MOJ
eISSN: 2379-6162


Case Report Volume 8 Issue 4
Dept of ENT and Head & Neck Surgery, GMCH, India
Correspondence: Dr. Nitin Gupta, Dept of ENT and Head & Neck Surgery, GMCH, Chandigarh, India
Received: September 13, 2020 | Published: November 16, 2020
Citation: Gupta N, Gulati A, Singhal SK, et al. Migratory foreign body of hypopharynx. MOJ Surg. 2020;8(4):87-89. DOI: 10.15406/mojs.2020.08.00178
A 22-year-old male, tailor by profession presented to Ear Nose Throat (ENT) emergency with accidental ingestion of needle while cleaning his teeth which was associated with difficulty in swallowing (more for solids than liquids) and irritation in throat. On clinical examination no foreign body was seen. Diagnosis of extraluminal migration can be done with the help of Computed tomograms (CT) scans which can provide exact location of foreign body before surgical exploration. C-arm can be utilized specially in metallic foreign bodies to localize during the surgery. In our case both CT and C-Arm were used and foreign body was removed by transcervical route without any complication. In case of absence of foreign body on intraluminal assessment, possibility of migration of foreign body should be completely ruled out and patient should be investigated accordingly.
Keywords: migratory, hypopharynx, ear, nose, throat
ENT, ear nose throat; CT, computed tomograms
A 22-year-old male, tailor by profession presented to Ear Nose Throat (ENT) emergency with accidental ingestion of needle three days back while cleaning his teeth which was associated with difficulty in swallowing (more for solids than liquids) and irritation in throat. There was no complaint of difficulty in breathing, cough, fever, neck swelling or any other complaints. Examination of oral cavity including palpation of the tonsillar fossa did not reveal presence of any foreign body. On indirect laryngoscopy, there was no pooling of secretions in bilateral pyriform sinuses and no foreign body was visualized. X-ray soft tissue neck (anteroposterior and lateral views) showed presence of radio-opaque sharp elongated foreign body lying horizontally in the pre-vertebral region on right side Figure 1. Due to metallic and sharp nature of the foreign body, a non-contrast CT scan of neck was done to find out exact location of the foreign body and it showed presence of foreign body in right prevertebral region, at the level of junction of third and fourth cervical vertebrae Figure 2. After taking informed and written consent patient was planned for endoscopic removal of foreign body under general anesthesia. Direct laryngoscopy revealed a normal endolarynx, pyriform sinuses, and cervical oesophagus. There was no mucosal breach and foreign body or its edge was not visualized.
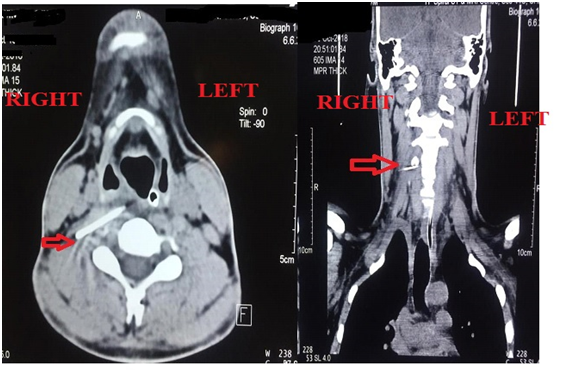
Figure 2 Non contrast computed tomogram (axial and coronal section) of neck showing foreign body in prevertebral area (red arrow).
So, decision was made for surgical exploration via transcervical approach. Patient was positioned with neck extended with face turned towards opposite side (left side). Incision was made two finger breadths below the angle of mandible. After raising subplatysmal flaps, the ipsilateral strap muscles were retracted medially and sternocleidomastoid was retracted laterally. After identifying trachea and esophagus medially and major vessels laterally, dissection was carried out in paracarotid region. Prevertebral fascia was dissected and no foreign body was seen. C-arm was used to localize the foreign body and edge of the foreign body (needle) was visualized with the help of C- arm Figures 3 & 4. Needle was removed after grasping with forceps. Negative suction drain no. 14 was put and fixed. Wound was closed in 2 layers. Immediate post-operative period was uneventful. Nasogastric tube removal and drain removal were done on post-operative day 3. On post-operative day 7, complete suture removal was done. Patient was discharged in stable condition after suture removal. Patient was prescribed oral antibiotic (Tab. Amoxyclav 625 mg TDS for 7 days), C. omez 20 mg OD and Tab. voveran 50 mg sos. Patient was followed up after 7 days and was normal with no fresh complaints. Neck wound was healthy.
Foreign body ingestion is a common complaint encountered by Otorhinolaryngologists. Foreign body ingestion is a common problem that is more commonly seen in children aged 6 months to 3 years of age. Most foreign bodies (80%) pass naturally through the gastrointestinal tract but 10-20% may need endoscopic intervention and 1% or less require surgery.1 In adults, foreign bodies are usually accidentally ingested together with food. Foreign bodies tend to get lodged in tonsil, base of tongue, vallecula, posterior pharyngeal wall, pyriform sinus and oesophagus.2 In adults, accidental swallowing commonly involves fish bone, chicken bone, dentures or toothpicks.3 Migration of a foreign body from hypopharynx to subcutaneous tissue of neck is a rare event.4,5 Patients with foreign body ingestion present with history of initial choking or gagging. Other symptoms include discomfort or pain, dysphagia, drooling of saliva and/or respiratory distress.6 Clinical signs include tenderness in neck, pooling of secretions in pyriform sinus on indirect laryngoscopy. Diagnosis of foreign body can be made on the basis of detailed clinical examination, X-ray soft tissue neck and CT scan of neck.7 In majority of cases, foreign bodies pass through the gastrointestinal tract spontaneously, in about 10-20% cases, endoscopic intervention may be required whereas in about 1% cases, surgical exploration may be needed.1 Extraluminal migration of ingested foreign bodies is seen rarely. The most common site at which a foreign body can perforate esophagus is the cricopharynx which is the narrowest part of the esophagus.8 Migration of foreign bodies is thought to occur due to strong muscular contractions and is possibly related to orientation of foreign body with respect to esophagus.
In our case the possible reason may have been the sharp nature and horizontal orientation of the foreign body which by means of oesophageal contractions got pushed into the neck and as the patient presented after three days so there were no signs of intraluminal injury. Patients with migrated foreign bodies can present with persistent pain, neck swelling, fever, respiratory distress, or hemoptysis.8 Migration from esophagus most often leads to mediastinitis, peritonitis, pneumothorax, pneumomediastinitis, or pneumonia.4,8 Rarely, foreign body may penetrate into aorta which may lead to aortoenteric fistula, a complication with high mortality rate.9 A CT scan provides detailed information regarding accurate size, site, orientation of foreign body which is helpful in planning for neck exploration. However, sometimes during surgery, the foreign body may not be situated exactly at the site as seen in CT due to the mobility of soft tissues of neck. In such cases, intraoperative use of the C-arm can be helpful.10 Removal of foreign body can be done via endoscopic or open approach or combined approach. Open approaches include transcervical approach and transthoracic approach. Migrated foreign body involving major vessels may also require involvement of cardiothoracic and vascular surgeon. Therefore, a multimodality approach is required while dealing with ingested foreign bodies. The above-mentioned case is an example of migration of the foreign body from hypopharynx to soft tissue of neck. In case of foreign bodies prone to migration, especially sharp foreign bodies, an absence of intraluminal foreign body on endoscopy necessitates a CT scan for determination of exact location of ingested foreign bodies. Extraluminal foreign bodies in neck can be removed via transcervical approach. Similar transcervical approach was used by Shaariyah MM et al.,4 and Divya GM et al.,10 for removal of migrated foreign body in to the neck.4,10
We conclude that careful assessment of the patient with a foreign body in throat is crucial to avoid any fatal complications. Extraluminal migration of foreign body can be diagnosed accurately with the help of computed tomogram. C-arm can be utilized specially in migrated metallic foreign bodies for accurate localization. In case of absence of foreign body on intraluminal assessment and strong suspicion of foreign body ingestion, possibility of migration of foreign body should be completely ruled out and patient should be investigated accordingly.
None.
None of the authors declares conflicts of interest.
None.

©2020 Gupta, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.