MOJ
eISSN: 2379-6162


Case Report Volume 6 Issue 4
1Department of Head and Neck Surgery, National Cancer Institute, Mexico
2Department of Otolaryngology, University of Antioquia, Colombia
Correspondence: Zaki Antonio Taissoun Aslan, Department of Head and Neck Surgery, National Cancer Institute, Mexico, Tel (+57) 300-8448804
Received: May 20, 2018 | Published: August 3, 2018
Citation: Aslan ZAT, Granados-García M, Luna-Ortiz K, et al. Primary high grade mucoepidermoid carcinoma of skin and cervical lymphatic affection a rare entity. MOJ Surg. 2018;6(1):114-117. DOI: 10.15406/mojs.2018.06.00136
Mucoepidermoid carcinoma is a well documented and described in the salivary glands entity, represents 20-30% of malignant tumors in minor salivary glands and multiple tumors have been reported in head and neck, paranasal sinuses, upper respiratory airways, thyroid, breast, in our experience and based on the literature, its cutaneous presentation is rare and infrequent, but identifiable by pathology and immunohistochemistry not very different from the salivary glands; Prognosis is related to histological grade, clinical outcome.
Keywords: carcinoma, metastasis, mucoepidermoid, skin
Mucoepidermoid carcinoma (MEC) is a well-documented and characterized pathology, being the most common tumor in the major and minor salivary glands. It is present in a 30% of all the malignant pathologies,1 which makes it a non-exclusive pathology of the head and the neck, since it can be present in the thyroid glands, breast and bronchus.2–5
Mucoepidermoid carcinoma (MEC) is referred to as an adenosquamous carcinoma (ASC). However, yet with an undefined terminology, it originates in the sweat glands in tandem with squamous and mucin producing cells, determining the differentiation between these, the histologic grade of the tumor.9
Literature tends to differentiate these two entities, basing itself on the clinic and biologic behavior.10–13 MEC is typically of a lower grade of differentiation, with lesser possibilities of presenting a locoregional or distance disease, while the high-graded ASC is a locoregional or metastatic disease in an important number of reported cases.14 A clinical case of a high-graded MEC with a metastatic locoregional disease is presented. It is treated with surgery and post surgical radiotherapy, monitoring and clinical evolution based on our institutional experience.
We are presenting a clinical case from our files, with an authorized informed consent assessed by the ethical and academic committee of the institution, a 34-year-old male identified as Mexican mestizo, with large exophytic lesion in the posterior triangle of the neck, without significant history. Physical exam: Tumor 10x10cm, exophytic, sessile base, associated with multiple metastases in bilateral neck lymph levels II- V right tumor burden greater than 10cm (Figure 1) (Figure 2). The histopathological report (HPR): poorly differentiated adenocarcinoma mucoproductor. PET/CT reports tumor metabolic activity in posterior triangle of the neck injury dependent and bilateral regional lymph node involvement with subcutaneous cellular tissue.
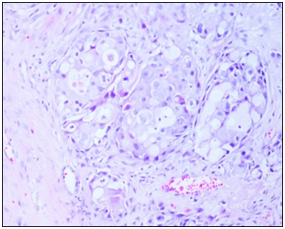
Figure 1 Excisional biopsy review of dermal infiltration poorly differentiated mucinous adenocarcinoma.
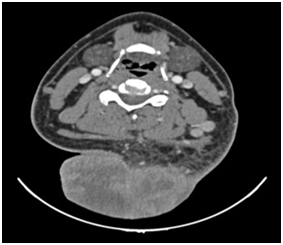
Figure 2 CT Scan, Tumor> 10cm in the posterior cervical region, with affection of subcutaneous tissue.
No discarded tumor activity suggested in lung nodule surveillance (Figure 3). Surgical resection of primary lesion dimensional oncologic margins and partial thickness graft of skin. Cervical treatment was delayed until recovery program (Figure 4) (Figure 5); HPR: high-grade mucoepidermoid carcinoma with vascular lymphatic permeation and extensive areas of necrosis and perineural invasion. Tumor size: 14x10x9cm-free surgical margins of neoplasia; the closest to 2cm, 2.6cm surgical bed to the IHC neoplasia: PAS with and without diastase alcian blue and mucicarmine: Positive for mucin (+++), cytokeratin 7, cytokeratin 8 p.63. Epithelial Membrane antigen: Positive focal (++), cytokeratin 14, cytokeratin 20. TTF -1: Negative (-) (Figure 6) (Figure 7).
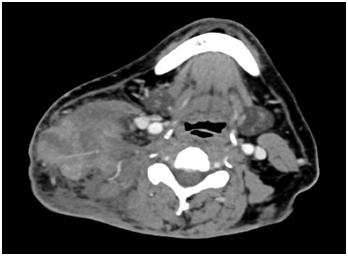
Figure 3 CT Scan, Tumor in the right posterior cervical neck region> 10 cm and tumor mass 14x10x9cms with thrombosis of right internal jugular vein.
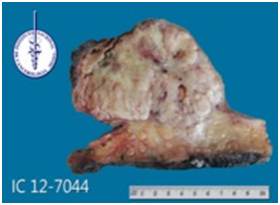
Figure 5B Three-dimensional tumor mass resected with oncological margins. Macroscopic sample. Tumor transected.
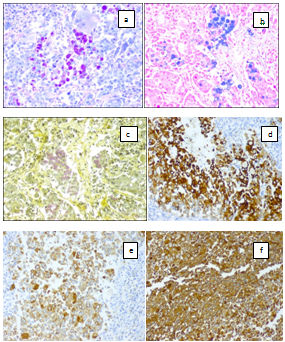
Figure 7 IHC neoplasia : a) PAS with and without diastase, b) alcian blue and , c) mucicarmine : Positive for mucin, d) cytokeratin 7 , e) cytokeratin 8 , f) Epithelial Membrane antigen : Positive, and , cytokeratin 14 , cytokeratin 20 , TTF -1: were Negative.
Subsequently bilateral radical neck dissection is done I–Va/b with subsequent triangles RHP: high-grade mucoepidermoid carcinoma (dermis) and soft-tissue tumor necrosis: 40%, cluster nodes with size: 7.5x6x5cm, lymphovascular permeation and invasion of perineural space, 20/20 lymph lymphoid hyperplasia. Left: lymphadenopathy 5/30 with high-grade mucoepidermoid carcinoma; submandibular glands without evidence of neoplasia. External radiation therapy is applied to cervical region 66 Gy, currently with an overall survival was 48 months, and disease-free survival, 45 months.
The present is a clinical case, an illustrative description of cases when clinical practice faces unusual entities and need to classify them, even when there are no antecedents. The pathology is very well described when it comes to salivary glands with some rare apparitions on the skin. Stewart et al. Reports that MEC is an entity with a diagnosis of histological characteristics based on the inclusion of escamous, basal and intermediate cells, a great number of musin secreting cells and an indistinguishable cellularity when it comes to a complete histological diagnosis.15 Just like MEC, ASC is more prone to appear in areas outside of the skin like the cervix, the pancreas, the lungs, the gastrointestinal tract, the head, as well as the neck.8,16–18
Clinically, the case of a 34-year-old male patient is brought forward. He presents a lesion of <10 cm in the posterior triangle of the neck with cervical bilateral methastasis from the levels II-V. Initially, the pathology reported a poorly differentiated adenocarcinoma mucoproductor. Both the extension studies and the PET/CT show tumor metabolic activity in the posterior neck injury dependent and bilateral regional lymph node involvement with subcutaneous cellular tissue. Consequently, an extensive surgery with optimal oncological margins was done with immediate reconstruction and dissection of the bilateral neck. The definitive report exposes a high-grade tumor, mucoepidermoid (MEC), with preineural and linfovascular invasion. The immunohistochemistry studies show PAS with and without distase alcian blue and mucicarmine: Positive for mucin (+++), cytokeratin 7, cytokeratin 8, p 63, and Epithelial Membrane antigen: Positive focal (++), cytokeratin 14, cytokeratin 20, TTF -1: Negative (-). Due to the rareness of this skin neoplasm, it is necessary to perform a complete physical exam together with imaging tests with high chances of being a metastatic disease in the salivary glands. Additionally, it calls our attention the expression of the p63 with focal positivity. Recent studies suggest that the p63, member of the same genetic family than the p53, is useful in the primary or differential diagnostic of the epidermal or skin adnexal neoplasms, differentiating them from the metastatic tumors.19–21
Recent revision of MEC and ASC, of around 30 cases, show a histological difference between these clinical units (Table 1). However, MEC can appear in the form of a high-grade tumor, unlike what is presented in (Table 1).6 Approximately, 8 of the 30 documented cases were different in their biological behaviors, with high grade histologies, locoregional dissemination, metastasic and death.22,23
|
MEC |
ASC |
Intraepidermal carcinoma |
- |
+ |
Well-differentiated adenocarcinoma |
- |
+ |
Dermal –based solid /cystic tumor |
+ |
- |
Papillary features |
+ |
- |
Mucigenic cell |
++ |
- |
Peritumoral fibrosis |
+ |
- |
High-grade nuclear features |
- |
-/+ |
Table 1 Histological characteristics of the mucoepidermoid carcinoma (MEC) and adenosquamous carcinoma (ASC)
Keyvan N et al. makes reference to the successful use of the mohs micrographic surgery in a high histological grade MEC with 1.5cm margins and to the oncoplastic reconstruction with a global survival rate of 36 months without postoperatoy radiotherapy.24 This sounds almost anecdotic, since a high-grade (MEC) is known to be very aggressive. In our report, we describe the case of a large tumor located in the posterior triangle of the neck with a bilateral locoregional disease and without metastatic disease, present in a 50% of the cases, mainly in the lungs.2 The standard treatment for MEC is a surgery with acceptable oncological margins, with or without dissection of the neck, followed by an oncoplastic reconstruction (if needed). The postoperatory external radiotherapy or intensity-modulated radiotherapy in doses of 60-70 Gy in intermediate graded and high graded tumors,2 with recurrences vary between 30-50 and 12% of the high graded tumors, successively lesser in the low graded ones.10 Our actual experience proves that the global survival rate was of 48 months, currently under monitoring, and the survival rate without the disease is of 45 months.
It is extremely difficult to know which the ideal treatment for MEC is, due to the fact that the published experiences belong to retrospective studies of the tumors in the salivary glands. Plus, in a series of primarily skin MEC cases, we consider that the experience of the institution is key in the curative oncological treatment, based on their experiences and multidisciplinary medical sessions to define a treatment plan.
Mucoepiedermoid skin carcinoma with lymph node metastasis is extremely rare, its clinical Figure depends obviously from the source site, can be classified into low, intermediate, and high grade which is composed of poorly differentiated tumors with mucin secreting cells, cells squamous and intermediate cells. It is generally accepted that the treatment of choice in resectable lesions is surgery with acceptable oncological margins, accompanied by radiotherapy as adjuvant treatment to avoid recurrence and disease control, but also in high-grade tumors, however in the literature currently there is no consensus on the appropriate treatment, based only on case reports and experiences of institutions.
None.
Author declares that there is no conflict of interest.

©2018 Aslan, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.