clean, caused nasal regurgitation of oral feeds and a challenge to use for mastication or phonation for patients. Although, an obturator may still be selected over, surgical reconstruction intentionally as the tumour bed needs to be left open for observation and under these circumstances the patient will have to comply.7
Nasal regurgitation was not a post-operative complication in our patients as the TMPF separated the oral and nasal cavities. The patients were referred to prosthodontic department for occlusal rehabilitation after healing.
Some of the complications associated with harvesting this flap are temporal hollowing, trismus, Alopecia and formation of a fistula, cheek fullness, velopharngeal incompetence and necrotic flap.9,11,12 In our patient the hollowing was not of concern as it was in the hair bearing area which camouflaged it well. As reported by other authors the harvest site is associated with minimal morbidity and healed unremarkably.8,13,14 One of the disadvantages of this flap is the it does not allow the use of Osseo integrated dental implants which would have been an asset especially in the anterior maxilla unlike the free flap.15 The choice of the flap is dependent on the extent of the tumour and the responsibility of the surgeon to restore the both the function and esthetics of the patient to the premorbid state.
TMPF continues to be a versatile flap useful for reconstruction after the ablative head and neck procedures. This regional flap can be used to cover extra oral and intraoral defects and a single surgeon can perform this procedure with ease.
Acknowledgment to all our patients.
We had consent from the patients and Dean and our Chair of Department to proceed with the data collection.
Prof Guthua and I have operated on these patients and have equal contribution in the manuscript preparation.
The authors declare that there are no conflicts of interest.
None.

©2021 Butt, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.