MOJ
eISSN: 2379-6162


Case Report Volume 12 Issue 2
1Department of Maxillofacial Surgery Hospital of Specialities Rabat, Morocco
2Faculty of Medicine and Pharmacy of Rabat. Mohammed V University in Rabat, Rabat, Morocco
Correspondence: Dr. Rajaa El-Azzouzi, Department of Maxillofacial Surgery Hospital of Specialities; CHU Ibn Sina, Av. Abderrahim Bouabid, BP 1382 RP. 10001, Rabat-Morocco, Tel, Tel +212.664.25.34.99
Received: May 12, 2024 | Published: May 24, 2024
Citation: El-Azzouzi R, Hassene ZAB, Dani B, et al. Phleboliths, not Sialoliths: a submandibular gland venous malformation: case report and literature review. MOJ Surg. 2024;12(2):50-52. DOI: 10.15406/mojs.2024.12.00260
Although venous malformations occurring in the submandibular gland are extremely rare, most have been diagnosed as "hemangiomas". Based on the literature review very few cases of submandibular gland venous malformation were reported for the last 55 years. We provide one of this rare cases; A 62-year-old female patient presented with swelling in the left submandibular area for 6 months with no complaints of xerostomia nor suppuration from the salivary ducts.
Ultrasound Sonography test of the neck and CT scan revealed an heterogenous lesion in left submandibular area with multiple calcifications. The mass was surgically excised, the histopathological examination reported a submandibular gland venous malformation with phleboliths. Low-flow vascular malformations of the head and neck region can develop phleboliths that may be mistaken for sialoliths given the similar calcified nature and location specially in salivary gland area. Appropriate history, clinical examination and investigation leads to the correct diagnosis and treatment.
Keywords: venous malformation, submandibular gland, phleboliths, case report
The understanding of vascular lesions was revolutionized by the classification proposed by Mulliken.1 The vascular lesions can be subdivided into two groups, hemangiomas or vascular malformations depending on the presence of cellular proliferation. Vascular malformations are not proliferative, they grow and never involute spontaneously, we distinguish, venous, lymphatic, arteriovenous and mixed malformations. Venous malformations, although common in the facial region, are rarely seen in the submandibular area. They may present with swelling and discomfort. Imaging with non contrast-enhanced computed tomography scan can reveal multiple calcified densities characteristic of either phleboliths or sialoliths. The present case report is an extremely rare site of venous malformation involving the submandibular gland.
We report a case of 62-year-old female patient, with complaints of a lightly painful swelling covering the left submandibular area, progressively increasing in volume for the past 6 months. The patient had no complaints of xerostomia, suppuration from the salivary ducts, nor fluctuance of the swelling and no associated odynophagia. On examination, a firm, well-defined, mobile, non-pulsatile swelling of size 4.5×3 cm was palpable in the left submandibular region with no overlying skin changes. No lymph node was palpable in the rest of the neck.
Ultrasonography revealed a heteroechoic lesion in the left submandibular region with internal vascularity and multiple macrocalcification within it (Figure 1). Cervico-facial angio-CT scan revealed a lobulated heterogenous lesion in left submandibular area with multiple calcifications, the largest was 9 mm × 9 mm (Figure 2). The diagnosis of venous malformation was evoked and a D-Dimer test was carried out, showing a level of > 530ng/ml. Treatment with heparin was started (Lovenox 1 mg/kg daily).
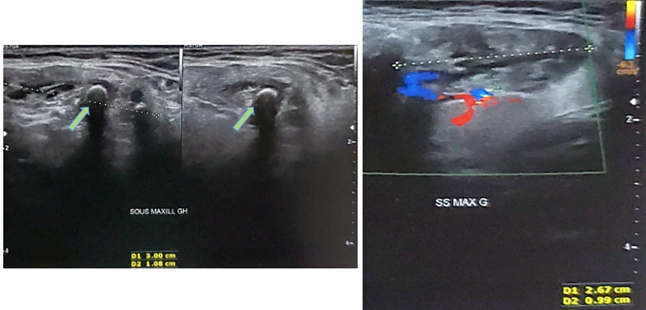
Figure 1 Cervical ultrasound showing left submandibular lesion with shadow cone images of phleboliths mimicking Sialoliths.
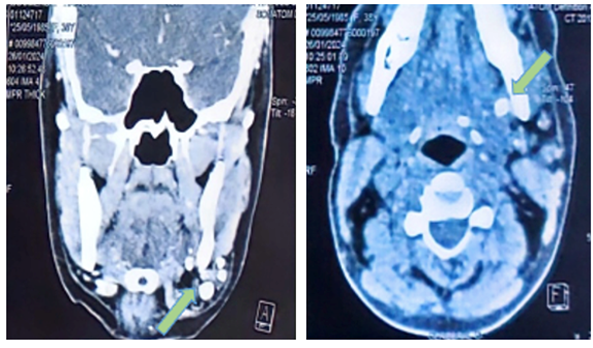
Figure 2 Cervico-facial CT scan in coronal, axial, section showing the left submandibular gland venous malformation with phleboliths.
The decision was made to offer excision of the left submandibular gland via a cervical incision under general anesthesia, the lesion appeared benign with multiple calcifications and dilated vessels (Figure 3). The lingual nerve was identified and protected with delicate dissection. A vacuum suction drain was inserted to prevent haematoma formation and it was removed the following day with minimal drainage. The final anatomopathological result revealed the diagnosis of sub-mandibular venous malformation and multiple phleboliths.
Although venous malformations occurring in the submandibular gland are extremely rare, most have been diagnosed as "hemangiomas". Confusing nomenclature, the relative rarity of these lesions and lack of a multidisciplinary approach are some of the factors leading to ineffective treatment. Slow-flow malformations include capillary, lymphatic and venous malformations where venous malformations is the most common type of vascular malformation, with an incidence of 1 to 2 in 10,000 and a prevalence of 1%.2
Although common in the facial region, are rarely seen in the submandibular area. In general, venous malformation can be silent for years and only revealed in particular situations, when they involve the mucosae or the skin, cause a bluish discoloration, increase in size with local extension or when local intravascular coagulation takes place with phleboliths. Athough phleboliths cause less pain in the head and neck region compared with the extremities.3,4 In the present case, the patient suffered from submandibular pain caused by multiple phleboliths.
Venous malformation usually manifest as a bluish mass of varying size, depressible, and increases in volume when the patient is in the decline position. The evolution may involve: Episodes of thrombosis with painful, inflammatory nodules that regress in a few days, leading to phleboliths, or localized intravascular coagulation: Characterized by pain and an increase in D-dimers.5 Submandibular gland venous malformation has no specific characteristics in clinical examination. However the association of phleboliths may mimic sialoliths. Furthermore an inaccurate diagnosis must be performed based on appropriate history, clinical examination and investigation.
Doppler ultrasound reveals a depressible vascular mass, and sometimes phleboliths. The flow measured within is slow or non-recordable, a Magnetic resonance imaging: Positive diagnosis (T2 hypersignal), CT scan may show heterogenous lesion with variable enhancement depending on rate of blood flow through the vascular malformation.6
Two principal therapeutic options involving, interventional radiology treatment: Sclerotherapy: Percutaneous embolization or surgery. In cervico-facial localization, there are some critical issues to be assessed: The involvement of the skin or the oral mucosa, the proximity to the airways, orbital and midfacial involvement.7 Superficial venous malformations involving the skin are best approached by surgical excision or laser therapy. Deep one settled far from important nerves or vessels can be approached by either surgery or sclerotherapy, in cases with morbid surgical access sclerotherapy is the best option, in deep lesions approximating critical nerves, surgical excision will provide good access and control over sclerotherapy with often unpredictable risk of direct nerve injury.8 Other modalities of treatment may include laser, cryotherapy and corticosteroids.9
Submandibular localization responds best to open excision with submandibulectomy as they often infiltrate the gland and encompass the marginal mandibular nerve. Sclerotherapy for these lesions has a higher risk for permanent nerve injury and recurrence.10 Complications include: Recurrence, especially in the case of sclerosis or partial removal, intraoperative hemorrhage and disseminated intravascular coagulation.
Although venous malformations occurring in the submandibular gland are extremely rare, most of them have been diagnosed as "hemangiomas". Confusing nomenclature, the relative rarity of these lesions, inappropriate diagnosis and lack of a multidisciplinary approach are some of the factors leading to ineffective treatment of these patients.
We express a special thanks to our patient for her cooperation.
The authors received no financial support for the research, authorship, or publication of this article.
Informed consent for publication was obtained from the patient.
The authors declare that there are no conflicts of interest.

©2024 El-Azzouzi, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.